69 The Importance of Tri-Modality Therapy for De Novo Stage IV Invasive Lobular Carcinoma (ILC) Presenting With Bone-Only Metastases
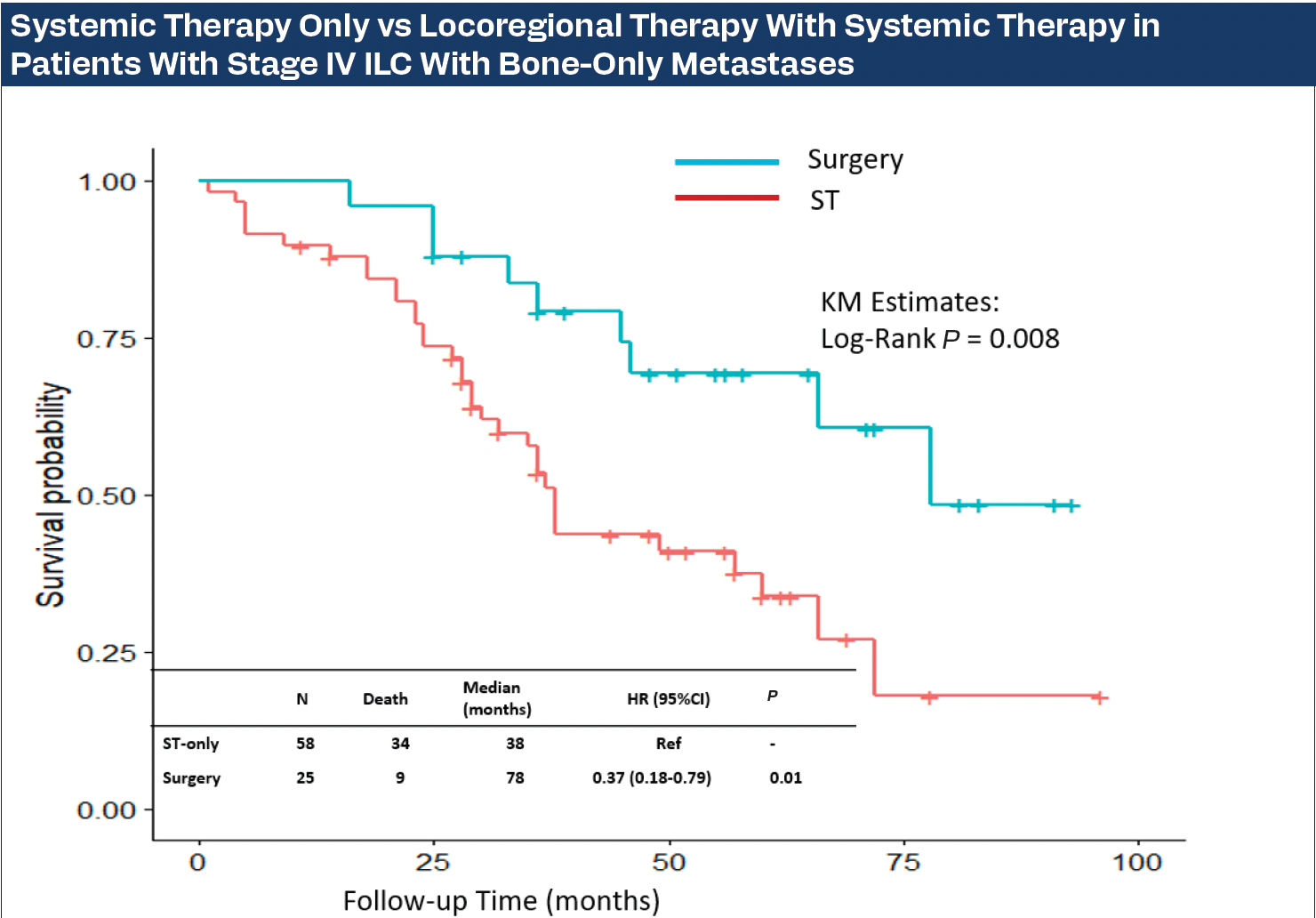
Systemic Therapy Only vs Locoregional Therapy With Systemic Therapy in Patients With Stage IV ILC With Bone-Only Metastases
Background
Locoregional therapy (LRT) of the primary breast carcinoma (BC) in the setting of de novo oligometastatic stage IV disease is strongly debated, despite both retrospective data and prospective trials supporting it. This study aims to determine the overall survival (OS) benefit of LRT combined with systemic therapy (ST) vs ST only in the management of invasive lobular carcinoma (ILC) presenting with de novo stage IV bone-only metastases.
Methods
Patients who presented from 2014 to 2022 with bone-only metastases were retrospectively identified from a prospectively maintained multi-institutional cohort of patients with oligometastases. Univariable and multivariable Cox proportional hazards models were used to identify factors associated with OS. The Kaplan-Meier method was used to estimate time-to-event outcomes. Groups were compared using the log-rank test. Variables included demographics, tumor size, histology, receptor status, use of endocrine therapy, chemotherapy, bisphosphonates, and ovarian suppression.
Results
Of 744 patients identified, 83 (11%) had ILC. Patients with ILC were older (58.9 years vs 52.6 years; P < .05), had a higher number of multiple tumors (81% vs 61%; P < .05), and had lower HER2-positive frequency (12% vs 29%; P < .05) than those with IDC. Hazard of death was 63% higher in ILC vs IDC (HR, 1.63; 95% CI, 1.1-2.24; P = .003). Median OS was 69 months and 49 months in IDC and ILC, respectively. For patients with ILC, baseline characteristics of age, body mass index, T stage, hormone receptor status, ST, and intervention to metastatic sites did not differ between those who had LRT plus ST (n = 25; 30%) vs ST only (P > .05). At a median follow-up of 36 months (IQR, 26-57), 48% (n = 40) of patients with ILC had died. In the ILC group, Kaplan-Meier OS estimates demonstrated longer OS among patients who underwent LRT+ST (median 78 months) vs 38 months with ST only, log-rank P = .008; Figure). Hazard of death was 63% lower with LRT+ST vs ST only (HR, 0.37; 95% CI, 0.18-0.79; P = .01). LRT plus ST was the only factor contributing to OS at 36 months (OR, 3.64; 95% CI, 1.33-11.20; P = .02).
Conclusion
Patients with ILC and de novo bone-only metastases have a worse prognosis compared to those with IDC, but those who have LRT plus ST have a better OS than those who receive ST only. While there may be selection biases in our multi-institutional retrospective cohort, patients with ILC should be considered for LRT for the primary tumor combined with ST.
