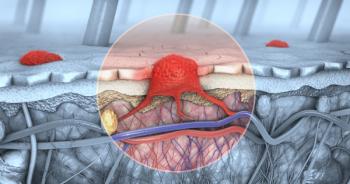
Efficacy of One-Day Fractionated Photodynamic Therapy for Basal Cell Carcinoma
Researchers evaluated the response of patients with BCC to fractionated photodynamic therapy at 30 days after treatment.
Fractionated photodynamic therapy offers good aesthetic results and complete response in patients with basal cell carcinoma when assessed at 30 days after treatment, according to the results of a study
The total dose of light is delivered in steps with fractionated photodynamic therapy, and the intervention lasts 1 day (administered over two 3-hour sessions). In Europe, photodynamic therapy is typically given in two doses, a week apart, which exposes the patient to added pain and discomfort compared with a one-time intervention.
In an interview with Cancer Network, Meenal Kheterpal, MD, a dermatologist at Duke Health, likened the additional day of treatment to experiencing a painful injury twice in a week.
“If you tore your ACL, would you go in and have it torn again the next week?” asked Kheterpal.“Probably not. Pain and discomfort are big issues. The fact that they can do it all in one day…might be a viable treatment.”
Kheterpal also pointed out that few Americans can tolerate two photodynamic therapy treatments a week apart. “Practically, that doesn’t often work,” she said. “Most people will do it and repeat it in 6 months.”
Kheterpal was also intrigued that the researchers applied the active ingredient, methyl aminolevulinate (MAL), before each session, when treating patients with fractionated photodynamic therapy.
“Re-applying MAL may allow it penetrate deeper and improve efficacy,” she said. She noted, however, that the price of an additional applicator, which can be high, may be tricky to get covered by insurers.
Kheterpal suggested an alternative to fractionated photodynamic therapy: a topical immunotherapy cream called imiquimod.
“Would you choose PDT where you have to come in and have this painful experience?” said Kheterpal. “Or, would you rather use a cream at home once daily for 6 weeks and theoretically get a more effective response? Aldara [imiquimod] is more effective and cheaper, based on 5-year, longitudinal, prospective data when compared to photodynamic therapy and may be more convenient for many.”
Kheterpal recognized that fractionated photodynamic therapy may still be the best option in patients who would not adhere to daily doses of imiquimod. Notably, although not as painful as fractionated photodynamic therapy, which she compared to the pain of a “severe” sunburn, imiquimod still hurts and causes symptoms akin to poison ivy rash, she said.
“PDT is a very nice treatment,” concluded Kheterpal. “There is data to support that PDT also has some cosmetic benefit to it, and patients should know that. Our job as physicians is to help our patients understand the risks and benefits of treatment, such that they can choose the right option for their condition.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.