HER2-Positive Breast Cancer Patients Prefer Subcutaneous Trastuzumab
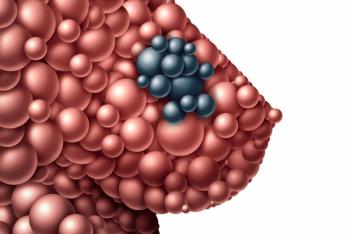
Results of the PrefHer study indicated that when given the option between subcutaneous trastuzumab and intravenous trastuzumab, significantly more patients with HER2-positive breast cancer preferred the subcutaneous administration.
Results of the PrefHer study indicated that when given the option between subcutaneous trastuzumab and intravenous trastuzumab, significantly more patients with HER2-positive breast cancer preferred the subcutaneous administration.
This preference combined with previously published noninferiority results indicates that a fixed dose of 600 mg subcutaneous trastuzumab every 3 weeks is a “validated, well tolerated and preferred option of patients for the treatment of HER2-positive breast cancer.”
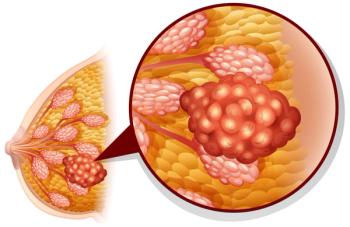
Intravenous trastuzumab is currently the standard of care for patients with HER2 disease. However, a subcutaneous version of the drug has been developed that would allow patients to self-administer with a single-use injection device. Prior research showed that the subcutaneous formulation of the drug was noninferior to the intravenous formulation.
In this study, researchers led by Xavier Pivot, MD, of CHU Jean Minjoz in Besancon, France, randomly assigned 124 patients to receive subcutaneous trastuzumab followed by intravenous trastuzumab, and 124 patients to receive the opposite sequence. All patients were aged 18 years or older and had HER2-positive primary breast adenocarcinoma with no residual, recurrent or metastatic disease. The
Of the 124 patients in each arm, 117 from the subcutaneous first group and 119 in the intravenous first group were included in the intent-to-treat population. In order to determine patient preference for subcutaneous vs intravenous administration, the researchers interviewed patients at baseline and after both treatments.
At study end, 91.5% of patients interviewed stated that they preferred the subcutaneous administration of trastuzumab compared with intravenous (95% CI, 87.2–94.7; P < .0001). In contrast, 6.8% of patients preferred intravenous administration (95% CI, 3.9–10.8). Four patients reported no preference.
The increased preference for subcutaneous administration occurred despite an increased occurrence of adverse events. Fifty-eight percent of patients reported adverse events during subcutaneous treatment compared with 44% during intravenous administration.
In an
Melichar congratulated the researchers on conducting this study for providing evidence in support of the use of subcutaneous trastuzumab, which could be self-administered in situations where patients live far from cancer centers, and for examining the question of patient preference at all.
“Only recently, prospective randomized trials examining aspects of cancer therapy associated with patient preference have been reported (eg, the PISCES trial, which compared pazopanib and sunitinib in metastatic renal-cell carcinoma),” Melichar wrote. “Doctors will still have to learn how to interpret this type of data. However, trials such as PISCES or PrefHer will remain, despite inherent limitations of pivotal studies that established the field, the foundations on which future investigations might be built.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.