Skin Cancer Rates Higher in Gay, Bisexual Men
Possibly due to a higher prevalence of indoor tanning, skin cancer rates are higher among gay and bisexual men compared to their heterosexual.
Skin cancer rates are higher among gay and bisexual men compared to their heterosexual counterparts, according to the results of a recent study. By contrast, gay and bisexual women were less likely to have nonmelanoma skin cancer than heterosexual women. These differences may be attributable to indoor tanning habits.
The article, “Association of Skin Cancer and Indoor Tanning in Sexual Minority Men and Women,” was
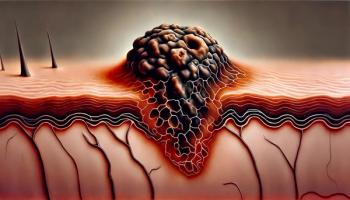
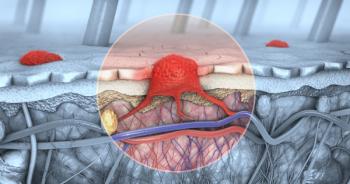
“Incidence of nonmelanoma skin cancer and melanoma in the United States has increased rapidly at 4.2% and 1.9% annually, respectively,” wrote authors led by Matthew Mansh, MD, of the department of dermatology at the University of California, San Francisco. “Conceptual and empirical data suggest that sexual minority men might be more likely to engage in indoor tanning and to develop skin cancer.”
The researchers analyzed data from several California Health Interview Surveys (CHISs) and the 2013 National Health Interview Survey (NHIS) to understand the prevalence of skin cancer and indoor tanning among gay and bisexual men and women. The study included 3,083 gay and bisexual men matched with 78,487 heterosexual men, and 3,029 gay and bisexual women matched with 107,976 heterosexual women.
Between 2001 and 2005, the CHIS data showed that skin cancer prevalence was 4.3% among gay and bisexual men compared with 2.7% among their heterosexual counterparts. The NHIS data also showed higher rates of skin cancer among gay and bisexual men compared with heterosexual men (6.7% vs 3.2%).
Gay and bisexual men were more likely to report the use of indoor tanning beds compared with heterosexual men (P < .001 for both the CHIS and NHIS data).
Gay and bisexual women were less likely than heterosexual women to report a nonmelanoma skin cancer diagnosis (P < .008) or indoor tanning (P = .03 for the CHIS data; P = .007 for the NHIS data).
“Studies exploring predictors of indoor tanning and other skin cancer risk behaviors in sexual minority men and how these fit into the sexual minority stress model would further our understanding of why sexual minority men are disproportionately affected by preventable diseases,” wrote Aaron J. Blashill, PhD, of San Diego State University, and Sherry Pagoto, PhD, of the University of Massachusetts Medical School, in an
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.