Novel PSMA-TRT-based Triplet Regimen Appears Effective in Prostate Cancer
All patients with chemo-naïve metastatic castration-resistant prostate cancer experienced PSA decline, and half the cohort experienced a PSA decline greater than 50% after treatment with a novel PSMA-targeted radionuclide therapy.
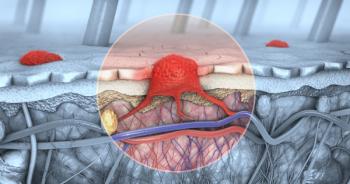
The use of an alpha prostate-specific membrane antigen-targeted radionuclide therapy (PSMA-TRT, 225Ac-J591), an androgen receptor (AR) signaling inhibitor, and pembrolizumab (Keytruda) elicited preliminary responses in patients with chemo-naïve metastatic castration-resistant prostate cancer (mCRPC), investigators reported.1
The preliminary findings of a phase 1/2 study were presented at the
“Immunotherapy generally results in modest responses for prostate cancer. Radiation, though, may increase the proportion of patients that respond to immunotherapy,” Sun explained.
In addition, PSMA-TRT is able to radiate multiple sites of disease simultaneously, and AR signaling inhibitors upregulate PSMA expression, may lead to increased PD-L1 expression, and can also radiosensitize prostate cancer.
“We hypothesize that triple therapy with [PSMA-TRT], pembrolizumab, and an [AR signaling inhibitor] will have a synergistic effect and lead to better responses and outcomes relative to immunotherapy plus [AR signaling inhibitor] alone,” Sun said.
The study enrolled patients with progressive mCRPC as defined by Prostate Cancer Working Group 3 criteria (at least 1 AR pathway inhibitor and no chemotherapy in the mCRPC setting). During the phase 1 portion of the study, patient received physician’s choice of AR signaling inhibitor along with pembrolizumab (400 mg every 6 weeks) along with a single infusion of 225Ac-J591 in 2 different cohorts of 6 patients (65 KBq/kg or 80 KBq/kg).
The phase 1 portion’s primary end point was the determination of 225Ac-J591 dose for the phase 2 portion of the study.
Median patient age was 66.5 years, and median prostate-specific antigen level was 7.75 ng/mL. Six patients (50%) had Cancer and Leukemia Group B intermediate-risk disease, 4 (33%) had low-risk disease, and 11 patients (92%) had bone metastases. All patients had received at least 1 prior AR pathway inhibitor. Five patients (42%) had received prior sipuleucel-T (Provenge), 1 (8%) had received prior radium-223 (Xofigo), 6 (50%) had received prior enzalutamide (Xtandi), 7 had received prior abiraterone acetate (Zytiga), and 2 (17%) had received prior PSMA-TRT.
AR signaling inhibitors used in the study included enzalutamide in 7 patients (58%), apalutamide (Erleada) in 3 patients (25%) and darolutamide (Nubeqa) in 2 patients (17%).
All of the patients experienced PSA decline, and half the cohort experienced a PSA decline greater than 50%. At more than 6 months’ follow-up, 4 patients (all from the 80 KBq/kg cohort) are still progression free and on study.
Regarding adverse events (AEs), “7 patients (58%) developed an unexpected inflammatory syndrome 7-14 days following treatment (C1D1) characterized by morbilliform rash, fever higher than 101°F, and low blood counts,” wrote the authors in their poster.
All-grade AEs included thrombocytopenia in 9 patients (75%), neutropenia in 7 patients (58%), nausea in 6 patients (50%), fatigue in 8 patients (67%), xerostomia in 9 patients (75%), and AST increase in 8 patients (67%).
Based on the findings of the phase 1 portion, the investigators selected the 80 KBq/kg dose of 225Ac-J591 for the phase 2 portion of the study, Sun reported at the meeting. That phase of the study is currently under way.
“Phase 2 is multicenter. Patients are randomized to triplet vs doublet [therapy],” Sun said. “The stratification criteria is based on presence or absence of visceral metastases, PSMA-PET imaging intensity, and [circulating blood cell (CBC)] count at baseline.
“The primary end point is response…which is a composite of radiographic response by RECIST criteria, conversion of unfavorable CBC counts to favorable, or PSA 50.”
Reference
1. Sun M, Nauseef J, Huicochea Castellanos S, et al. Phase I results of a phase I/II trial of pembrolizumab and AR signaling inhibitor (ARSI) +/- 225Ac-J591 for chemo-naïve metastatic castration-resistant prostate cancer (mCRPC). Presented at: Society for Urologic Oncology (SUO) 23rd Annual Meeting; November 30-December 2, 2022; San Diego, California. Poster 76. https://suo-abstracts.secure-platform.com/a/gallery/rounds/15/details/2687
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.