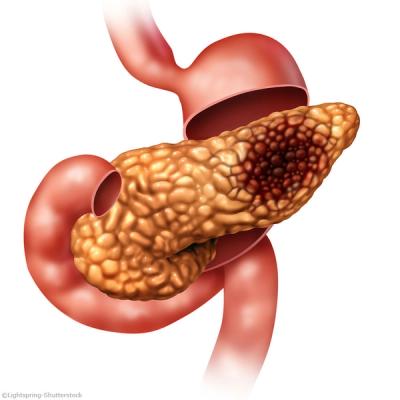
Pancreatic Cancer
Latest News
Video Series

Latest Videos
Shorts

Podcasts
CME Content
More News

Results from the phase 3 COMPETE trial demonstrated that 177Lu-edotreotide improved PFS and ORR compared with everolimus in patients with GEP-NETs.

Phase 2 data show consistent overall immunotherapy immunogenicity with ELI-002 7P in those with KRAS-mutated pancreatic ductal adenocarcinoma.

Considering historical trends of underpowered data in NET surgical studies, CUTNETs established a collaboration of surgical teams to better power research.
Kenneth H. Yu, MD, discusses the results from the SHARON trial in pancreatic cancer that were presented at ESMO 2025.

Results from the SHARON trial presented at ESMO 2025 showed a potential treatment option for patients with PDAC who have BRCA1/2 or PALB2 mutations.

The safety profile of telisotuzumab adizutecan was manageable in pancreatic ductal adenocarcinoma, consistent with its profile in other tumor types.

Serious AEs occurred in 49% of patients treated with FOLFIRNOX vs 43% of patients treated with chemoradiation for pancreatic ductal adenocarcinoma.

Atebimetinib with gemcitabine and nab-paclitaxel achieved 9-month OS and PFS of 86% and 53%, respectively, in patients with pancreatic cancer in frontline settings.
At 30 months, mitazalimab plus mFOLFIRINOX achieved an OS rate of 21% in patients with previously untreated metastatic PDAC.

Patients with PDAC and non-GOF mutations had less favorable OS and DFS outcomes in various instances compared with those who had wild-type genes or GOF mutations.

An independent data monitoring committee recommended the continuation of the phase 2 AMPLIFY-7P trial evaluating ELI-002 7P in PDAC in August 2025.
After the predictive probability of achieving superiority with mFOLFIRINOX or S-IROX was less than 1%, the trial was terminated due to futility.

TTFields plus chemotherapy significantly prolonged overall survival compared with chemotherapy alone in patients with pancreatic cancer.

Induction chemotherapy may allow investigators to biologically select patients with a favorable prognosis who benefit most from chemoradiotherapy.

The retrospective study is the largest to evaluate the relationship between dose-averaged LET profiles and local control after CIRT for pancreatic cancer.
Data from the PANOVA-3 trial may support the concomitant use of TTFields plus standard of care in solid tumors across different therapeutic settings.

The independent data monitoring committee confirmed the favorable safety profile of ELI-002 7P for the treatment of PDAC in the phase 1/2 AMPLIFY-7P trial.

Results from a phase 1/2a trial supported the designation for VS-7375 in those with PDAC harboring a KRAS G12D mutation.

Results from the phase 3 CABINET trial demonstrated a clear progression-free survival benefit with cabozantinib vs placebo in patients with well-differentiated pNET/epNET.

Quemliclustat plus gemcitabine and nab-paclitaxel chemotherapy outperformed median OS benchmarks in patients with metastatic PDAC.
Explore the latest advancements in pancreatic cancer treatment, focusing on genetic mutations, targeted therapies, and emerging clinical strategies.

Findings from the phase 2b ASCEND trial will be presented at the European Society for Medical Oncology Gastrointestinal Cancers Congress on July 2, 2025.

Elraglusib plus gemcitabine and nab-paclitaxel demonstrated a median OS of 12.5 months vs 8.5 months with chemotherapy alone in patients with PDAC.

Stereotactic online adaptive magnetic resonance–guided radiation therapy was well tolerated and maintained stable QOL in patients with PDAC for up to 1 year.

Results from a phase 2a trial showed a 6-month OS and PFS rate of 94% and 72% compared with 67% and 44% from the phase 3 MPACT trial in the first-line treatment of PDAC.