Adding Localized Therapy to Ipilimumab Boosts Survival in Melanoma
Patients with metastatic melanoma may benefit from the addition of a local tumor-targeted treatment in addition to ipilimumab.
Patients with metastatic melanoma may benefit from the addition of a local tumor-targeted treatment in addition to ipilimumab (Yervoy), according to the results of a retrospective study
Adding local therapy to ipilimumab increased survival by a median of 51 weeks from 42 weeks to 93 weeks among patients treated with the combination therapy (P = .0028).
Excluding those patients with brain metastases-who were not distributed equally among the two comparator groups-patients treated with the combination therapy had a median survival of 117 weeks compared to 46 weeks among those treated just with ipilimumab.
The survival advantage “seemed to overcome even traditional risk factors of poor outcomes. This suggests that this combination could be an option for all patients with malignant melanoma, and this is being tested in ongoing prospective clinical trials,” said study author Sebastian Theurich, MD, a physician and a scientist in the Center of Integrated Oncology (CIO) at the University Hospital of Cologne, Germany, in an American Association for Cancer Research
Theurich and his colleagues analyzed data from 127 metastatic melanoma patients treated at four different cancer centers in Switzerland and Germany. Eighty-two patients received ipilimumab alone and 45 patients received ipilimumab plus a local therapy for symptom control. The local therapy was used to relieve patients’ symptoms and not as a potential curative treatment. All patients received ipilimumab at the 3 mg/kg dose every 3 weeks. Forty-nine (38.6%) of the patients had brain metastases at the time of ipilimumab therapy initiation.
The number of immune-related adverse events (irAEs) was not significantly increased in patients who received the localized treatment. Eight patients (17.8%) and 15 patients (18.3%) in the combination therapy group and in the ipilimumab alone group, respectively, experienced grade 3 or greater irAEs.
The results are in concordance with a prior study of 29 patients in the United States also treated with ipilimumab and local radiotherapy. “Having data from different parts of the world improves the validity of the results, especially if you deal with retrospective analyses,” added Theurich.
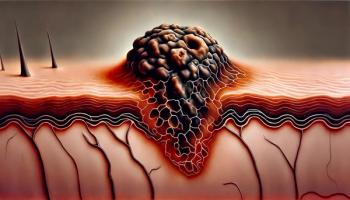
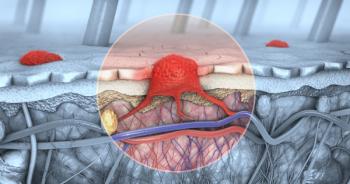
According to the study authors, one potential mechanism of how local therapy facilities a more robust antitumor immune response is that the local peripheral treatments are able to activate immune cells that can then attack tumors.
The limitations of the study are that the study is retrospective and did not compare randomized treatment groups. These results are now being tested in prospective clinical trials.
The study was partly funded by the University of Cologne and the Freie Akademische Gesellschaft Basel, Switzerland.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.