Afami-cel Demonstrates Enduring Responses in Pretreated Synovial Sarcoma
Findings from the phase 2 SPEARHEAD-1 trial demonstrate how T-cell receptor therapy may effectively target solid tumors.
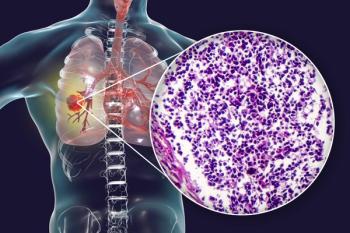
Combining afamitresgene autoleucel (afami-cel) with lymphodepletion chemotherapy produced sustained responses in patients with previously treated, HLA-A*02–positive, MAGE-A4–positive synovial sarcoma and myxoid round cell liposarcoma, according to findings from the phase 2 SPEARHEAD-1 trial (NCT04044768) published in The Lancet.1
The overall response rate (ORR) across the modified intent-to-treat (ITT) population was 37% (n = 19/52; 95% CI, 24%-51%), with all responses consisting of partial responses (PRs). Specifically, the ORR was 39% (n = 17/44) for patients with synovial sarcoma and 25% (n = 2/8) for those with myxoid round cell liposarcoma. Data highlighted a concordance rate of 79% between independent and investigator-based assessments of ORR.
Among responders, the median time to initial confirmed response was 4.9 weeks (95% CI, 4.3-8.1), and the median duration of response (DOR) was 11.6 months (95% CI, 4.4-18.0) in patients with synovial sarcoma and 4.2 months (95% CI, 2.9-5.5) among those with myxoid round cell liposarcoma. Investigators reported responses across key subgroups, with more frequent responses occurring among female patients with synovial sarcoma, those with higher MAGE-A4 expression, lower disease burden prior to lymphodepletion, and those who did not receive bridging therapy.
The median overall survival (OS) was 15.4 months (95% CI, 10.9-28.7) among patients in the overall population, and the estimated 12-month OS probability was 60% (95% CI, 46%-73%). Among patients with a response in the synovial sarcoma group, the median OS was not reached (NR; 95% CI, 15.4-not estimable [NE]), the estimated 12-month OS rate was 90% (95% CI, 65%-99%), and the estimated 24-month OS rate was 70% (95% CI, 43%-87%).
“The use of CAR T-cell therapies targeting cell surface cancer antigens in hematological malignancies is well established, but their activity in solid tumors has been disappointing. Solid tumors can have an immunosuppressive microenvironment that makes effective treatment with cell therapy more challenging than for hematological malignancies,” Sandra P. D’Angelo, MD, a sarcoma oncologist and cellular therapist at Memorial Sloan Kettering Cancer Center, and coauthors wrote.
“This study shows the ability to effectively target solid tumor cancer antigens with T-cell receptor therapy and highlights MAGE-A4 as a new immunotherapy target for the treatment of synovial sarcoma. Our findings support the use of afami-cel as a potentially effective treatment option for patients with HLA-A*02–positive and MAGE-A4–positive synovial sarcoma following progression despite previous anthracycline-based or ifosfamide-based therapy.”
The open-label SPEARHEAD-1 trial included 3 patient cohorts; the findings of this report pertained to cohort 1. In this cohort, 52 patients who were 16 to 75 years old with HLA-A*02–positive, metastatic, unresectable synovial sarcoma (n = 44), or myxoid round cell liposarcoma (n = 8) expressing MAGE-A4 and previously received treatment with anthracycline-containing or ifosfamide-based chemotherapy were evaluated. Following lymphodepletion, patients received afami-cel as a single intravenous infusion at 1.0 x 109 to 10.0 x 109 T cells.
The trial’s primary end point was ORR in the cohort based on independent review committee assessment per RECIST v1.1 criteria. Secondary end points included treatment-emergent adverse effects (TEAEs), DOR, time to initial confirmed response, progression-free survival, and OS.
Across the overall population, most patients were male (54%), White (87%), not Hispanic (83%), and from Canada or the United States (71%). Additionally, most patients had poorly differentiated histology (50%), stage IV disease (79%), 4 or more prior lines of treatment (35%), no bridging therapy (62%), and an ECOG performance status of 0 (52%).
TEAEs affected all patients who were treated with afami-cel. The most common any-grade TEAEs included cytokine release syndrome (CRS; 71%), decreased white blood cell counts or leukopenia (27%), pyrexia (23%), decreased neutrophil counts or neutropenia (23%), and decreased lymphocyte counts or lymphopenia (17%). There were no treatment-related deaths.
In February 2024,
Reference
- D’Angelo SP, Araujo DM, Abdul Razak AR, et al. Afamitresgene autoleucel for advanced synovial sarcoma and myxoid round cell liposarcoma (SPEARHEAD-1): an international, open-label, phase 2 trial. The Lancet. Published online March 27, 2024. doi:10.1016/S0140-6736(24)00319-2
- Adaptimmune announces U.S. FDA acceptance of biologics license application for afami-cel for the treatment of advanced synovial sarcoma with priority review. News release. Adaptimmune Therapeutics. January 31, 2024. Accessed April 1, 2024. http://tinyurl.com/3xr923n4
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.