Malignant Melanoma: Biology, Diagnosis, and Management
Cutaneous malignant melanoma is a relatively common neoplasm. In the United States in 1995, an estimated 34,000 cases of melanoma will be diagnosed, and 7,200 persons will die of melanoma [1]. Early primary melanoma is highly curable, but once the disease becomes disseminated, it is nearly always fatal. The overall survival rate has more than doubled from 40% in the 1960s to more than 80% today, but this increase is attributable to earlier diagnosis rather than to treatment advances [2].
Cutaneous malignant melanoma is a relatively common neoplasm. In the United States in 1995, an estimated 34,000 cases of melanoma will be diagnosed, and 7,200 persons will die of melanoma [1]. Early primary melanoma is highly curable, but once the disease becomes disseminated, it is nearly always fatal. The overall survival rate has more than doubled from 40% in the 1960s to more than 80% today, but this increase is attributable to earlier diagnosis rather than to treatment advances [2]. Treatment for locally advanced or metastatic melanoma has been largely unsatisfactory despite ongoing basic science research and innovative clinical approaches such as biotherapy, vaccines, and regional perfusion therapy. However, several new treatment strategies do show promise. This chapter reviews current epidemiologic and biologic aspects of melanoma, briefly describes the commonly used staging systems, and outlines therapeutic approaches for the different stages of disease, including metastatic melanoma.
The lifetime incidence of malignant melanoma in the United States increased from 1 in 1,500 persons in 1935 to 1 in 105 persons in 1991, an increase greater than that for any other major cancer [3]. Malignant melanoma is currently the eighth most prevalent cancer in the United States [1]. It is a disease affecting persons of all ages, with a median age at diagnosis in the mid-40s.
Exposure to sunlight is an important risk factor for the development of malignant melanoma. Intermittent exposure, especially early in life, seems to be more important than simple cumulative exposure [4]. It is speculated that increased recreational exposure to the sun has contributed to the rising incidence of melanoma.
Epidemiologic studies have identified certain phenotypic factors consistently associated with increased risk for the development of malignant melanoma. These factors include blue, green, or gray eyes; blond or red hair; light complexion; freckles; sun sensitivity; and the tendency to burn rather than tan. Other significant risk factors include a family history of melanoma, a personal history of nonmelanoma skin cancer, an increased number of melanocytic nevi, and xeroderma pigmentosum. Patients who have had one malignant melanoma are at increased risk for developing another; their risk is about 5%, compared with the approximately 1% lifetime risk of malignant melanoma in whites [5].
Some malignant melanomas arise in “precursor” pigmented lesions, while others arise in normal-appearing skin. Two types of pigmented lesions have been reported to be precursors for malignant melanoma: congenital melanocytic nevi and dysplastic nevi, better known today as atypical moles.
Congenital melanocytic nevi contain nevus cells and are present at birth. They occur in 1% of newborns and are usually small (less than 1.5 cm) or medium-sized (1.5 to 19.9 cm). Whether small or medium congenital melanocytic nevi are associated with an increased risk for melanoma is still controversial. On the other hand, large congenital melanocytic nevi (20 cm or greater) are associated with a 6% lifetime risk of developing melanoma [6].
Dysplastic nevi, or atypical moles, are acquired pigmented lesions of the skin that can occur in familial [7] and nonfamilial [8] settings. Patients with the dysplastic nevus syndrome have more than 100 moles, some of which have melanoma-like features (ie, asymmetry, border irregularity, and color variegation), and at least one mole larger than 8 mm in diameter [9]. The risk of malignant melanoma in people with this syndrome has been shown to be between 7- and 140-fold higher than that in the general population, with a family history of melanoma accounting for the higher figures [10]. Prospective close monitoring and early diagnosis may improve outcome in these high-risk individuals.
As the epidemiologic evidence indicates, there is definitely a genetic predisposition to malignant melanoma. In addition to polygenetic influences, there are also several syndromes of mendelian inheritance of a predisposition to melanoma. These syndromes include the classic familial atypical multiple mole melanoma (FAMMM) syndrome, non-FAMMM familial cutaneous malignant melanoma, xeroderma pigmentosum, and congenital nevocytic nevus syndrome [11]. Cannon-Albright et al demonstrated in a 1992 study that a series of kindreds with inherited malignant melanoma shared an abnormal genetic locus at the 9p13-p22 chromosomal region [12]. This same chromosomal region is frequently deleted or involved in translocations in sporadic melanomas. The locus has been mapped to the 9p21 area, cloned, and given the name multiple tumor-suppressor 1 (MTS1) gene [13]. This appears to be the same locus as a recently identified tumor-suppressor gene, p16 [14]. The search is ongoing for other single or multiple “melanoma susceptibility genes.”
Also of interest is work done to determine the genetic underpinnings of melanoma antigen expression. A recent article describes the mapping of the human melanoma antigen (MAGE) gene family to the chromosome region Xq27-qter. This finding raises the question of whether deletion of this gene in advanced melanoma might lead to resistance to immunotherapy [15]. It is hoped that research into the genetic determinants of melanoma will lead to advances in earlier diagnosis, targeted therapy, and gene therapy.
Melanocytes are cells of neural-crest origin that migrate to the skin and several other peripheral sites early during fetal development. They reside primarily in the basal layer of the epidermis and synthesize the pigment melanin, which is an important protective factor against the damaging effects of B-range ultraviolet light. Melanocyte-stimulating hormone is a pituitary hormone that supports the growth of melanocytes and causes increased production of melanin by the cells. The other major factor regulating melanocyte function is melatonin, an indole molecule that originates in the pineal gland and suppresses melanocyte function under conditions of decreased ambient light. Melanocytes respond to other paracrine growth factors as well, and malignant melanocytes produce growth factors themselves that may function in short autocrine loops to stimulate melanoma growth [16]. The neoplastic transformation of melanocytes gives rise to malignant melanoma.
A better understanding of melanoma biology was made possible in recent years by the development of tissue culture techniques and the establishment of cell lines from normal epidermal melanocytes and melanomas at different stages of progression [17]. It has been demonstrated that normal melanocytes require at least four mitogens to grow in culture media: insulin or insulin-like growth factor, fibroblast growth factor-alpha, melanocyte-stimulating hormone, and phorbol esters. In contrast, cell lines derived from intermediate stages of melanoma show successive loss of growth factor requirements, and metastatic melanomas proliferate in the absence of any exogenous proteins or phorbol esters [16]. These findings support the hypothesis that tumor cells produce autocrine growth factors and develop growth autonomy.
The importance of the microenvironment and cellular interactions in malignant melanoma biology has recently been recognized. Inhibition of growth of early-stage melanoma cell lines was observed when they were cocultured with dermal fibroblasts, whereas stimulation of growth was seen when cell lines derived from metastatic melanoma were cocultured with fibroblasts under the same conditions [18]. Identification of the factor or factors involved in modulating the growth of melanomas is an important area for research.
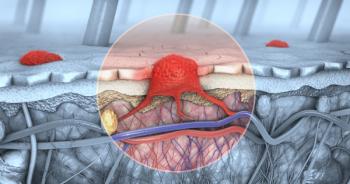
The mechanisms involved in melanoma invasion are being studied by several groups. Albelda et al [19] showed expression of the beta-3-integrin subunit by melanomas in vertical growth phase and by metastatic melanomas but not by benign melanocytes and radial-growth-phase melanomas. These data suggest the importance of integrin molecules in tumor invasion and their potential use as markers of melanoma cells entering the metastatic phase of tumor progression. Meissauer et al [20], utilizing specific inhibitors of the fibrinolytic system, provided evidence that urokinase-type and tissue-type plasminogen activators also play a role in malignant melanoma invasion in vitro. Besides integrins and plasminogen-activating factors, other membrane-bound proteases [21] and oligosaccharidic structures [22] have been shown to participate in tumor invasion and are potential targets for new therapeutic modalities.
Clinicians and researchers have long known that the interaction between the host immune system and melanoma is unique among human malignancies. The rare but intriguing phenomenon of spontaneous regression in malignant melanoma suggests an important role of the immune system in this disease. Histopathologic examination of primary (and sometimes metastatic) melanoma often reveals an active mononuclear inflammatory infiltrate and fibrosis. When these cells are invading within the melanoma mass, they are called tumor infiltrating lymphocytes (TIL). This phenomenon of an inflammatory infiltrate is sometimes called pathologic regression, and the prognostic importance of this finding is not yet clearly defined. Some evidence indicates that the presence of TIL may be a favorable prognostic factor in primary melanoma [23].
A very important issue in tumor immunology concerns the mechanisms of immune response and tumor strategies to escape the immune system's surveillance, and much of the important work in these areas has been carried out in melanoma models. Elegant experiments by Pandolfi et al demonstrated loss of expression of HLA-A2 antigens in two melanoma cell lines accompanied by a lack of immunologic recognition by autologous lymphocytes [24]. Transfection of HLA-A2 complementary DNA partially restored the ability of autologous lymphocytes to destroy the corresponding melanoma cells. This work illustrates one of the mechanisms by which malignant melanoma may escape the immunologic system of the host.
In animal models, the role of cytotoxic T lymphocytes and natural killer (NK) cells in preventing the establishment of metastatic disease has been well defined [25]. However, the role of these cells in the natural history of human melanoma is less certain. NK cells seem to be present in metastatic melanoma specimens more frequently than in primary lesions [26]. Defects in NK activity in patients with metastatic disease have been described [27], but a lack of correlation between NK activity and prognosis in melanoma patients also has been reported [28]. While HLA class I coexpression with cellular antigens is required for cytotoxic T-cell killing of melanoma cells, the ability of NK cells to kill melanoma is enhanced when down-regulation of class I antigens is induced by c-myc overexpression in melanoma cell lines [29,30]. Further investigation into the targets of both cellular and antibody-mediated immune responses to melanoma should lead to more sophisticated and less toxic treatment options.
Major Subtypes
Malignant melanoma has four major subtypes with unique clinical features [31].
Superficial spreading melanoma, which constitutes approximately 70% of melanomas, generally arises in a preexisting nevus. Early in its development, superficial spreading melanoma is a flat lesion with mixtures of deeply pigmented areas and amelanotic foci. As the lesion grows, the surface may become irregular, and the perimeter may show indentation.
Nodular Melanoma: The second most common pattern of growth (15% to 30%) is nodular melanoma. The lesion is typically blue-black and raised or dome-shaped, and it generally begins in uninvolved skin on the trunk, head, and neck areas. Nodular melanomas are more common in men and tend to arise in middle age. Five percent are amelanotic, and such lesions are frequently misdiagnosed. Nodular melanomas lack the radial growth phase typical of other melanomas and therefore have sharply demarcated borders. They are more aggressive and usually develop more rapidly than do superficial spreading melanomas.
Lentigo maligna melanoma, the third subtype, constitutes 4% to 10% of all melanomas and is typically located on the faces of older white women. The lesion's propensity to metastasize is small. In general, lentigo maligna melanomas are large (more than 3 cm), tan, flat lesions and are always associated with sun-related changes in the dermis and epidermis.
Acral Lentiginous Melanoma: The fourth type of malignant melanoma is the acral lentiginous variety. It occurs on the palms or soles or beneath the nail beds. However, not all plantar or solar melanomas are acral lentiginous lesions; a minority are superficial spreading or nodular melanomas. Acral lentiginous melanomas represent only 2% to 8% of melanomas in whites. In dark-skinned patients, such as blacks, Asians, and Hispanics, however, they account for 35% to 60% of melanomas. Acral lentiginous melanoma is primarily seen in older patients. Ulceration is commonly observed in this type of melanoma.
Of the four major subtypes of malignant melanoma, superficial spreading and lentigo maligna melanoma have the best survival rates, whereas nodular melanoma has the worst. However, when rates are adjusted for tumor thickness, there is no difference in 10-year survival rates between superficial spreading melanoma and nodular melanoma. The better prognosis associated with superficial spreading melanomas, therefore, seems to be related to the fact that they are thinner at the time of diagnosis. Lentigo maligna melanomas, on the other hand, have a better prognosis than the other growth patterns, even when matched by thickness [32].
Less Common Subtypes
Three less common types of malignant melanoma deserve mention here because of their distinctive clinical presentations and poor prognoses.
Desmoplastic Melanoma: The first is desmoplastic melanoma, a melanocyte-derived neoplasm of the skin involving the epidermis but with a predominantly dermal tumor focus. Desmoplastic melanoma lesions are frequently amelanotic, involve deeper structures of the dermis, and have a tendency to track along peripheral nerve sheaths [33]. Survival is worse than for the common cutaneous melanomas, because dissemination occurs early in the natural history of desmoplastic melanomas.
Uveal Melanoma: Another special type of melanoma is uveal (ocular) melanoma, a rare and clinically peculiar type of melanoma arising from the melanocytes of the pigmented uvea. This melanoma is curable when detected at an early stage. It may be observed when quite small, but at this stage is difficult to distinguish clinically from a benign nevus. Nonetheless, current opinion regards lesions greater than 2-mm thick as worrisome, and the smaller uveal melanoma lesions can be treated with local excision, photocoagulation, external-beam radiotherapy, or radioiodide plaque brachytherapy [34]. Enucleation is still recommended for larger lesions or when an increase in size or rate of growth is seen. Appropriate management of uveal nevi and small suspicious lesions requires frequent follow-up by a qualified ophthalmologist or ocular oncologist. Unfortunately, most of the time, uveal melanoma presents at a more advanced stage, has an extremely poor prognosis, and has a propensity to metastasize to the liver [35].
Mucosal Melanoma: The third clinically distinctive type of melanoma is the mucosal variant, which can arise in the mouth, anus, external or internal genital tract, upper respiratory tract, or elsewhere in the gastrointestinal tract. It also tends to present as advanced local disease and has an aggressive natural history leading to death. Mucosal melanomas seem to be less responsive to therapy than are the standard cutaneous types [36].
Malignant melanoma should be suspected in any pigmented skin or mucosal surface lesion that changes in color or size, begins to itch, or bleeds spontaneously. The clinical characteristics that suggest malignancy include variegation in color; acquisition of red, white, or blue color in a previously brown or black lesion; border irregularity; and surface elevation [37].
An elliptical excisional biopsy with a 2-mm margin of normal-appearing tissue is usually indicated for diagnostic purposes. Larger margins may be excessive for a benign condition and insufficient for treatment of a melanoma. Incisional or punch biopsies should be performed only when the amount of skin removed is critical because of lesion size or anatomic location. Such specimens should be taken from the clinically suspicious areas and should include a full thickness of skin and subcutaneous fat for adequate microstaging.
After a histopathologic diagnosis of malignant melanoma is made, the tumor must be staged to determine prognosis and treatment. Microstaging allows prognostic categorization of risk of relapse and survival. Tumor thickness is the single most important prognostic factor for patients with malignant melanoma limited to the primary site [38].
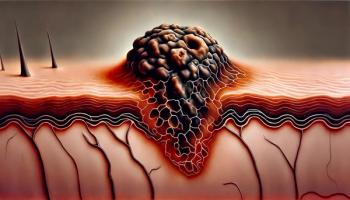
Clark's levels of microinvasion reflect increasing depth of tumor penetration into the dermal layers and the subcutaneous fat [39]. Clark's level I indicates melanoma in situ; level II, invasion of the papillary dermis; level III, invasion of the papillary-reticular dermal interface; level IV, frank invasion of the reticular dermis; and level V, invasion of the subcutaneous tissue. In Breslow's microstaging system, the thickness of the lesion is measured with an ocular micrometer to determine the maximal vertical thickness of the melanoma [40]. Both systems are predictive of the risk of metastasis, but data from several institutions have shown that Breslow's thickness is a relatively more accurate and reproducible parameter than is Clark's level of invasion.
Two staging systems are commonly used for malignant melanoma. A simple and widely used three-stage system developed by the World Health Organization (WHO) categorizes patients on the basis of nodal and distant metastasis [41]. Stage I applies to melanoma localized to the primary site, stage II indicates the presence of regional lymph-node metastases, and stage III indicates metastatic spread of disease to distant organs. However, this staging system, although easy to remember, does not take into account tumor thickness, which is an important prognostic factor in malignant melanoma. Another limitation is that 85% or more of newly diagnosed cases of melanoma fall into stage I.
In view of the limitations of the WHO staging system, the American Joint Committee on Cancer (AJCC) developed a four-stage system incorporating tumor thickness as part of the staging criteria and dividing clinically localized melanomas into two stages according to the microstaging information. This system allows for a better distribution of metastatic risk and survival among the defined groups [31]. Table 1 compares the WHO and the AJCC staging systems for malignant melanoma.
Table 2 shows the published survival rates for the various AJCC stages of malignant melanoma [31]. Survival relates directly to the eventual occurrence of disseminated disease and is not as yet thought to be influenced by treatment beyond surgical management of the primary lesion itself. It is hoped that treatment of advanced disease will be shown to affect survival in the future.
Survival can be predicted best by primary lesion thickness and by the presence of nodal or distant metastases as noted above, but some evidence suggests that measures of primary lesion progression, such as high mitotic rate, lack of tumor-infiltrating lymphocytes, and evidence of pathologic regression may influence prognosis independently [42]. Other well-known negative prognostic factors include ulceration of the primary lesion; location of the lesion on the head, neck, or back; and to a lesser extent, male sex.
Because surgical management of the primary lesion is the only treatment known to affect survival, proper local treatment is crucial. An important question in the management of primary cutaneous melanoma is the appropriate width of the margins of excision.
A randomized prospective study sponsored by the WHO Melanoma Programme showed similar rates of disease-free and overall survival for patients with melanomas thinner than 2 mm excised with narrow margins (1 cm) or wide margins (3 cm). However, 4 of 305 patients with tumors thicker than 1 mm treated with narrow margins had local recurrences. The authors concluded that narrow excision with 1-cm margins is safe for melanomas thinner than 1 mm [43].
Margins of 2 cm for tumors thicker than 1 mm have been shown in a large study by Balch et al to be adequate to control local recurrence, revising the previously held belief that margins of 3 to 5 cm were required for intermediate-thickness melanomas [44]. In this study, 486 melanoma patients with primary lesions between 1 and 4 mm thick were assigned randomly to receive 2- or 4-cm surgical margins. The outcomes in terms of local recurrence rate and development of in-transit metastases were not significantly different between the groups (0.8% vs 1.7% local recurrence and 2.1% vs 2.5% in-transit metastases, respectively). The best surgical margins for primary lesions thicker than 4 mm have yet to be determined, but for now, margins of 2 to 3 cm are considered prudent.
The role of prophylactic or elective lymph-node dissection in the management of primary malignant melanoma is controversial. Theoretically, removal of clinically normal lymph nodes bearing microscopic metastatic foci would improve prognosis. However, it is believed that patients with thick melanomas (greater than 4 mm) do not benefit from elective regional lymph-node dissection in view of the high likelihood that systemic metastasis has already occurred [45]. For thin melanomas (less than 1 mm), the low incidence of nodal metastasis does not justify the morbidity associated with lymph-node dissection [46]. However, for intermediate-thickness lesions (1 to 4 mm), nonrandomized studies have suggested a benefit from elective lymph-node dissection [47,48].
Prospective, randomized studies that included patients with all tumor thicknesses, however, have failed to demonstrate improved survival among patients treated with immediate prophylactic node dissection, compared with those who underwent therapeutic node dissection at the time of clinically evident nodal metastases [49]. Ongoing randomized trials of patients with stage I melanoma of intermediate thickness should clarify the role of elective lymph-node dissection [50].
In the meantime, an interesting new tool is available to help with the management of regional lymph nodes. A technique called sentinel lymph-node mapping and resection has been described by Morton et al [51]. The draining lymphatic vessels from a high-risk primary melanoma are identified by injecting dyes such as isosulfan blue and patent blue-V. The “sentinel” (first) lymph node that takes up the dye is surgically removed and subjected to histologic analysis. If this node is not involved with melanoma, there is a less than 5% chance that any lymph nodes in that drainage site are pathologically involved. This technique, after further study, may prove to be the best way to determine optimal surgical management of intermediate- and high-risk primary melanomas of the extremities with clinically uninvolved draining lymph nodes.
Patients with metastatic involvement of the regional lymph nodes are best treated with therapeutic lymphadenectomy. Unfortunately, 60% to 70% of these patients will eventually have relapses, mainly in distant sites. Several adjuvant strategies have been employed in an attempt to improve the prognosis of these and other high-risk melanoma patients. As yet, they have not proved successful.
Levamisole (Ergamisol), a nonspecific immunostimulant, has been studied in the adjuvant setting with conflicting results. A randomized trial sponsored by the National Cancer Institute of Canada compared this agent alone, oral bacillus Calmette-Gurin (BCG) alone, BCG alternating with levamisole, and a no-adjuvant-treatment control arm. Compared with the control arm, patients treated with adjuvant levamisole showed a 29% reduction in recurrence and death [52]. This result contrasts with a randomized study by Spitler involving similar categories of patients but indicating that levamisole was ineffective as an adjuvant to surgery in high-risk patients with malignant melanoma [53].
Among many negative studies of adjuvant chemotherapy or immunotherapy, a large randomized trial by the WHO Melanoma Programme did not show a benefit in terms of disease-free or overall survival from adjuvant dacarbazine, BCG, or both when compared with surgery alone for WHO stage II melanoma of any anatomic location and stage I melanoma of the trunk [54]. One prospective, nonrandomized trial of adjuvant therapy with the investigational agent vindesine (Eldisine) demonstrated a benefit in terms of disease-free survival and median survival in those receiving the drug after surgical lymphadenectomy, but the outcome in control patients was worse than expected [55]. One prospective, controlled, nonrandomized study of adjuvant chemohormonal therapy with tamoxifen, dacarbazine, cisplatin (Platinol), and carmustine (BiCNU) in 18 patients with high-risk stage III or completely resected stage IV disease showed no survival advantage in the treated patients, but showed a trend toward longer median disease-free survival [56].
A polyvalent melanoma vaccine has also been studied in the adjuvant setting [57], where it was shown in 55 stage II and stage III patients to be safe and to induce an immune response, but numbers were not large enough to assess treatment efficacy.
The use of isolated regional limb perfusion with melphalan (Alkeran) has also been studied in the adjuvant setting with conflicting results [58]. Multiple studies using normothermic and hyperthermic techniques showed slightly better disease-free survival than in historical controls, but there have been no randomized studies. In recent years, this technique has been studied more frequently for local recurrence, with encouraging results [59,60]. There are still no randomized studies, however. Technical complexity and expense make this treatment difficult to recommend without better data on efficacy.
The role of alpha interferon (IFN-alfa) in patients with surgically resected locoregional melanoma is being studied in two prospective, controlled randomized trials. A trial undertaken by the Eastern Cooperative Oncology Group using IFN-alfa at a dose of 20 million U/m²/d given intravenously 5 days a week for 1 month, followed by 10 million U/m²/d given subcutaneously 3 days a week for 11 months in patients with resected stage II or stage III disease has shown preliminary evidence of a modest benefit [61]. However, toxicity has been high in this trial. In contrast, a WHO study using IFN-alfa at a dose of 3 million U given subcutaneously three times per week for 3 years in stage III patients has reported no significant toxicity [62]. Preliminary results of this study also show a modest benefit in prolonging the time to disease progression.
Until these studies are published in peer-reviewed journals, the standard of care for patients with high-risk locoregional disease after definitive surgical treatment is still observation alone, because no form of adjuvant systemic or regional treatment has been established to have a beneficial role in prolonging survival. Patients at high risk for relapse should be encouraged to participate in clinical trials.
Malignant melanoma can metastasize to almost any organ in the body. The survival time for patients with metastatic disease ranges from 6 to 9 months when metastases are detected in multiple organ sites. Patients with metastases to skin, subcutaneous tissue, or distant lymph nodes have the longest survival, averaging 12 to 15 months. After regional lymph nodes, the lungs are the second most frequent initial site of relapse; patients with lung metastases have a median survival of 11 months. Patients with liver, brain, or bone metastases have a median survival of only 3 to 4 months [31].
Surgical removal of metastatic deposits can play an important role in the management of disseminated melanoma. The goal of surgical excision may be to render a patient free of disease by removing a solitary mass after systemic therapy or to provide relief from symptomatic disease in the palliative setting. In several series, resection of isolated metastases to the brain, lungs, gastrointestinal tract, skin, or subcutaneous tissues has resulted in overall 2-year survival rates ranging from 15% to 30% in selected patients, with some long-term survivors, especially among patients with solitary lung metastases [31].
Radiotherapy plays a limited role in the management of metastatic melanoma. It is used mainly for palliation of central nervous system metastases or painful bone metastases and for control of pain and bleeding from recurrent unresectable cutaneous or lymph-node masses. More recently, use of the cobalt-60 gamma unit (“gamma knife”) has shown encouraging results for long-term local control of brain metastases smaller than 2.5 to 3.0 cm in diameter [63].
Single-Agent Chemotherapy
The only single agent approved for the treatment of melanoma is dacarbazine, which provides response rates of 15% to 20% but results in complete remission in less than 5% of treated patients. Responses have been observed mainly in soft tissues, ie, skin, subcutaneous tissue, lymph-node, and lung metastases, which are more responsive than metastatic deposits in the bones, liver, or central nervous system (these respond in less than 10% of patients). The responses obtained with this agent are usually short-lived, ranging from 3 to 6 months. Consequently, patients treated with dacarbazine have not experienced a significant increase in survival, which has generally ranged between 4 and 6 months [64-66].
The nitrosoureas also have a significant but low level of antitumor activity in melanoma, with response rates around 15% [65,67]. This group of drugs includes carmustine, lomustine (CeeNu), and semustine (MeCCNU). Patients previously exposed to dacarbazine have an even lower rate of response to the nitrosoureas than untreated patients [65]. Fotemustine, a new nitrosourea, has recently been studied in Europe. A multicenter phase II study of 153 evaluable patients showed a 30% response rate in previously untreated patients and 24% overall. Responses were also observed in patients with brain metastases from melanoma [68].
Other classes of chemotherapeutic agents with a low level of activity-10% to 20%-include the vinca alkaloids [69,70] and platinum compounds such as cisplatin and carboplatin [71-73]. The chemoprotectant agent ethiofos (WR-2721) may enhance the therapeutic index of platinum compounds, accounting for the total response rate of 53% in one small study (which has not been confirmed)[74].
Paclitaxel (Taxol), a new agent that acts on the microtubule assembly, has recently been studied in phase II trials [75,76]. Three complete responses and four partial responses were observed among 53 melanoma patients. Further exploration of this agent for the treatment of malignant melanoma may be warranted.
A new lipid-soluble dihydrofolate reductase inhibitor, piritrexim isethionate (taken orally), produced a response rate of 23% in 31 evaluable patients [77]. Interestingly, responses were seen in previously treated patients as well as in previously untreated patients. Piritrexim appears to be more active than methotrexate and deserves further investigation in the treatment of melanoma.
Combination Chemotherapy
Based on the independent activity of dacarbazine and the nitrosoureas, several studies combining the two types of agents were performed in the late 1970s. However, these studies failed to show superiority of the combination over dacarbazine alone [65,78]. Dacarbazine has also been combined with dactinomycin (Cosmegen) [79], vinca alkaloids [80], cisplatin [81], and fotemustine [82]. The observed response rates with the two-drug combinations have ranged from 20% to 25%, which are not significantly superior to the rate with dacarbazine alone. The exception is fotemustine, which produced a response rate of 33% when combined with dacarbazine. Table 3 summarizes the results with selected two-drug combination regimens that include dacarbazine.
Combinations of three or more drugs, with or without dacarbazine, have also been investigated. A three-drug combination regimen of carmustine, hydroxyurea, and dacarbazine tested by the Southwest Oncology Group produced an overall response rate of 27% in 178 patients, with response duration averaging 6 months [83]. A regimen combining bleomycin (Blenoxane), vincristine (Oncovin), lomustine, and dacarbazine (BOLD), developed in the late 1970s at Duke University, produced a 40% total response rate, with a 9% complete response rate in 91 previously untreated patients [84]. Subsequent studies of the BOLD regimen have had less impressive results, with total response rates ranging from 4% to 20% [85,86]. However, one European study that substituted vindesine for vincristine demonstrated a response rate of 41% [87].
A number of combination chemotherapy regimens without dacarbazine were studied in the late 1970s and early 1980s. The most promising was a combination of bleomycin, vinblastine, and cisplatin, which produced response rates ranging from 22% to 43% in several trials [88,89].
Most recently, several groups have reported activity with a combination of dacarbazine, cisplatin, and a vinca alkaloid (either vinblastine or vindesine)[90-93]. The response rates achieved with this three-drug combination have ranged from 24% to 45%, which are superior to those reported with dacarbazine alone. However, formal prospective, controlled studies have not been performed to confirm the apparent superiority of this regimen. Results with selected multiagent chemotherapy regimens are summarized in Table 4.
Hormonal Therapy
Hormonal manipulation in melanoma has been studied since the 1970s. The role of tamoxifen in the treatment of melanoma is controversial. As a single agent, this nonsteroidal antiestrogen has produced an objective response rate of only 6% [94]. However, a recent Italian study [95] comparing dacarbazine alone with the combination of dacarbazine and tamoxifen for metastatic melanoma reported a superior response rate (28% vs 12%) and longer median survival (48 weeks vs 29 weeks) favoring the chemohormonal arm. The additional benefit of tamoxifen was seen primarily among women.
Similarly, a regimen of tamoxifen, dacarbazine, carmustine, and cisplatin first studied in 1984 showed a response rate of 55% and a complete response rate of 20% in 20 patients with metastatic disease [96]. In addition, a report from McClay et al [97] showed a higher response rate with this combination (51%) than with the chemotherapy agents alone (10%). However, the survival rates were not significantly different in this trial because of early relapse in the central nervous system in the responding patients. This regimen, initially developed at Dartmouth University (hence, the Dartmouth regimen), is used quite widely in the community because of its high response rate in the initial studies. It has also been shown to produce a high response rate (55%) in patients with metastatic disease that progressed after prior therapy with interleukin-2 (IL-2, aldesleukin [Proleukin])[98].
Another trial assessed the effectiveness of tamoxifen added to high-dose cisplatin and dacarbazine but failed to show an additional benefit [99]. Trials of combination chemotherapy and tamoxifen are shown in Table 5 [100].
Megestrol acetate was added to the Dartmouth regimen in one trial and produced a total response rate of 47% in 19 patients [101]. The rationale for using megestrol in this trial was the possible abrogation of chemotherapy resistance and prevention of treatment-related cachexia.
Another hormonal maneuver that has been studied is daily oral melatonin, the melanocyte-suppressive hormone of pineal origin that has been shown to have growth-suppressive, immune-stimulatory, and oncostatic properties in animal models. Melatonin treatment produced a 15% response rate with no toxic effect except fatigue in 40 patients with metastatic disease [102]. This interesting drug deserves further investigation, especially as a modulator of chemotherapy response.
High-Dose Chemotherapy With Autologous Bone Marrow Transplantation
High-dose chemotherapy with either single or multiple agents followed by autologous bone marrow transplantation for metastatic melanoma has produced high rates of response, ranging from 20% to 81% [103-105]. Complete response rates have ranged from 0% to 6%, with some additional patients being rendered free of disease after surgical resection of isolated sites of disease. However, the responses have been short-lived, with very few long-term survivors, and the treatment is accompanied by severe toxic effects and even death.
This treatment strategy has also been used in the adjuvant setting after lymphadenectomy in a randomized trial of immediate treatment with high-dose cyclophosphamide (Cytoxan, Neosar), cisplatin, and carmustine with marrow rescue, compared with the same treatment at the time of relapse, in 39 patients with high-risk regional disease [106]. Median time to progression was prolonged in the immediate treatment group, but median survival did not differ between the two groups.
Use of growth factors may reduce the toxicity associated with high-dose chemotherapy treatment and also may support dose escalation without bone marrow transplantation.
Biologic Therapy
Nonspecific immunotherapy, including BCG and Corynebacteriumparvum treatments, has been used for decades in the treatment of malignant melanoma, although it has had only minimal impact on the natural history of the disease. Recently, the availability of lymphokines, such as the interferons and IL-2, produced by means of recombinant DNA technology, has rekindled interest in biologic therapy (immunotherapy) for malignant melanoma and other neoplasms.
Interferons: Initial studies of partially purified human leukocyte-derived interferon showed that it stimulated T-helper/inducer subsets of lymphocytes and increased NK cell activity [107] but had only minimal activity against melanoma. Subsequently, several groups studied recombinant interferons alfa-2a (Roferon-A) and alfa-2b (Intron A) at different dosages and schedules for the treatment of advanced melanoma, and observed response rates of 10% to 20% [78]. Four large studies of interferon in patients with advanced melanoma are summarized in Table 6 [108,109]. The response rates in untreated patients ranged from 8% to 22%, which is similar to the activity produced by dacarbazine. However, interferon's well-known systemic toxicity limits its use in patients already debilitated by cancer.
Studies from The University of Texas M.D. Anderson Cancer Center showed that more than half of patients cannot tolerate interferon doses larger than 20 million U/m²/d. Lower doses of 10 million U/m² given three times a week were shown to have equal activity but to be better tolerated [110]. The greatest antitumor effects of interferon were obtained with long-term administration on a daily or three-times-weekly basis, whereas very few patients responded to once-weekly doses or 5-day courses every 3 weeks [78].
Interferon has been used with equal efficacy in previously untreated and previously treated patients, in whom alternative chemotherapy is rarely effective. In a small proportion of melanoma patients, the disease has been controlled with interferon for periods in excess of 2 to 3 years [111]. The frequency of response to interferon is somewhat higher for soft-tissue metastases than for disease at other distant sites. Nonetheless, responses have been observed in lung and liver metastases as well.
Interleukin-2: The second biologic agent to show activity against metastatic melanoma was IL-2, a cytokine also known as T-cell-derived growth factor, which mediates the activation and expansion of effector lymphocytes after antigen exposure. In initial studies performed at the National Cancer Institute, six partial responses were obtained among 23 patients treated with IL-2 alone [112]. The combination of IL-2 with lymphokine-activated killer (LAK) cells, which are autologous lymphocytes activated by IL-2 ex vivo, resulted in three complete responses and three partial responses among 34 patients with metastatic disease [112]. More recent trials using bolus doses of IL-2 obtained modest response rates of 16% to 22%, which are not superior to the activity of single-agent chemotherapy. Table 7 summarizes trials using IL-2 alone and in combination with LAK cells for advanced melanoma [113-115].
The bolus administration of IL-2 in initial trials was accompanied by severe toxic effects. Constitutional symptoms, capillary leak syndrome, and deaths occurred [113]. Continuous infusion of IL-2 was associated with decreased toxicity, and apparently maintained IL-2's potent immunomodulatory effects and ability to induce clinical responses. The continuous infusion schedule is therefore preferred, and the usual dose is 12 to 18 million IU/m²/d for 5 days.
IFN-alfa and IL-2 have also been used in combination by some investigators. In 1992, Sznol et al reported on the use of combined IL-2/LAK cells and IFN-alfa as immunomodulation along with low-dose cyclophosphamide and doxorubicin (Adriamycin, Rubex) in 40 patients with metastatic disease. There were six responders, but only one response was long-term [116].
Keilholz et al compared two dosing schedules of IFN-alfa followed by IL-2 in 54 patients [117]. They found an improved response rate (41% vs 18%) when the IL-2 infusion was “front-loaded,” ie, given as a peaking high-dose infusion over the first 42 hours with very-low-dose infusion for the rest of the 5 days, as opposed to being given as a constant-dose 5-day infusion. The toxicity of IL-2 was also reduced when given in this fashion.
Home subcutaneous therapy with IL-2 and IFN-alfa has also been attempted, with quite mild toxic effects, but tumor responses in the heavily pretreated patients were disappointing [118]. A phase III randomized trial reported in 1993 compared high-dose bolus IL-2 alone with the same IL-2 dose combined with concurrent IFN-alfa. This trial demonstrated low response rates not improved by the addition of IFN-alfa (5% vs 10% in the IL-2 and IL-2-plus-IFN-a groups, respectively) in 85 patients with advanced melanoma [119]. Overall, the results with cytokine therapy for metastatic melanoma have not been significantly better than those with combination chemotherapy.
Biochemotherapy
The term biochemotherapy applies to the combined use of biologic and chemotherapeutic agents. This treatment strategy has been studied with the hope that the two treatments used sequentially or concurrently might improve the response rates achieved with either therapy alone, without excessive additional toxicity.
The initial studies of biochemotherapy for malignant melanoma combined the most active chemotherapy agent, dacarbazine, with IFN-alfa. In a trial reported by Bajetta et al, among 75 evaluable patients with metastatic melanoma, 8% complete responses and 17% partial responses were observed, suggesting improved activity with the combination [120]. In contrast, an international multicenter randomized trial comparing the combination of IFN alfa-2b and dacarbazine with either agent alone was not able to confirm the superiority of the combined treatment over dacarbazine alone. However, the trial was closed prior to full patient accrual [121].
A recently reported Australian multicenter randomized trial also failed to show a superior response rate with the combination of dacarbazine and IFN-alfa over dacarbazine alone [122]. In contrast to these negative results, a trial conducted in South Africa by Falkson et al obtained a notable response rate of 53% with combined dacarbazine and IFN alfa-2b [123]. In this trial, IFN alfa-2b was given intravenously 5 days a week for 3 weeks prior to starting dacarbazine, and then subcutaneously three times a week along with dacarbazine at a standard dosage. Median time to treatment failure and median survival were significantly longer with the biochemotherapy combination than with dacarbazine alone. Most important, a recently published multicenter randomized trial with 236 patients compared dacarbazine alone with dacarbazine and two different doses of IFN-alfa [124]. The response rates, in the range of 25%, did not differ among the arms, but response duration was longer in the IFN-alfa groups.
Stoter et al [125] and Flaherty et al [126] used a similar strategy with dacarbazine and IL-2, and demonstrated response rates of 24% in 25 patients [125] and 22% in 32 patients [126]. More disappointing results were seen in a Southwest Oncology Group study using this combination, which produced no responses in 13 patients [127], and in a trial by Fiedler et al, which produced two responses in 16 patients [128]. LAK cells added to this treatment strategy did not produce a more favorable response rate [129]. However, a trial by Khayat et al combining IFN-alfa and IL-2 with cisplatin did achieve a better response rate in 39 patients, with a 12% complete response rate and a 54% total response rate [130]. Lastly, the addition of intravenous BCG or C parvum extract to combination chemotherapy also has failed to produce a greater benefit [131,132].
In summary, inconsistent clinical results have been seen with the addition of immunotherapy to single-agent chemotherapy. Overall, no additive benefit has been demonstrated, especially in the one large randomized trial [124].
Because of these less than satisfactory results, a more intensive approach incorporating IL-2 and IFN-alfa with multiagent chemotherapy has recently been studied by several groups. At M.D. Anderson Cancer Center, since October 1990 we have been studying IL-2 and IFN-alfa given alternately or concurrently with the combination of cisplatin, vinblastine, and dacarbazine (CVD) for patients with metastatic malignant melanoma. Although administration of IL-2 by continuous infusion requires hospitalization, the CVD chemotherapy can be given in the outpatient clinic. Among 30 evaluable patients, preliminary results were 6 complete responses and 11 partial responses, for an overall response rate of 56% [133]. Since that time, a total of 155 patients have been treated with either sequential or concurrent biochemotherapy, with a complete response rate of 17% and a total response rate of 55% [134]. This regimen has been accompanied by severe multisystem toxicity, including myelosuppression, capillary leak syndrome, and renal and gastrointestinal toxic effects, limiting its applicability only to patients who have good performance status.
Results of a similar approach using sequential chemotherapy and immunotherapy were reported by the University of Chicago group. The chemotherapy regimen comprised carmustine, dacarbazine, cisplatin, and tamoxifen. IL-2 was given on a bolus schedule along with IFN alfa-2a. The reported response rate in 42 consecutive patients was 57%, with a complete response rate of 24% [135].
Another biochemotherapy regimen using cisplatin and dacarbazine with high-dose IL-2 given in the inpatient setting achieved a complete response rate of 8% and a total response rate of 42% in 38 patients [136], and a strategy using the same chemotherapy and IL-2 given in an outpatient setting produced very similar results (response rate, 42%; complete response rate, 9%)[137]. Lastly, the protocol of Khayat et al used in 39 heavily pretreated patients could be considered as aggressive as these regimens, with a similar high response rate [132]. These aggressive regimens seem to increase complete and overall response rates significantly with only moderate and mostly manageable additional toxic effects. However, a survival benefit has not yet been shown conclusively. Table 8 summarizes the results of the major biochemotherapy studies.
Melanoma Vaccines and Monoclonal Antibodies
Vaccine therapy can be categorized into several types, including autologous melanoma cell preparations, allogeneic cell fraction preparations, purified melanoma antigens, and anti-idiotypic antibodies, which mimic melanoma antigens. Another consideration is the carrier or adjuvant in which the vaccine is delivered. Vaccine development for melanoma and other malignant tumors has progressed steadily in recent years, but a definite clinical benefit has yet to be demonstrated.
Morton et al have published the results of their whole-cell, polyvalent, allogeneic melanoma cell vaccine with BCG as an adjuvant in 136 patients [138]. Among 40 patients with evaluable disease, there were nine responders. The treated patients had a longer median survival than did historical controls, and survival was correlated with measures of an immune response to the vaccine.
An autologous vaccine studied in 64 patients by Berd et al was given after a cyclophosphamide dose, with BCG used as an adjuvant [139]. The response rate was 12%, and response correlated with the development of a cellular immune response to the vaccine. Some patients responded after initial disease progression.
Mitchell et al used an allogeneic lysate vaccine and a novel adjuvant called DETOX in 20 patients with metastatic disease, and demonstrated a 16% response rate [140].
Anti-idiotypic antibodies (monoclonal antibodies directed against the variable region of antimelanoma antigen antibodies, thereby mimicking the antigen itself) have also been used as vaccines, with little toxicity and demonstration of a humoral immune response, but low response rates [141]. In addition to the anti-idiotypic antibodies, other monoclonal antibodies have been used as well [142]. Most of these agents have been directed against glycolipid antigens, which are preferentially expressed on melanocytes and melanoma. Some responses have been seen, and toxicity has not been a major problem. Further work is in progress.
Despite rapid advances in our understanding of melanoma, there are still many more questions than answers. There is still no standard adjuvant treatment for patients with high-risk primary melanoma or effective treatment of newly diagnosed metastatic disease. It is hoped that improved treatment options will come with continued basic science investigation and well-designed clinical trials to test the efficacy of new regimens and compare results of alternative therapies.
An important issue likely to be resolved by ongoing trials is whether adjuvant IFN-alfa will decrease relapse rates and increase survival for patients with intermediate- and high-risk locoregional melanoma. Another crucial question, currently being studied at M.D. Anderson Cancer Center, is whether aggressive neoadjuvant biochemotherapy will improve outcome for high-risk patients with locoregional disease. The appropriate role of vaccines and the tools to assess immunologic responses are still being defined. The development of new pharmacologic agents using the molecular-mechanistic approach holds promise. Finally, gene therapy for melanoma, though still in the early stages of development, may allow a less toxic, more specific alternative to today's cytotoxic and biologic treatments.
Despite substantial improvements in survival rates in recent decades, the incidence of malignant melanoma and the associated absolute mortality are rising. The increase in survival is attributable entirely to earlier diagnosis. Efforts to treat metastatic disease have had minimal impact on survival. Initial excitement created by the first results with biologic therapy has been tempered by associated severe toxicities. Ongoing clinical research in the areas of biochemotherapy, melanoma vaccines, and new cytotoxic drugs offers hope of better therapy in the near future.
Recent developments in the understanding of tumor biology may someday translate into a significant benefit for patients. For now, efforts should be focused on primary prevention-avoidance of excessive solar exposure and use of sun protection-and secondary prevention programs emphasizing the importance of early diagnosis. Patients with advanced disease should be encouraged to participate in clinical trials.
References:
1. Wingo P, Tong T, Bolden S: Cancer statistics, 1995. CA Cancer J Clin 45:8â30, 1995.
2. Sober A: Cutaneous melanoma: Opportunity for cure. CA Cancer J Clin 41:197â199, 1991.
3. Ries L, Hankey B, Miller B, et al: Cancer Statistics Review 1973â1988. Bethesda, Md, National Cancer Institute, 1991.
4. Lew R, Sober A, Cook N, et al: Sun exposure habits in patients with cutaneous melanoma: A case control study. J Dermatol Surg Oncol 9:981â986, 1983.
5. Friedman R, Rigel D, Silverman M, et al: Malignant melanoma in the 1990s: The continued importance of early detection and the role of physician examination and self-examination of the skin. CA Cancer J Clin 41:201â226, 1991.
6. Rhodes A, Wood W, Sober A, et al: Non-epidermal origin of malignant melanoma associated with a giant congenital nevocellular nevus. Plast Reconstr Surg 67:782â790, 1981.
7. Clark WJ, Reimer R, Greene M, et al: Origin of familial malignant melanoma from heritable melanocytic lesions: “The B-K mole syndrome.” Arch Dermatol 114:732â738, 1978.
8. Elder D, Goldman L, Goldman S, et al: Dysplastic nevus syndrome: A phenotypic association of sporadic cutaneous melanoma. Cancer 46:1787â1794, 1980.
9. Tiersten A, Grin C, Kopf A, et al: Prospective follow-up for malignant melanoma in patients with the atypical-mole (dysplastic nevus) syndrome. J Dermatol Surg Oncol 17:44â48, 1991.
10. Hoffman S, Yohn J, Robinson W, et al: Melanoma: 1. Clinical characteristics. Hosp Pract 15:35â46, 1994.
11. Lynch H, Fusaro R: Hereditary malignant melanoma: A unifying etiologic hypothesis. Cancer Genet Cytogenet 20:301â304, 1986.
12. Cannon-Albright L, Goldgar D, Meyer L, et al: Assignment of a locus for familial melanoma, MLM, to chromosome 9p13-p22. Science 258:1148â1152, 1992.
13. Hussussain C, Struewing J, Goldstein A, et al: Germline p16 mutations in familial melanoma. Nat Genet 8:15â21, 1994.
14. Kamb A, Gruis N, Weaver-Feldhaus J, et al: A cell cycle regulator potentially involved in genesis of many tumor types. Science 264:436â440, 1994.
15. Oaks M, Hanson JJ, O'Malley D: Molecular cytogenetic mapping of the human melanoma antigen to chromosome Xq27-qter: Implications for MAGE immunotherapy. Cancer Res 54:1627â1629, 1994.
16. Rodeck U, Herlyn M: Growth factors in melanoma. Cancer Met Rev 10:89â101, 1991.
17. Menrad A, Herlyn M: Tumor progression, biology and host response in melanoma. Curr Opin Oncol 4:351â356, 1992.
18. Cornil I, Theodorescu D, Man S, et al: Fibroblast cell interactions with human melanoma cells affect tumor cell growth as a function of tumor progression. Proc Natl Acad Sci USA 88:6028â6032, 1991.
19. Albelda S, Mette S, Elder D, et al: Integrin distribution in malignant melanoma: Association of the beta-3 subunit with tumor progression. Cancer Res 50:6757â6764, 1990.
20. Meissauer A, Kramer M, Hofmann M, et al: Urokinase-type and tissue-type plasminogen activators are essential for in vitro invasion of human melanoma cells. Exp Cell Res 192:453â459, 1991.
21. Aoyama A, Chen W-T: A 170-kDa membrane-bound protease is associated with the expression of invasiveness by human malignant melanoma cells. Proc Natl Acad Sci USA 87:8296â8300, 1990.
22. Seftor R, Seftor E, Grimes W, et al: Human melanoma cell invasion is inhibited in vitro by swainsonine and deoxymannojirimycin with a concomitant decrease in collagenase IV expression. Melanoma Res 1:43â45, 1991.
23. Mackensen A, Carcelain G, Viel S, et al: Direct evidence to support the immunosurveillance concept in a human regressive melanoma. J Clin Invest 93:1397â1402, 1994.
24. Pandolfi F, Boyle L, Trentin L, et al: Expression of HLA-A2 antigen in human melanoma cell lines and its role in T-cell recognition. Cancer Res 51:3164â3170, 1991.
25. Markovic S, Murasko D: Role of natural killer and T-cells in interferon induced inhibition of spontaneous metastases of the B16F10L murine melanoma. Cancer Res 51:1124â1128, 1991.
26. Kornstein M, Stewart R, Elder D: Natural killer cells in the host response to melanoma. Cancer Res 47:1411â1412, 1987.
27. Muller C, Pehamberger H, Binder M, et al: Defective interferon-augmented natural killer cell activity in patients with metastatic malignant melanoma. J Cancer Res Clin Oncol 115:393â396, 1989.
28. Hersey P, Edwards A, Milton G, et al: No evidence for an association between natural killer cell activity and prognosis in melanoma patients. Nat Immun Cell Growth Reg 3:87â94, 1984.
29. Peltenburg L, Steegenga W, Kruse K, et al: c-myc-induced natural killer cell sensitivity of human melanoma cells is reversed by HLA-B27 transfection. Eur J Immunol 22:2737â2740, 1992.
30. Versteeg R, Peltenburg L, Plomp A, et al: High expression of the c-myc oncogene renders melanoma cells prone to lysis by natural killer cells. J Immunol 143:4331â4337, 1989.
31. Balch C, Houghton A, Peters L: Cutaneous melanoma, in DeVita VT Jr, Hellman S, Rosenberg SA (eds): Cancer: Principles and Practice of Oncology, 4th ed, pp 1612â1614. Philadelphia, JB Lippincott, 1993.
32. Urist M, Balch C, Soong S-J, et al: Head and neck melanoma in 536 clinical stage I patients: A prognostic factors analysis and results of surgical treatment. Ann Surg 200:769â775, 1984.
33. Jain S, Allen P: Desmoplastic malignant melanoma and its variants. Am J Surg Pathol 13:358â373, 1989.
34. Hungerford J: Uveal melanoma. Eur J Cancer 29A:1368â1372, 1993.
35. Shields J: Management of uveal melanoma: A continuing dilemma. Cancer 72:2067â2068, 1993.
36. Cooper P, Mills S, Allen M: Malignant melanoma of the anus: Report of 12 patients and analysis of 255 additional cases. Dis Colon Rectum 25:693â703, 1982.
37. Wick M, Sober A, Fitzpatrick T, et al: Clinical characteristics of early cutaneous melanoma. Cancer 45:2684â2686, 1980.
38. Balch C, Soong S-J, Shaw H, et al: An analysis of prognostic factors in 8500 patients with cutaneous melanoma, in Balch C, Houghton A, Milton G, et al (eds): Cutaneous Melanoma, 2nd ed, pp 165â187. Philadelphia, JB Lippincott, 1992.
39. Clark WJ, From L, Bernardino E, et al: The histogenesis and biologic behavior of primary human malignant melanomas of the skin. Cancer Res 29:705â726, 1969.
40. Breslow A: Thickness, cross-sectional areas and depth of invasion in the prognosis of cutaneous melanoma. Ann Surg 182:572â575, 1975.
41. Goldsmith H: Melanoma: An overview. CA Cancer J Clin 29:194, 1979.
42. Clark WJ, Elder D, DuPont GI, et al: Model predicting survival in stage I melanoma based on tumor progression. J Natl Cancer Inst 81:1893â1904, 1989.
43. Veronesi U, Cascinelli N: Narrow excision (1-cm margin): A safe procedure for thin cutaneous melanoma. Arch Surg 126:438â441, 1991.
44. Balch C, Urist M, Karakousis C, et al: Efficacy of 2-cm surgical margins for intermediate-thickness melanomas (1 to 4 mm): Results of a multi-institutional randomized surgical trial. Ann Surg 218:262â267, 1993.
45. Crowley N, Seigler H: The role of elective lymph node dissection in the management of patients with thick cutaneous melanoma. Cancer 66:2522â2527, 1990.
46. Balch C: The role of elective lymph node dissection in melanoma: Rationale, results, and controversies. J Clin Oncol 6:163â172, 1988.
47. Balch C, Soong S-J, Milton G, et al: A comparison of prognostic factors and surgical results in 1,786 patients with localized (stage I) melanoma treated in Alabama, USA, and New South Wales, Australia. Ann Surg 196:677â684, 1982.
48. Drepper H, Kohler C, Bastian B, et al: Benefit of elective lymph node dissection in subgroups of melanoma patients: Results of a multicenter study of 3616 patients. Cancer 72:741â749, 1993.
49. Sim F, Taylor W, Pritchard D, et al: Lymphadenectomy in the management of stage I malignant melanoma: A prospective randomized study. Mayo Clin Proc 61:697â705, 1986.
50. Cady B: “Prophylactic” lymph node dissection in melanoma: Does it help? J Clin Oncol 6:2â4, 1988.
51. Morton D, Wen D, Wong J, et al: Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 127:392â399, 1992.
52. Quirt I, Shelley W, Pater J, et al: Improved survival in patients with poor-prognosis malignant melanoma treated with adjuvant levamisole: A phase III study by the National Cancer Institute of Canada clinical trial group. J Clin Oncol 9:729â735, 1991.
53. Spitler L: A randomized trial of levamisole versus placebo as adjuvant therapy in malignant melanoma. J Clin Oncol 9:736â740, 1991.
54. Veronesi U, Adamus J, Aubert C, et al: A randomized trial of adjuvant chemotherapy and immunotherapy in cutaneous melanoma. N Engl J Med 307:913â916, 1982.
55. Retsas S, Quigley M, Pectasides D, et al: Clinical and histologic involvement of regional lymph nodes in malignant melanoma: Adjuvant vindesine improves survival. Cancer 73:2119â2130, 1994.
56. Saba H, Cruse C, Wells K, et al: Adjuvant chemotherapy in malignant melanoma using dacarbazine, carmustine, cisplatin, and tamoxifen regimens: A University of South Florida and H. Lee Moffitt Melanoma Center study. Ann Plast Surg 28:60â64, 1992.
57. Bystryn J-C, Oratz R, Harris M, et al: Immunogenicity of a polyvalent melanoma vaccine in humans. Cancer 61:1065â1070, 1988.
58. Cumberlin R, De Moss E, Lassus M, et al: Isolation perfusion for malignant melanoma of the extremity: A review. J Clin Oncol 3:1022â1031, 1985.
59. Baas P, Schrafford Koops H, Haekstra H, et al: Isolated regional perfusion in the treatment of melanoma of the extremities. Reg Cancer Treat 1:33â36, 1988.
60. Hafstrom L, Rudenstam C, Blomquist E, et al: Regional hyperthermic perfusion with melphalan after surgery for recurrent malignant melanoma. J Clin Oncol 9:2091â2094, 1991.
61. Kirkwood J, Hunt M, Smith T, et al: A randomized controlled trial of high-dose IFN alpha-2b for high-risk melanoma: The ECOG trial EST-1684 (abstract). Proc Am Soc Clin Oncol 12:390, 1993.
62. Cascinelli N, Bufalino R, Morabito A, et al: Results of adjuvant interferon study in WHO Melanoma Programme (letter). Lancet 343:913â914, 1994.
63. Coffey R, Flickinger J, Bissonette D, et al: Radiosurgery for solitary brain metastases using the cobalt-60 gamma unit: Methods and results in 24 patients. Int J Radiat Oncol Biol Phys 20:1287â1295, 1991.
64. Carbone P, Costello W: Eastern Cooperative Oncology Group studies with DTIC (NSC-45388). Cancer Treat Rep 60:193â198, 1976.
65. Costanza M, Nathanson L, Schoenfeld D, et al: Results with methyl-CCNU and DTIC in metastatic melanoma. Cancer 40:1010â1015, 1977.
66. Nathanson L, Walter J, Horton J, et al: Characteristics of prognosis and response to an imidazole carboxamide in malignant melanoma. Clin Pharmacol Ther 12:955â962, 1971.
67. Ramirez G, Wilson W, Grage T, et al: Phase II evaluation of 1,3-bis(2-chloroethyl)-1-nitrosourea (BCNU, NSC-409962) in patients with solid tumors. Cancer Treat Rep 56:787â790, 1972.
68. Jacquillat C, Khayat D, Banzet P, et al: Final report of the French multicenter phase II study of the nitrosourea fotemustine in 153 evaluable patients with disseminated malignant melanoma including patients with cerebral metastases. Cancer 66:1873â1878, 1990.
69. Retsas S, Peat I, Ashford R, et al: Updated results of vindesine as a single agent in the therapy of advanced malignant melanoma. Cancer Treat Rev 7(suppl):87â90, 1980.
70. Quagliana J, Stephens R, Baker L, et al: Vindesine in patients with metastatic malignant melanoma: A Southwest Oncology Group study. J Clin Oncol 2:316â319, 1984.
71. Mechl Z, Krejci P: Cis-diaminedichloroplatinum in the treatment of disseminated malignant melanoma. Neoplasma 30:371â377, 1983.
72. Chang A, Hunt M, Parkinson D, et al: Phase II trial of carboplatin in patients with metastatic malignant melanoma: A report from the Eastern Cooperative Oncology Group. Am J Clin Oncol 16:152â155, 1993.
73. Evans L, Casper E, Rosenbluth R: Phase II study of carboplatin in advanced malignant melanoma. Cancer Treat Rep 71:171â172, 1987.
74. Glover D, Glick J, Weiler C, et al: WR-2721 and high-dose cisplatin: An active combination in the treatment of metastatic melanoma. J Clin Oncol 5:574â578, 1987.
75. Legha S, Ring S, Papadopoulos N, et al: A phase II trial of Taxol in metastatic melanoma. Cancer 65:2478â2481, 1990.
76. Einzig A, Hochster H, Wiernik P, et al: A phase II study of Taxol in patients with malignant melanoma. Invest New Drugs 9:59â64, 1991.
77. Feun L, Gonzalez R, Savaraj N, et al: Phase II trial of piritrexim in metastatic melanoma using intermittent, low-dose administration. J Clin Oncol 9:464â467, 1991.
78. Legha S: Current therapy for malignant melanoma. Semin Oncol 16:34â44, 1989.
79. Costanzi J, Fletcher W, Balcerzak S, et al: Combination chemotherapy plus levamisole in the treatment of disseminated malignant melanoma. Cancer 53:833â836, 1984.
80. Vorobiof D, Sarli R, Falkson G: Combination chemotherapy with dacarbazine and vindesine in the treatment of metastatic malignant melanoma. Cancer Treat Rep 70:927â928, 1986.
81. Fletcher W, Green S, Fletcher J, et al: Evaluation of cisplatin and DTIC combination chemotherapy in disseminated melanoma: A Southwest Oncology Group study. Am J Clin Oncol 11:589â593, 1988.
82. Avril M, Bonneterre J, Delaunay M, et al: Combination chemotherapy of dacarbazine and fotemustine in disseminated malignant melanoma: Experience of the French Study Group. Cancer Chemother Pharmacol 27:81â84, 1990.
83. Costanzi J, Vaitkevicius V, Quagliana J, et al: Combination chemotherapy for disseminated melanoma. Cancer 35:342â346, 1975.
84. Seigler H, Lucas V, Pickett N, et al: DTIC, CCNU, bleomycin and vincristine (BOLD) in metastatic melanoma. Cancer 46:2346â2348, 1980.
85. York R, Foltz A: Bleomycin, vincristine, lomustine, and DTIC chemotherapy for metastatic melanoma. Cancer 61:2183â2186, 1988.
86. Franco E, for the Prudente Foundation Melanoma Study Group: Chemotherapy of disseminated melanoma with bleomycin, vincristine, CCNU, and DTIC (BOLD regimen). Cancer 63:1676â1680, 1989.
87. Stables G, Doherty V, MacKie R: Nine years' experience of BELD combination chemotherapy (bleomycin, vindesine, CCNU, and DTIC) for metastatic melanoma. Br J Dermatol 127:505â508, 1992.
88. Nathanson L, Kaufman S, Carey R, et al: Vinblastine infusion, bleomycin, and cis-dichlorodiammineplatinum chemotherapy in metastatic melanoma. Cancer 48:1290â1294, 1981.
89. Johnson D, Presant C, Einhorn L, et al: Cisplatin, vinblastine, and bleomycin in the treatment of metastatic melanoma: A phase II study of the Southeastern Cancer Study Group. Cancer Treat Rep 69:821â824, 1985.
90. Ringborg U, Jungnelius U, Hansson J, et al: DTIC-vindesine-cisplatin in disseminated malignant melanoma: A phase II study (abstract). Proc Am Soc Clin Oncol 6:212, 1987.
91. Legha S, Ring S, Papadopoulos N, et al: A prospective evaluation of a triple-drug regimen containing cisplatin, vinblastine, and dacarbazine (CVD) for metastatic melanoma. Cancer 64:2024â2029, 1989.
92. Pectasides D, Yianniotis H, Alevizakos N, et al: Treatment of metastatic malignant melanoma with dacarbazine, vindesine, and cisplatin. Br J Cancer 60:627â629, 1989.
93. Verschraegen C, Kleeberg U, Mudler J, et al: Combination of cisplatin, vindesine, and dacarbazine in advanced malignant melanoma: A phase II study of the EORTC Malignant Melanoma Cooperative Group. Cancer 62:1061â1065, 1988.
94. Nesbit R, Woods R, Tattersall M, et al: Tamoxifen in malignant melanoma. N Engl J Med 301:1241â1242, 1979.
95. Cocconi G, Bella M, Calabresi F, et al: Treatment of metastatic melanoma with dacarbazine plus tamoxifen. N Engl J Med 327:516â523, 1992.
96. Del Prete S, Maurer L, O'Donnell J, et al: Combination chemotherapy with cisplatin, carmustine, dacarbazine, and tamoxifen in metastatic melanoma. Cancer Treat Rep 66:1403â1405, 1984.
97. McClay E, Mastrangelo M, Berd D, et al: Effective combination chemo/hormonal therapy for malignant melanoma: Experience with three consecutive trials. Int J Cancer 50:553â556, 1992.
98. Richards J, Gilewski T, Ramming K, et al: Effective chemotherapy for melanoma after treatment with interleukin-2. Cancer 69:427â429, 1992.
99. Buzaid A, Murren J, Durivage H: High-dose cisplatin with dacarbazine and tamoxifen in the treatment of metastatic melanoma. Cancer 68:1238â1241, 1991.
100. Fierro M, Bertero M, Novelli M, et al: Therapy for metastatic melanoma: Effective combination of dacarbazine, carmustine, cisplatin and tamoxifen. Melanoma Res 3:127â131, 1993.
101. Nathanson L, Meelu M, Losada R: Chemohormone therapy of metastatic melanoma with megestrol acetate plus dacarbazine, carmustine, and cisplatin. Cancer 73:98â102, 1994.
102. Gonzales R, Sanchez A, Ferguson J, et al: Melatonin therapy of advanced human malignant melanoma. Melanoma Res 1:237â243, 1991.
103. Wolff S, Herzig R, Fay J, et al: High-dose thiotepa with autologous bone marrow transplantation for metastatic malignant melanoma: Results of phase I and II studies of the North American Bone Marrow Transplantation Group. J Clin Oncol 7:245â249, 1989.
104. Shea T, Antman K, Eder J, et al: Malignant melanoma: Treatment with high-dose combination alkylating agent chemotherapy and autologous bone marrow support. Arch Dermatol 124:878â884, 1988.
105. Thatcher N, Lind M, Morgenstern G, et al: High-dose, double alkylating agent chemotherapy with DTIC, melphalan, or ifosfamide and marrow rescue for metastatic malignant melanoma. Cancer 63:1296â1302, 1989.
106. Meisenberg B, Ross M, Vredenburgh J, et al: Randomized trial of high-dose chemotherapy with autologous bone marrow support as adjuvant therapy for high-risk, multi-node-positive malignant melanoma. J Natl Cancer Inst 85:1080â1085, 1993.
107. Karavodin L, Golub S: Systemic administration of human leukocyte interferon to melanoma patients: III. Increased helper:suppressor ratios in melanoma patients during interferon treatment. Nat Immun Cell Growth Reg 3:193â202, 1984.
108. Robinson W, Kirkwood J, Harvey H, et al: Effective use of recombinant human alfa 2 interferon (IFN alfa2) in metastatic malignant melanoma (MMM): A comparison of two regimens (abstract). Proc Am Soc Clin Oncol 3:60, 1984.
109. Kirkwood J, Ernstoff M, Davis C, et al: Comparison of intramuscular and intravenous recombinant alpha-2a interferon in melanoma and other cancers. Ann Intern Med 103:32â36, 1985.
110. Legha S, Papadopoulos N, Plager C: Clinical evaluation of recombinant interferon alfa-2A (Roferon-A) in metastatic melanoma using two different schedules. J Clin Oncol 5:1240â1246, 1987.
111. Creagan E, Ahmann D, Frytak S: Phase II trials of recombinant leukocyte alpha interferon in disseminated malignant melanoma: Results in 96 patients. Cancer Treat Rep 70:619â624, 1986.
112. Rosenberg S, Lotze M, Mule J: New approaches to the immunotherapy of cancer using interleukin-2. Ann Intern Med 108:853â864, 1988.
113. Parkinson D, Abrams J, Wiernik P, et al: Interleukin-2 therapy in patients with metastatic malignant melanoma: A phase II study. J Clin Oncol 8:1650â1656, 1990.
114. McCabe M, Stablein D, Hawkins M, et al: The modified group C experience-phase III randomized trials of IL-2 vs IL-2/LAK in advanced renal cell carcinoma and advanced melanoma (abstract). Proc Am Soc Clin Oncol 10:213, 1991.
115. Dutcher J, Creekmore S, Weiss G, et al: Phase II study of high dose interleukin-2 (IL-2) and lymphokine-activated killer (LAK) cells in patients with melanoma (abstract). Proc Am Soc Clin Oncol 6:246, 1987.
116. Sznol M, Clark J, Smith J, et al: Pilot study of interleukin-2 and lymphokine-activated killer cells combined with immunomodulatory doses of chemotherapy and sequenced with interferon alfa-2a in patients with metastatic melanoma and renal cell carcinoma. J Natl Cancer Inst 84:929â937, 1992.
117. Keilholz U, Scheibenbogen C, Tilgen W, et al: Interferon-alpha and interleukin-2 in the treatment of malignant melanoma: Comparison of two phase 2 trials. Cancer 72:607â614, 1993.
118. deBraud F, Biganzoli L, Bajetta E, et al: Subcutaneous low-dose interleukin-2 plus alpha interferon in advanced melanoma. Tumori 79:187â190, 1993.
119. Sparano J, Fisher R, Sunderland M, et al: Randomized phase III trial of treatment with high-dose interleukin-2 alone or in combination with interferon alfa-2a in patients with advanced melanoma. J Clin Oncol 11:1969â1977, 1993.
120. Bajetta E, Negretti E, Giannotti B, et al: Phase II study of interferon alpha-2a and dacarbazine in advanced melanoma. Am J Clin Oncol 13:405â409, 1990.
121. Kirkwood J, Ernstoff M, Giuliano A, et al: Interferon alpha 2a and dacarbazine in melanoma. J Natl Cancer Inst 82:1062â1063, 1990.
122. Thomson D, Adena M, McLeod G, et al: Interferon-alfa-2a does not improve response or survival when combined with dacarbazine in metastatic malignant melanoma: Results of a multi-institutional Australian randomized trial. Melanoma Res 3:133â138, 1993.
123. Falkson C, Falkson G, Falkson H: Improved results with the addition of interferon alfa-2a to dacarbazine in the treatment of patients with metastatic malignant melanoma. J Clin Oncol 9:1403â1408, 1991.
124. Bajetta E, Di Leo A, Zampino M, et al: Multicenter randomized trial of dacarbazine alone or in combination with two different doses and schedules of interferon alfa-2a in the treatment of advanced melanoma. J Clin Oncol 12:806â811, 1994.
125. Stoter G, Aamdal S, Rodenhuis S, et al: Sequential administration of recombinant human interleukin-2 and dacarbazine in metastatic melanoma: A multicenter phase II study. J Clin Oncol 9:1687â1691, 1991.
126. Flaherty L, Redman B, Chabot G, et al: A phase I-II study of dacarbazine in combination with outpatient interleukin-2 in metastatic malignant melanoma. Cancer 65:2471â2477, 1990.
127. Flaherty L, Liu P, Fletcher W, et al: Dacarbazine and outpatient interleukin-2 in treatment of metastatic malignant melanoma: A phase II Southwest Oncology Group trial. J Natl Cancer Inst 84:893â894, 1992.
128. Fiedler W, Jasmin C, De Mulder P, et al: A phase II study of sequential recombinant interleukin-2 followed by dacarbazine in metastatic melanoma. Eur J Cancer 28:443â446, 1992.
129. Dillman R, Oldham R, Barth N, et al: Recombinant interleukin-2 and adoptive immunotherapy alternated with dacarbazine therapy in melanoma: A National Biotherapy Study Group trial. J Natl Cancer Inst 82:1345â1349, 1990.
130. Khayat D, Borel C, Torani J, et al: Sequential chemoimmunotherapy with cisplatin, interleukin-2, and interferon alfa-2a for metastatic melanoma. J Clin Oncol 11:2173â2180, 1993.
131. Verschraegen C, Legha S, Hersh E, et al: Phase II study of vindesine and dacarbazine with or without non-specific stimulation of the immune system in patients with metastatic melanoma. Eur J Cancer 29A:708â711, 1993.
132. Thatcher N, Wagstaff J, Mene A, et al: Corynebacterium parvum followed by chemotherapy (actinomycin D and DTIC) compared with chemotherapy alone for metastatic malignant melanoma. Eur J Cancer 22:1009â1014, 1986.
133. Legha S, Plager S, Ring S, et al: A phase-II study of biochemotherapy using interleukin-2 (IL-2) + interferon alfa-2a (IFN) in combination with cisplatin (C), vinblastine (V), and DTIC (D) in patients with metastatic melanoma (abstract). Proc Am Soc Clin Oncol 11:343, 1992.
134. Legha SS, Ring S, Bedikian AY, et al: Combined biochemotherapy in the treatment of advanced melanoma, in Program and Abstracts: Advances in the Biology and Clinical Management of Melanoma, pp 32â33 (abstract). Houston, The University of Texas M. D. Anderson Cancer Center, 1995.
135. Richards J, Mehta N, Ramming K, et al: Sequential chemoimmunotherapy in the treatment of metastatic melanoma. J Clin Oncol 10:1338â1343, 1992.
136. Atkins M, O'Boyle K, Sosman J, et al: Multi-institutional phase II trial of intensive combination chemoimmunotherapy for metastatic melanoma. J Clin Oncol 12:1553â1560, 1994.
137. Flaherty L, Robinson W, Redman B, et al: A phase II study of dacarbazine and cisplatin in combination with outpatient administered interleukin-2 in metastatic melanoma. Cancer 71:3520â3525, 1993.
138. Morton D, Foshag L, Hoon D, et al: Prolongation of survival in metastatic melanoma after active specific immunotherapy with a new polyvalent melanoma vaccine. Ann Surg 216:463â482, 1992.
139. Berd D, Maguire H Jr, McCue P, et al: Treatment of metastatic melanoma with an autologous tumor-cell vaccine: Clinical and immunologic results in 64 patients. J Clin Oncol 8:1858â1867, 1990.
140. Mitchell M, Harel W, Kempf R, et al: Active-specific immunotherapy for melanoma. J Clin Oncol 8:856â869, 1990.
141. Mittelman A, Chen Z, Kageshita T, et al: Active specific immunotherapy in patients with melanoma: A clinical trial with mouse anti-idiotypic monoclonal antibodies elicited with syngeneic anti-high molecular weight melanoma-associated antigen monoclonal antibodies. J Clin Invest 86:2136â2144, 1990.
142. Steffens T, Bajorin D, Houghton A: Immunotherapy with monoclonal antibodies in metastatic melanoma. World J Surg 16:261â269, 1992.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.