
Approval of Mosunetuzumab Becomes ‘Critically Important’ First-Line Treatment Option in R/R Follicular Lymphoma, Expert Says
An expert from Rutgers Cancer Institute reviews data that lead to the approval of mosunetuzumab for patients with relapsed/refractory follicular lymphoma.
Results from the
Matasar, an investigator of the study, chief of the Division of Blood Disorders at Rutgers Cancer Institute, and professor at Rutgers Robert Wood Johnson Medical School spoke with CancerNetwork® regarding the trial’s updated results that were presented at the
Of note, the agent yielded an objective response rate of 78% and a complete response of 60%. Moreover the 24-month DOR rate was 53% (95% CI, 38%-68%), and the 24-month duration of CR rate was 63% (95% CI, 38%-88%).
Transcript:
The approval of mosunetuzumab for patients with relapsed/refractory follicular lymphoma after 2 or more prior lines of therapy is an important event. This is a critically important approval for this patient population. Patients with follicular lymphoma have relatively few options prior to the approval of mosunetuzumab. In terms of FDA-approved therapy, we have CAR T-cell therapy, and we have some PI3K inhibitors available.
For patients who have already [been exposed to] cytotoxic chemotherapy and immunomodulatory therapy such as [lenalidomide] Revlimid options were relatively few and outcomes with subsequent lines of therapy tend to be suboptimal.
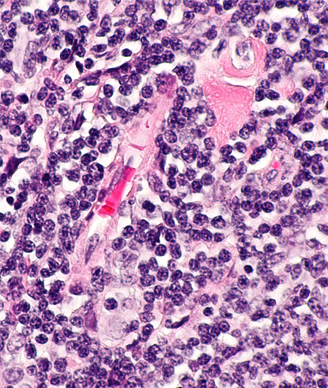
Mosunetuzumab is a first in-class approval of bispecific antibodies targeting CD20 and CD3. The activity in [patients with] follicular lymphoma is excellent with an overall response rate of approximately 80% and a complete response rate of approximately 60%.
It is increasingly clear that these responses can indeed be durable with median follow-up reported of over 2 years without having achieved median progression-free survival, duration of response, duration of complete response, and we’re seeing both good tolerability as well as excellent durability of these responses in an otherwise hard to treat patient population.
References
- FDA approves Genentech’s Lunsumio, a first-in-class bispecific antibody, to treat people with relapsed/refractory follicular lymphoma. News release. Genentech. December 22, 2022. Accessed January 6, 2023. https://bit.ly/3FPCn7h
- Bartlett NL, Sehn LH, Matasar MJ, et al. Mosunetuzumab monotherapy demonstrates durable efficacy with a manageable safety profile in patients with relapsed/refractory follicular lymphoma who received ≥2 prior therapies: updated results from a pivotal phase II study. Blood. 2022;140(suppl 1):1467-1470.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.



































