Intermittent IFN Alfa-2b Not Recommended for High-Risk Melanoma
Researchers testing the use of intermittent high-dose interferon alfa-2b cannot currently recommend the regimen as an adjuvant treatment for high-risk melanoma.
Although the regimen provided some benefits, researchers testing the use of intermittent high-dose interferon (IFN) alfa-2b (iHDI) cannot currently recommend the regimen as an adjuvant treatment for high-risk melanoma, according to the results of a phase III study
“The present DeCOG [Dermatologic Cooperative Oncology Group] trial demonstrated that intermittent high-dose IFN alfa-2b administered intravenously is not superior to standard 1-year HDI therapy in patients with resected stage III melanoma, despite the promising safety and toxicity profile for intermittent HDI,” wrote Peter Mohr, MD, of Elbe-Klinikum Buxtehude Am Krankenhaus in Buxtehude, Germany, and colleagues.
According to the study, standard regimens of high-dose IFN and its maintenance therapy result in debilitating adverse effects that often lead to dose reductions and treatment withdrawal. Therefore, treatment regimens that include intermittent treatment have been studied to see if they are associated with less toxicity and greater convenience to patients.
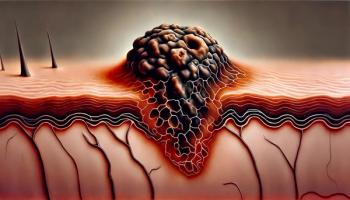
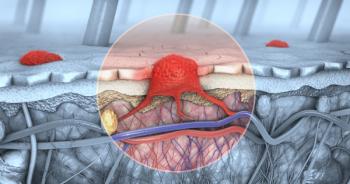
In this analysis by the DeCOG, the researchers enrolled 649 patients with stage III resected lymph node or in-transit metastasis from cutaneous malignant melanoma. Patients were randomly assigned to treatment with either high-dose IFN alfa-2b given at 20 MIU/m2 per day, 5 days a week for 4 weeks, followed by maintenance with 10 MIU/m2 per day, 3 days a week for 48 weeks (standard); or 3 courses of IFN alfa-2b at 20 MIU/m2 given 5 days a week for 4 weeks then repeated every 4 months. The intent-to-treat analysis included 627 patients.
With a median follow-up of more than 4 years, no significant difference was found between the two treatment regimens for distant metastasis–free survival (P = .12) or overall survival (P = .85). However, patients treated with the standard high-dose regimen had significantly better relapse-free survival (hazard ratio, 1.27; P = .03) compared with those assigned to the intermittent regimen.
According to the researchers, “Although distant metastasis–free survival did not significantly differ between the arms, recurrence-free survival is regarded as an important end point for adjuvant treatments. Therefore, the difference in recurrence-free survival favoring standard HDI is a crucial finding.”
Patients assigned to the standard regimen had a lower rate of treatment discontinuation due to recurrence of their disease (25% vs 29.6%). However, discontinuation of treatment due to adverse events was about half as much in patients assigned to the intermittent regimen compared with standard of care (6.8% vs 14.6%), and fewer patients on intermittent therapy reported impairment to quality of life (8.0% vs 11.4%).
“Of interest, no cumulative toxicity was observed after three cycles of iHDI. Therefore, the overall effect on quality of life was substantially less with three courses of iHDI than with conventional HDI,” wrote the researchers. “However, any improvement in tolerability and quality of life must be contrasted with a potential loss of efficacy because at least 50% of patients would tolerate moderate or severe IFN alfa-2b toxicity for 4% or 10% improvement in 5-year disease-free survival, respectively.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.