- ONCOLOGY Vol 17 No 9
- Volume 17
- Issue 9
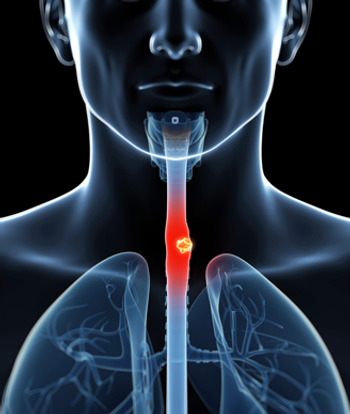
Irinotecan/Cisplatin Followed by 5-FU/ Paclitaxel/Radiotherapy and Surgery in Esophageal Cancer
Local-regional carcinoma of the esophagus is often diagnosed inadvanced stages because the diagnosis is established when symptomsare severe. The prognosis of patients with local-regional carcinoma ofthe esophagus continues to be grim. While preoperative chemoradiotherapyincreases the fraction of patients who achieve pathologiccomplete response, that percentage is approximately 25%. In an attemptto increase the number of patients with either no cancer in the surgicalspecimen or only microscopic cancer, we adopted a three-step strategy.The current study utilized up to two 6-week cycles of induction chemotherapywith irinotecan (CPT-11, Camptosar) and cisplatin as step 1.This was followed by concurrent radiotherapy and chemotherapy withcontinuous infusion fluorouracil (5-FU) and paclitaxel as step 2. Oncethe patients recovered from chemoradiotherapy, a preoperative evaluationwas performed and surgery was attempted. All patients signed aninformed consent prior to their participation on the study. A total of 43patients were enrolled. The baseline endoscopic ultrasonography revealedthat 36 patients had a T3 tumor, five patients had a T2 tumor, andtwo had a T1 tumor. Twenty-seven patients had node-positive cancer(N1). Thirty-nine (91%) of the 43 patients underwent surgery; all hadan R0 (curative) resection. A pathologic complete response was noted in12 of the 39 patients. In addition, 17 patients had only microscopic(< 10%) viable cancer in the specimen. Therefore, a significant pathologicresponse was seen in 29 (74%) of 39 taken to surgery or 29 (67%)of all 43 patients enrolled on the study. With a median follow up beyond25 months, 20 patients remain alive and 12 patients remain free ofcancer. Our preliminary data suggest that the proportion of patientswith significant pathologic response can be increased by using thethree-step strategy.
ABSTRACT: Local-regional carcinoma of the esophagus is often diagnosed inadvanced stages because the diagnosis is established when symptomsare severe. The prognosis of patients with local-regional carcinoma ofthe esophagus continues to be grim. While preoperative chemoradiotherapyincreases the fraction of patients who achieve pathologiccomplete response, that percentage is approximately 25%. In an attemptto increase the number of patients with either no cancer in the surgicalspecimen or only microscopic cancer, we adopted a three-step strategy.The current study utilized up to two 6-week cycles of induction chemotherapywith irinotecan (CPT-11, Camptosar) and cisplatin as step 1.This was followed by concurrent radiotherapy and chemotherapy withcontinuous infusion fluorouracil (5-FU) and paclitaxel as step 2. Oncethe patients recovered from chemoradiotherapy, a preoperative evaluationwas performed and surgery was attempted. All patients signed aninformed consent prior to their participation on the study. A total of 43patients were enrolled. The baseline endoscopic ultrasonography revealedthat 36 patients had a T3 tumor, five patients had a T2 tumor, andtwo had a T1 tumor. Twenty-seven patients had node-positive cancer(N1). Thirty-nine (91%) of the 43 patients underwent surgery; all hadan R0 (curative) resection. A pathologic complete response was noted in12 of the 39 patients. In addition, 17 patients had only microscopic(Carcinoma of the esophagus is avirulent malignancy that is diagnosedonly when patientsexperience rather severe and advancedsymptoms. As a result, it is not uncommonto find M1 cancer at diagnosisor node-positive cancer on initialstaging. Approximately 13,900 newcases of esophageal cancer (more thanhalf involving the gastroesophagealjunction) are diagnosed each year inthe United States.[1] In the West,esophageal cancer has undergone arapid evolution affecting predominantlyCaucasian men and having an adenocarcinomahistology. Associationwith Barrett's metaplasia, reflux disease,hiatal hernia, and obesity is alsoevident.[2] This is in contrast to endemicareas where squamous cell histologypredominates, and mid- or upper thoracic localization is common.The carcinogenic forces at workare also different.The 5-year survival rate of patientswith local-regional esophageal or gastroesophagealcarcinoma is approximately15% to 20%. This cure ratecan be obtained by surgery, and by some estimates, also by definitivechemoradiotherapy. The data on definitivechemoradiotherapy are predominantlyon squamous cellcarcinoma. For patients taken straightto surgery, an R0 (curative) resectionrate of 60% and 3-year overall survivalrate of approximately 30% isexpected.[3] Surgical mortality hasbeen substantially reduced in recentyears due to improved supportive careand better patient selection. Nonetheless,it is well understood that mortalityand morbidity are directly relatedto number of surgeries performed at agiven institution. For example, the dataof Swisher et al demonstrated thathospitals that perform a large numberof esophagectomies demonstrated improvedoutcomes and decreased hospitaluse.[4]For patients with localized esophagealcarcinoma, the challenges include(1) proper selection of patientswho are most likely to benefit fromthe stipulated approach; (2) achievementof an R0 resection when surgeryis contemplated; (3) achievement ofpathologic complete response or< 10% microscopic cancer in the surgicalspecimen (two groups that havea better survival than those with> 10% residual cancer); (4) reducingthe rate of persistent or locally recurrentcancer when using definitivechemoradiotherapy, (a rate currentlyabove 60%-a desired number wouldbe 30%); (5) reducing morbidity fromchemoradiotherapy, surgery, and chemotherapyby providing adequate nutrition,supportive care, and willingnessto constantly refine approaches; and(6) improving staging procedures againto select the proper patients.The three-step strategy providesmore theoretical advantages than thepreviously used uni- or dual-modalityapproaches.[5] We elected to use acombination of irinotecan (CPT-11,Camptosar) and cisplatin that has demonstratedactivity in patients with carcinomaof the esophagus.[6] We chosecontinuous infusion of fluorouracil (5-FU) and paclitaxel with radiotherapy,as it has previously resulted in loweredmorbidity in patients with carcinomaof the esophagus andgastroesophageal junction in previousstudies by our group.[7]Our objectives in this trial were toincrease the R0 resection rate, increasethe fraction of patients who achievesignificant pathologic response, andevaluate morbidity and mortality. Thedata being discussed are preliminary.MethodsPatients with potentially resectableadenocarcinoma or squamous cell carcinomaof the esophagus or gastroesophagealjunction with histologicproof of adenocarcinoma underwentfull staging including endoscopic ultrasonography.The patients had acceptablehepatic, renal, and marrowfunction. They were male or female,18 years or older, with a performancestatus (PS) ≤ 2. Patients with celiacadenopathy (≥ 1 cm) visualized byCT scan (except when the gastroesophagealjunction was involved)were not registered in the study. Allpatients gave written informed consent.Patients had to be medically fitto withstand surgery. At the time whenthis protocol was initiated, neither ourinstitution nor others routinely usedpositron emission tomographyscanning.Irinotecan was given at 70 mg/m2,and cisplatin given at 20 mg/m2 IVonce a week on days 1, 7, 21, and 28,but not on days 14 and 35 (one cycle).If a patient achieved a clinical response,a second cycle of irinotecan/cisplatin was given that began on day42 (day 1 of the second cycle).The patients received radiotherapyat 45 Gy (1.8-Gy fractions) and continuousinfusion low-dose 5-FU at 300mg/m
Articles in this issue
over 22 years ago
Cancer Websites You Can Use:People Living With Cancerover 22 years ago
Toward a Breast Cancer Vaccine:Work in Progressover 22 years ago
Cervical Cancer: Issues of Sexuality and FertilityNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.