63 Choice Architecture Bias in Genetic Counseling of Breast Cancer Patients
Background
American Society of Breast Surgeons (ASBrS) consensus guidelines recommend genetic testing be available to all patients with a personal history of breast cancer, with the National Comprehensive Cancer Network allowing for multigene panel testing beyond the most common pathogenic variants of breast cancer. Genetic counseling is typically provided by breast surgeons or genetic counselors. However, there are no formal recommendations for the breadth of genes to be tested.
The ASBrS asserts genetic testing should occur in the context of informed consent. In this context, the breadth of genetic testing should be decided by the patient following pretest counseling.
Choice architecture posits that decisions are influenced by how choices are presented. Depending on the bias of the choice architect, be it surgeon or genetic counselor, there may be differences in the size of panels ordered for which there should be none.
Methods
Breast surgeons (n = 4) and genetic counselors (n = 5) with more than 50 genetic test orders among the breast cancer population within a 7-hospital system were audited over a 3-year period (n = 3912 tests). The median number of genes ordered was used to create order categories: less than median vs at least median. Chi-square analyses were used to compare the relationships between order category and clinician as well as order category and clinician’s role.
Results
Genetic Tests Ordered by Breast Surgeons and Genetic Counselors
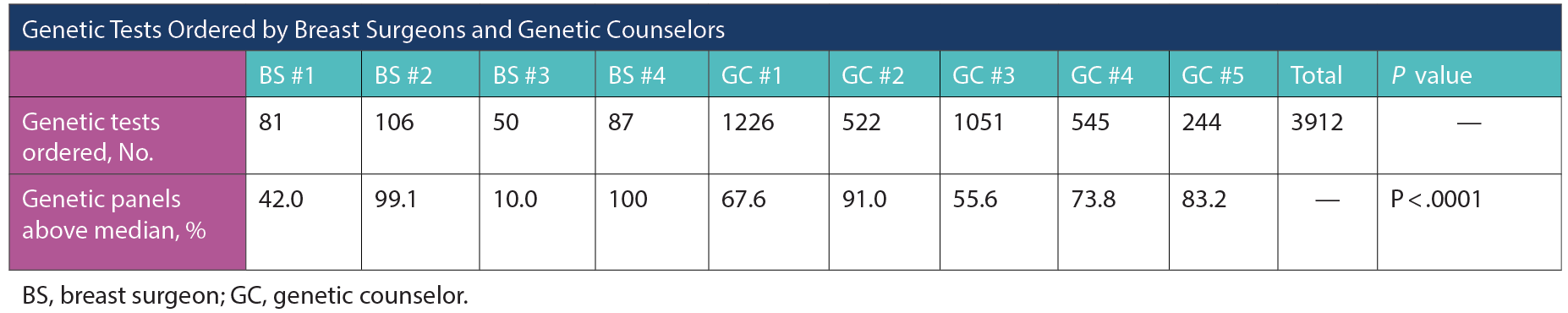
The median number of genes tested was 48 (IQR, 32-85). There were significant differences in the proportion of orders above the median among the 4 breast surgeons (P < .001) as well as among the 5 genetic counselors (P < .001). In contrast, there was no difference in the proportion of orders above the median between the 2 clinician groups (P = .50).
Discussion
These data lack propensity-matching of the breast cancer populations, yet there is significant anchoring in 5 of 9 clinicians, where greater than 90% of their panels are either greater or fewer than the median. This suggests a wide variation in the pretest counseling provided among both breast surgeons and genetic counselors. The differences in ordering panels indicates further research and guidelines may be warranted in this rapidly evolving component of the care of patients with breast cancer.
