Adverse Effects
Latest News
Latest Videos

Shorts



Podcasts
CME Content
More News
The Chemo Mouthpiece had favorable outcomes when used during and after treatment with chemotherapy among a range of patients with various types of cancer.

A survey found that patients believed dermatologic AEs were more prevalent with anti-cancer therapies than what has been reported.

The intravenous formulation of tocilizumab-anoh for CRS is expected to launch in the US on August 31, 2025.

ATR04-484 showed inhibition of both methicillin-sensitive and methicillin-resistant Staphylococcus aureus bacteria strains, which are associated with rash.
Diverse dermatologic AEs, such as hair and nail toxicities, can be associated with various cancer treatments.

BMI, serum albumin, and G8 screening tool scores were all factors correlated with the likelihood of experiencing a grade 3 or higher AE.
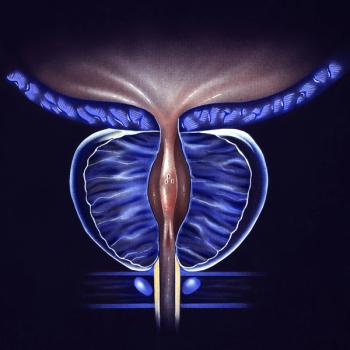
Toxicity complications were assessed between single- and multiple-treatment modalities for patients with localized prostate cancer.

Quality of life improvements can be made if clinicians better understand auditory attention decay after cancer treatment in pediatric patients with cerebellar tumors.

One of the most predictable toxicities of autologous stem cell transplantation for multiple myeloma — even more so than mucositis — is hair loss.
When pembrolizumab is combined with immunotherapies, the incidence of grade 3 to 5 toxicities increases, especially with anti–CTLA-4 combinations.
“We’ve seen with the initial anti-CTLA-4 ipilimumab experience that, as time went by, we were better at identifying and managing toxicities,” stated Omid Hamad, MD.
A pooled analysis found pembrolizumab has a discontinuation rate of 12.7%, and a major key to handling it is maintaining good communication between the doctor and the patient.

All patients who received HT-001 in the phase 2a CLEER-001 trial showed significant skin toxicity improvements by 6 weeks.
Results from the phase 3 AVA-PED-301 trial support the FDA decision for avatrombopag in pediatric thrombocytopenia.

The novel drug showed promise in helping to decrease chemotherapy-induced peripheral neuropathy for those who had received prior chemotherapy.

Study results suggest follow-up with hypercholesterolemia control and audiological assessments for cisplatin-treated patients with cancer.
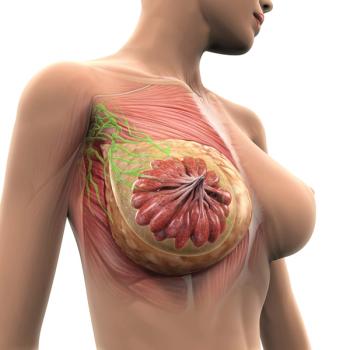
Safety data further support datopotamab deruxtecan as a new treatment option in metastatic hormone receptor–positive, HER2-negative breast cancer.
Additional research may be necessary to validate the efficacy of telehealth interventions in clinical activities for patients with cancer.

Lack of energy, difficulty with sleeping, and pain were some of the most common symptoms reported in older patients with cancer.

Emphasizing precise terminology in clinical studies may improve the transparency and accuracy of information presented at oncology conferences.
Findings from a study raise concerns for the outcomes of individuals who experience an adverse financial event prior to a cancer diagnosis.
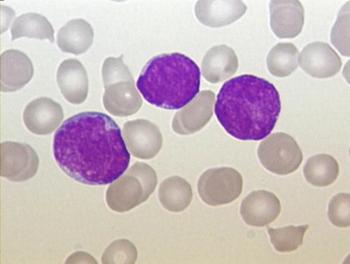
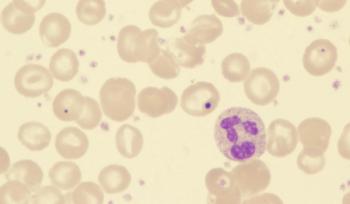
Administering pegylated asparaginase continuously to pediatric patients with acute lymphoblastic leukemia appears to be safe without compromising the efficacy of treatment.

Data from a meta-analysis may provide safety insights for future randomized clinical trials evaluating immune checkpoint blockade in the definitive setting for patients with cancer.

Investigators assess edoxaban as part of a multicenter, open-label superiority trial in patients with active cancer and newly diagnosed isolate distal deep vein thrombosis.

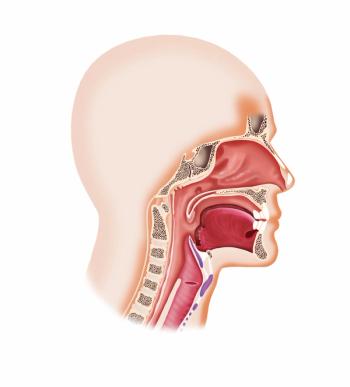
The FDA requires data from an additional clinical trial to support the potential approval of avasopasem for managing radiation-induced severe oral mucositis in patients with head and neck cancer.