
Approval of Adagrasib for KRAS G12C–Mutated NSCLC Will ‘Open Up Another Therapeutic Option’, Says Expert
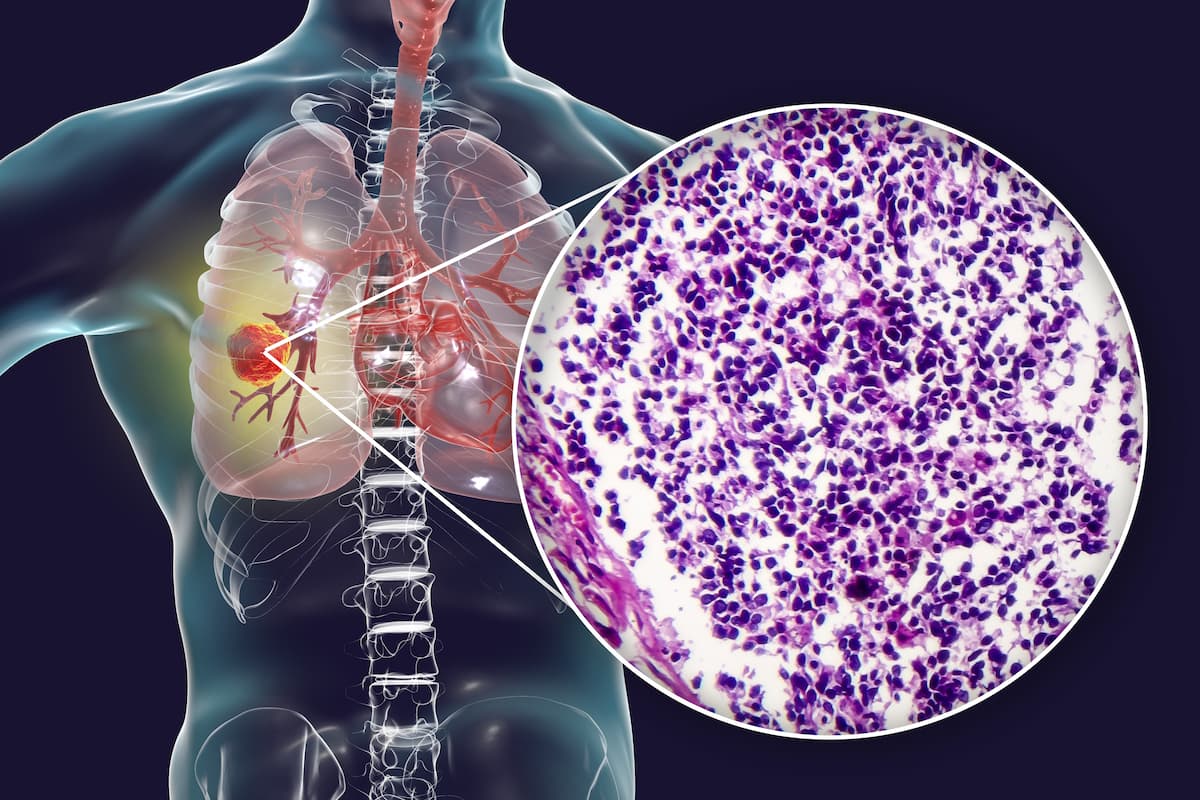
Alexander Spira, MD, PhD, FACP, of the Virginia Cancer Specialists, discusses how the FDA approval of adagrasib for KRAS G12C–mutated non–small cell lung cancer can provide benefit for this patient population.
In an interview with CancerNetwork®, Alexander Spira, MD, PhD, FACP, a medical oncologist and co-director of the Virginia Cancer Specialists Research Institution, as well as the director of the Thoracic and Phase I Program and clinical assistant professor at Johns Hopkins University, spoke about the
According to Spira, the approval of adagrasib allows for another treatment option for patients with KRAS G12C–mutated NSCLC who may tolerate the agent more than other approved therapies such as sotorasib (Lumakras). He also described other benefits of the agent in terms of managing central nervous system (CNS) metastases.
Transcript:
The approval of adagrasib for KRAS G12C–mutated non–small cell lung cancer will open up another therapeutic option. As you know, we have sotorasib already approved, but [these agents] do have slightly different toxicity profiles. It's always good to have more than one class because some people do tolerate one better than the other one. It also verifies the fact that this is now an actual genetic mutation for which we've been trying to find drugs for the better part of a quarter century. The other thing that is that adagrasib does have some [central nervous system] CNS activity, and these patients do have a predilection to CNS metastases. Hopefully, it could be used in that situation for the right patients, although this would likely not be on the label.
Reference
FDA grants accelerated approval to adagrasib for KRAS G12C-mutated NSCLC. News release. FDA. December 12, 2022. Accessed December 13, 2022. https://bit.ly/3UUVphS
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.



































