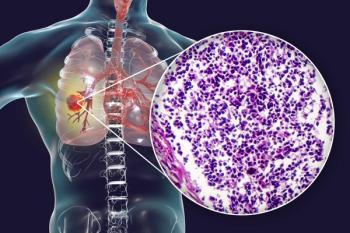
Small Cell Lung Cancer (SCLC)
Latest News
Video Series
Latest Videos
Shorts
Podcasts
CME Content
More News

In a spotlight session at the Chemotherapy Foundation Symposium, Anne Chiang, MD, PhD, covered developments in the field of LS-SCLC.

Data from the DeLLphi-304 trial support the full approval of tarlatamab in this extensive-stage small cell lung cancer population.

Patients with ES-SCLC who had an ECOG performance status of 2 or 3 achieved ORRs of 52.4% and 45.5%, respectively, with the study treatment.

Data show that XCR1-positive conventional type 1 dendritic cells may play a role as mediators of response to atezolizumab in extensive-stage SCLC.

Combinations of antiangiogenic therapy with chemoimmunotherapy may feasibly be shifted forward in real-world extensive-stage small cell lung cancer care.
Findings from the RATIONALE-312 trial support tislelizumab plus chemotherapy as a frontline treatment option in extensive-stage small cell lung cancer.

Data from IDeate-Lung01 reveal a disease control rate exceeding 90% with infinatamab deruxtecan.

Data from DeLLphi-304 support the use of tarlatamab as a standard of care for all patients with second-line small cell lung cancer.

Tarlatamab plus chemo/IO showed a 71% objective response rate and promising safety for patients with ES-SCLC in the DeLLphi-303 study.

Those with limited-stage small cell lung cancer who had elevated ProGRP levels at baseline had worse OS and PFS outcomes vs those with normalized levels.

Twice-daily radiotherapy prolongs survival vs once-daily radiation among those with LS-SCLC, even with the incorporation of immunotherapy.

Data from the phase 3 IMforte trial support the FDA approval of maintenance lurbinectedin plus atezolizumab in extensive-stage small cell lung cancer.
A real-world, retrospective analysis showed that CRS and ICANS occurred in 48% and 16% of patients with ES-SCLC who were treated with tarlatamab.
Biomarker research may better elucidate clinical benefit and identify mechanisms of resistance with tarlatamab in extensive-stage small cell lung cancer.

Clinical trials in small cell lung cancer appear to be more “pragmatic” with their inclusion criteria than before, according to Anne Chiang, MD, PhD.

The frontline treatment algorithm in SCLC is poised to look “radically different” in the upcoming years, according to Anne Chiang, MD, PhD.

In patients with ES-ECLC treated with chemotherapy and immunotherapy, stereotactic body radiation therapy did not significantly improve overall survival.

CAR T-cell therapies or other agents that affect the immune system in the long term may be important to keep in mind for the management of SCLC.

Employing patient-reported outcomes may help include those with small cell lung cancer in the shared decision-making process.

In the SWOG S2409 PRISM trial, over 800 patients with small cell lung cancer will receive different treatment regimens based on their disease subtype.

In patients with LS-SCLC who were ineligible for a prophylactic cranial irradiation, toripalimab appeared to decrease the progression of brain metastases.

Future biomarker analysis will include correlation of efficacy with SLFN11 expression and with markers of DNA damage repair.
Cisplatin/etoposide and carboplatin/etoposide achieved median OS of 8.8 months and 7.8 months, respectively, in those with extensive-stage small cell lung cancer.

Data from the IDeate-Lung01 trial support the potential role that ifinatamab deruxtecan may play in the management of extensive-stage small cell lung cancer.

Lurbinectedin achieved an ORR of 27% in all patients with extensive-stage small cell lung cancer in the phase 4 Jazz Emerge 402 study.