Oncology NEWS International
- Oncology NEWS International Vol 14 No 3
- Volume 14
- Issue 3
After 2 Years of Tam, Switching to Anastrozole Is More Effective
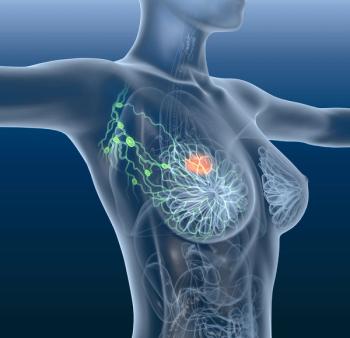
SAN ANTONIO-For postmenopausal women with hormone-receptor-positive early-stage breast cancer, switching to anastrozole (Arimidex) after 2 years of tamoxifen is more effective than continuing on tamoxifen, according to Raimund Jakesz, MD, Vienna Medical School, Vienna, Austria. The conclusion arose out of analysis of combined results of two trials enrolling a total of 3,224 women: the Viennese ABCSG (Austrian Breast and Colorectal Cancer Study Group) Trial 8, and the German ARNO 95 Trial (by the German Adjuvant Breast Cancer Group).
SAN ANTONIOFor postmenopausal women with hormone-receptor-positive early-stage breast cancer, switching to anastrozole (Arimidex) after 2 years of tamoxifen is more effective than continuing on tamoxifen, according to Raimund Jakesz, MD, Vienna Medical School, Vienna, Austria. The conclusion arose out of analysis of combined results of two trials enrolling a total of 3,224 women: the Viennese ABCSG (Austrian Breast and Colorectal Cancer Study Group) Trial 8, and the German ARNO 95 Trial (by the German Adjuvant Breast Cancer Group).
The ABCSG and ARNO trials were nearly identical, Dr. Jakesz said at the 27th Annual San Antonio Breast Cancer Symposium (abstract 2). They included primarily favorable prognostic groups (T1 70%, node negative 74%, grade 1-2 95%). The main difference was that the ABCSG trial allowed grade 1-2 tumors, while ARNO also included grade 3 tumors. Nearly 40% were less than 60 years old. About 81% were both estrogen-receptor and progesterone-receptor positive. Breast conservation was possible in approximately 77%. No patients received chemotherapy.
In both trials, patients were randomized to 3 years of tamoxifen (n = 1,606) or anastrozole (n = 1,618) after 2 years of tamoxifen. The primary endpoint was event-free survival, with events defined as locoregional recurrences, distant metastases, or contralateral breast cancer.
In this interim analysis, event-free survival significantly favored anastrozole (see Table), with a 40% risk reduction. The finding met the stopping boundary for event-free survival, and no further patients are being recruited into the two studies. An analysis of variables affecting event-free survival showed anastrozole to be an independent prognostic factor, along with negative nodal status and non-grade 3 tumor grade.
Dr. Jakesz noted that unlike other trials, the major difference in events between tamoxifen and anastrozole was in distant recurrences, with 75 such events in the tamoxifen group and 46 in the anastrozole group, resulting in a significant difference in distant-recurrence-free survival favoring anastrozole (HR = 0.61, P = .0067). There was no overall survival benefit for anastrozole, which Dr. Jakesz attributed to the low number of deaths and the short follow-up period.
Overall, both treatments were well tolerated. As expected, there were significantly more fractures in patients switching to anastrozole27 (2.4%) vs 14 (1.2%) for tamoxifen. Dr. Jakesz pointed out that because gynecological side effects generally occur soon after initiating tamoxifen therapy, there were no differences between groups in this respect.
Based on both event-free and distant-recurrence-free survival, the superior strategy, Dr. Jakesz concluded, is to switch women from tamoxifen to anastrozole at 2 years. Studies are needed to determine whether initial adjuvant anastrozole given for 5 years is superior to switching from tamoxifen to anastrozole after 2 years. He noted that ABCSG-16 (SALSA) is evaluating 2 vs 5 years of anastrozole following 3 years of tamoxifen therapy.
Articles in this issue
about 21 years ago
Smoking Speeds Progression of Pancreas Caabout 21 years ago
Alcohol, Obesity, and Smoking Risk Factors for HCCabout 21 years ago
Adding Bevacizumab Improves Response to Oxaliplatin Regimensabout 21 years ago
Capecitabine Promises Convenience, Efficacy in LARC, Five Studies Showabout 21 years ago
Avastin Enhances FOLFOX Efficacyabout 21 years ago
Panitumumab, Anti-EGFR MoAb,Promising in Colon Cancerabout 21 years ago
Oxaliplatin/Gemcitabine Effective in Advanced Pancreatic Cancerabout 21 years ago
Study Strengthens Evidence of Link Between Liver Cancer and Diabetesabout 21 years ago
Capecitabine Promises Convenience, Efficacy in LARC, Five Studies ShowNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.