
- ONCOLOGY Vol 9 No 11
- Volume 9
- Issue 11
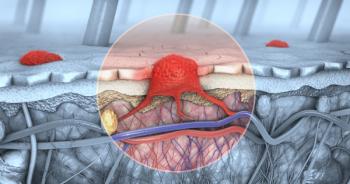
Systemic Treatments for Advanced Cutaneous Melanoma
The treatment of advanced cutaneous melanoma remains disappointing. Single-agent cytotoxic drugs usually produce response rates of less than 20%, though newer agents, particularly fotemustine and temozolomide, show some promise, especially in patients with brain metastases.
The treatment of advanced cutaneous melanoma remains disappointing. Single-agent cytotoxic drugs usually produce response rates of less than 20%, though newer agents, particularly fotemustine and temozolomide, show some promise, especially in patients with brain metastases. Combination chemotherapy regimens yield response rates of 20% to 40%, but durable complete remissions are uncommon. Interferon-alfa and interleukin-2 alone produce response rates of 10% to 20%, 3% to 5% of which are durable. Vaccines and monoclonal antibodies have low level activity in advanced disease but may play a role in the adjuvant setting. The combinations of cisplatin-based regimens plus IFN-alfa and IL-2 have produced overall response rates of 50% to 60% and complete responses in 20% of patients, about half of which are durable. The toxicity of these regimens is severe, however, and their impact on survival remains to be established.
Cutaneous malignant melanoma is becoming a more common neoplasm. In 1995, an estimated 34,000 cases of melanoma will be diagnosed in the United States and 7,200 deaths due to melanoma will occur [1]. By the year 2000, it is estimated that 1 of every 75 Americans will be diagnosed with melanoma.
Early primary melanoma is highly curable, but once the disease becomes widely disseminated, it is nearly always fatal. The survival time for patients with metastatic disease ranges from 6 to 9 months when metastases are detected in multiple organ sites. Patients with skin, subcutaneous tissue, and distant lymph node metastases have the longest survival, averaging 12 to 15 months, whereas patients with liver, brain, and bone metastases have a median survival of only 3 to 4 months [2].
The treatment of metastatic melanoma remains unsatisfactory, and thus far survival has been determined primarily by the extent and pace of the disease, rather than by the treatment strategy. In this article, we provide an overview of the systemic treatment options for advanced cutaneous melanoma, with emphasis on the more novel therapeutic approaches.
Single-Agent Chemotherapy
The only single agent approved for the treatment of melanoma is dacarbazine, which produces response rates of 10% to 20% but results in complete remission in less than 5% of treated patients [2]. Responses have been observed mainly in soft tissues, ie, skin, subcutaneous tissue, lymph node, and lung metastases, and are usually short-lived, ranging from 3 to 6 months. Although complete responses are rare, approximately one-fourth of complete responders do attain long-term remissions [2].
The antitumor activity of the nitrosoureas currently available in the United States-carmustine (BCNU [BiCNU]), and lomustine (CCNU [CeeNu])-is similar to that of dacarbazine, with response rates ranging from 10% to 20% [2]. Patients previously exposed to dacarbazine have an even lower response rate to the nitrosoureas than do untreated patients.
Fotemustine, a new agent of this class, has recently been studied in Europe. This novel chloroethyl nitrosourea with an amino acid-phosphonyl adduct has a mechanism of action involving rapid metabolic conversion and consequent alkylation of thioenzymes involved in DNA synthesis. In addition, it rapidly crosses the blood-brain barrier, possibly through an amino acid transport system. A multicenter phase II study of fotemustine with 153 assessable patients showed a response rate of 30% in previously untreated patients and 24% overall [3]. Most importantly, a response rate of 20% was observed in 85 patients with brain metastases, and some of the responses were durable [4].
Other classes of chemotherapeutic agents with antitumor activity include the vinca alkaloids and platinum compounds, including cisplatin (Platinol) and carboplatin (Paraplatin), which have reported response rates of 10% to 20% [2]. A new lipid-soluble dihydrofolate reductase inhibitor, piritrexim (taken orally), produced a response rate of 23% in 31 evaluable patients [5]. Interestingly, responses were seen in previously treated as well as previously untreated patients.
Taxanes, including paclitaxel (Taxol) and docetaxel (Taxotere), agents that inhibit disassembly of the microtubule complex, have also been evaluated in metastatic melanoma. In two phase II trials, 3 complete responses and 4 partial responses were observed among 53 melanoma patients [5]. Docetaxel has produced similar response rates, with 3 responders in 27 patients studied [6,7]. Further exploration of the taxanes in combination with other cytotoxic agents is warranted.
Another new agent, temozolomide, which is entering phase II studies in the United States, deserves special mention. This agent is an imidazotetrazine derivative that spontaneously converts in vivo to MTIC (methyl triazeno imidazole carboxamide), the active metabolite of dacarbazine, and crosses the blood-brain barrier efficiently in animal models. Temozolomide has shown significant antitumor activity in preclinical studies, and responses have been seen in phase I trials in patients with melanoma (with and without brain metastases) and in patients with primary brain tumors [5].
A recent European phase II study in 49 assessable patients with metastatic disease demonstrated a 6% complete response rate and a 21% total response rate [8]. In this series, four patients had brain metastases, one of whom attained a partial response. The possible utility of this agent awaits further phase II data.
Combination Chemotherapy
Based on the independent activity of dacarbazine and the nitrosoureas, several studies combining the two agents were performed in the late 1970s. These studies failed to show the superiority of the combination regimens over dacarbazine alone [2]. Dacarbazine also has been combined with dactinomycin (Cosmegan), vinca alkaloids, cisplatin, and fotemustine. The observed response rates with the two-drug combinations have ranged from 20% to 35%, which are not clearly superior to response rates achieved with dacarbazine alone [2].
Combinations of three or more drugs with or without dacarbazine also have been investigated. A three-drug combination regimen of BCNU, hydroxyurea (Hydrea), and dacarbazine tested by the Southwest Oncology Group (SWOG) produced an overall response rate of 27% in 178 patients, with response duration averaging 6 months [2].
A regimen combining bleomycin, Oncovin, lomustine, and dacarbazine (BOLD), developed in the late 1970s at Duke University, produced a 40% response rate (9% complete responses) in a total of 72 assessable patients [2]. Subsequent studies with the BOLD regimen failed to confirm these initial results, however; overall response rates in these later studies ranged from 4% to 20% [5].
Among combination chemotherapy regimens not including dacarbazine that were developed in the late 1970s and early '80s, a combination of bleomycin (Blenoxane), vinblastine, and cisplatin showed response rates ranging from 22% to 43% in several trials [2]. More recently, various groups have reported their results combining dacarbazine, cisplatin, and a vinca alkaloid (either vinblastine or vindesine [Eldisine]) [2]. The response rates achieved with this three-drug combination ranged from 24% to 45%, which appear to be superior to rates reported with dacarbazine alone.
Phase III Trials--Despite the abundance of phase II studies exploring different combinations of cytotoxic drugs, there have been only a limited number of phase III trials comparing dacarbazine alone with combination chemotherapy or comparing different combination regimens. The results of these phase III trials are summarized in Table 1 [9-16]. Except for the SWOG study reported by Costanzi et al [12], which showed a significant improvement in response rate for combination chemotherapy vs dacarbazine, all the trials were extremely small and therefore had insufficient power to detect significant differences in response rate or survival. In addition, some of the studies combined dacarbazine with relatively inactive drugs. Thus, it is not surprising that none of the studies showed a significant difference in survival and only one study revealed a significant improvement in response rate.
The final results of the Cancer Community Oncology Program study, which compares dacarbazine alone with cis-platin, vinblastine, and dacarbazine (CVD) should be available in the near future [16]. Also, investigators at Memorial Sloan-Kettering Cancer Center are currently evaluating the combination of cisplatin, BCNU, dacarbazine, and tamoxifen vs dacarbazine alone. Pending the results of these and other controlled studies, dacarbazine alone remains the standard for initial chemotherapy treatment of metastatic melanoma.
Chemohormonal Therapy
Hormonal therapy in melanoma has been studied since the early 1970s.
Tamoxifen--Of the hormonal agents evaluated in melanoma, tamoxifen has been studied most extensively. In large phase II trials, this nonsteroidal antiestrogen produced overall response rates of only 4% to 6% [17]. Responses were seen primarily among women and in patients with soft-tissue metastases.
Based on the simple principle of combining active agents against melanoma to attain at least an additive antitumor effect, investigators from the Dartmouth School of Medicine evaluated the combination of cisplatin, BCNU, dacarbazine, and tamoxifen. In 1984, Del Prete et al [18] reported on the activity of this regimen (often referred to as the "Dartmouth regimen" or CBDT) in 20 patients with metastatic disease; they obtained an overall response rate of 55% with a complete response rate of 20%. McClay et al [19] confirmed these initial results in 20 patients, but because of a high incidence of thromboembolic events, dropped tamoxifen from the regimen in the next cohort of 25 patients, with a decrease in response rate from 52% to 10% [17]. Similar results were observed by the Dartmouth group, again with a small number of patients [20].
Based on the results of these small pilot studies, McClay et al have suggested that tamoxifen was the component crucial to the effectiveness of this regimen. Various investigators subsequently pursued this lead, with conflicting results (Table 2) [21-29]. In studies using all four drugs, response rates have been consistently high (approximately 40%), although these studies have been carried out at single institutions with relatively small numbers of patients.
Preliminary in vitro data reported by McClay et al [17] suggest that tamoxifen and cisplatin exhibit synergistic antitumor activity in melanoma, possibly through the binding of tamoxifen to antiestrogen binding sites on tumor cells. In addition, a pilot study conducted by McClay et al [17], in which the addition of tamoxifen to cisplatin after cisplatin failure produced some clinical responses, supports this hypothesis. However, two phase II studies reported by Buzaid et al [26] and Flaherty et al [27] using cisplatin, dacarbazine, and tamoxifen but no BCNU showed response rates of less than 20%.
More recently, various groups have used high doses of tamoxifen with the Dartmouth regimen or some of its components with the intent of enhancing the efficacy of the combination [21,25,30,31]. However, the response rates in these studies do not appear to be clearly better than those using lower doses of tamoxifen [20,22-24,29].
To date, the results of four randomized studies comparing chemotherapy regimens with and without tamoxifen have been reported; these are summarized in Table 3 [32-34]. Of the four studies, only the study by Cocconi et al [34], which compared dacarbazine alone with dacarbazine plus tamoxifen, showed an improvement in response rate and survival. In this report, the major benefit was observed in women. All the other studies failed to show any differences in the response rate.
Most importantly, the largest study, conducted under the auspices of the National Cancer Institute of Canada, compared cisplatin, dacarbazine, BCNU, and tamoxifen with the same chemotherapy drugs plus placebo and also showed no statistically significant difference in response rate or survival (J.J. Rusthoven, MD; personal communication, May 1995). This well-designed, prospective, randomized study found that tamoxifen does not appear to significantly enhance the antitumor effect of the combination of cisplatin, dacarbazine, and BCNU and illustrates the problem of drawing conclusions based on small sequential trials.
Other Hormones--Megestrol acetate also has been added to the same cytotoxic agents as the Dartmouth regimen in one trial, with a total response rate of 47% in 19 patients [35]. One other hormonal maneuver has been studied in melanoma--daily oral melatonin, the melanocyte-suppressive hormone of pineal origin that has been shown to have growth-suppressive, immunostimulatory, and oncostatic properties in animal models. This hormone showed a 15% response rate in 40 patients with metastatic disease, with no toxic effects except fatigue [36]. Melatonin deserves further investigation, especially as a modulator of chemotherapy response.
High-Dose Chemotherapy With Autologous Bone Marrow Support
High-dose chemotherapy with either single or multiple agents followed by autologous bone marrow transplantation has produced high rates of response, ranging from 20% to 81%. Complete response rates have been quite low, however, and the responses have been short-lived, with very few long-term survivors [5]. In the future, possible use of high-dose chemotherapy in complete responders may be reconsidered as consolidation therapy after aggressive combination therapy.
Nonspecific immunotherapy, including bacillus Calmette-Guérin (BCG) injections and Corynebacterium parvum extract treatments, has been used for decades in the treatment of malignant melanoma, although it has had only minimal impact on the natural history of the disease. Recently, the advent of recombinant DNA techniques has rekindled interest in biologic therapy for the treatment of melanoma.
Interferons
Initial studies showed that partially purified human leukocyte-derived interferon (IFN) stimulated T-helper/inducer subsets of lymphocytes and increased natural killer cell activity, but showed only minimal activity against melanoma. Subsequently, several groups studied recombinant IFNs alfa-2a (Roferon) and alfa-2b (Intron A) at different dosages and schedules for the treatment of advanced melanoma, and observed response rates of 8% to 22% [2,5]. The greatest antitumor effects of IFN-alfa were obtained with chronic administration on a daily or three-times-weekly basis, whereas very few patients responded to once-weekly doses or 5-day courses every 3 weeks [2].
Interferon has been used with equal efficacy in patients who have not responded to chemotherapy, in whom alternative chemotherapy is rarely effective. In a small proportion of melanoma patients, IFN has controlled the disease for periods in excess of 2 to 3 years [2,5]. The frequency of response to IFN-alfa is somewhat higher for soft-tissue metastases than for disease at other distant sites; however, therapeutic responses have been observed in lung and liver metastases as well. Phase I/II studies with IFN-beta and -gamma are more limited and suggest a lower response rate compared to that seen with IFN-alfa [5].
Interleukin-2
The second biologic agent to show activity against metastatic melanoma was interleukin-2 (IL-2), a cytokine also known as T-cell-derived growth factor, which mediates the activation and expansion of effector lymphocytes after antigen exposure. In the initial studies performed at the NCI, 6 partial responses were obtained among 23 patients treated with high-dose IL-2 alone [5]. These results were subsequently confirmed by various groups, who reported response rates in the range of 10% to 20% [5]. Similar responses have been observed when IL-2 was administered by continuous infusion but with less toxicity [5].
Based on murine models showing that the combination of IL-2 plus lymphokine-activated killer (LAK) cells (autologous lymphocytes activated by IL-2 ex vivo) was clearly superior to IL-2 alone, Rosenberg et al [5] evaluated the combination of IL-2 with LAK cells in patients with advanced melanoma. In their initial report, among 34 patients treated, 3 achieved a complete response and 3, a partial response. Despite the strong preclinical data and the encouraging preliminary results reported by Rosenberg et al, the results of phase III trials showed no significant difference between IL-2 alone and IL-2 plus LAK cells in terms of response rate and survival [5].
Another strategy, also pioneered by Rosenberg's group, was the combination of IL-2 with tumor-infiltrating lymphocytes (TILs), lymphocytes derived from tumor isolates cultured in the presence of IL-2, which, in animal models, were shown to be 50 to 100 times more potent in tumor cell-killing activity than LAK cells. The pooled results of studies of IL-2 and TILs conducted at the NCI up to 1993 in a total of 50 patients demonstrate a response rate of 38% [5], which is only a modest improvement over that for IL-2 alone, particularly in light of the tremendous expense and complexity of the treatment. Furthermore, other investigators have not been able to reproduce the results of Rosenberg et al; response rates observed by these groups have been in the 20% range [5].
The NCI investigators are currently combining IL-2 with TILs transfected with the tumor necrosis factor (TNF) gene, which was more effective than TILs alone in animal models. Lastly, Rosenberg's group is investigating the use of TILs that specifically recognize certain melanoma antigens, such as melanoma antigen gene (MAGE)-1, MAGE-2, and melanoma antigen recognized by T-cells (MART)-1.
Interferon-alfa Plus Interleukin-2
As IFN-alfa upregulates the expression of major histocompatibility complex class I antigens in tumor cells and activates mononuclear cell killing activity, it was hypothesized that interferon-alfa could enhance the antitumor activity of IL-2 in vivo [5]. This hypothesis was confirmed in murine models, which clearly showed a synergistic interaction between IFN-alfa and IL-2. Following this lead, various clinical studies were conducted in patients with advanced melanoma, with overall response rates ranging from 10% to 41% in large series [5].
Despite the encouraging phase II data, a randomized trial comparing IL-2 plus IFN-alfa to IL-2 alone in 85 patients showed no significant difference in response rate and survival [5]. It thus remains unclear as to whether IL-2 plus IFN-alfa is indeed superior to IL-2 alone.
Most IL-2 studies have used fixed doses of IL-2. More recently, Keilholz et al [5] reported the results of two phase II trials that evaluated different schedules of IFN followed by IL-2. In one study, IL-2 was given at a fixed dose (referred to as the "fixed-dose regimen"), while in the other, IL-2 was initially given in high doses followed by a rapid taper (the "decrescendo regimen"). According to the investigators, the rationale for the decrescendo regimen was that the high initial doses of IL-2 would increase the induction of the alfa chain of the IL-2 receptor on lymphocytes, and the subsequent rapid taper would decrease the production of TNF and reduce toxicity. In a phase II study, the decrescendo regimen was not only more active but also less toxic than the fixed-dose regimen, with response rates of 41% vs 18%, respectively (P = 0.067). This study suggests that the decrescendo regimen may be more active and less toxic than the traditionalfixed-dose regimens and, therefore, merits further evaluation.
Unlike metastatic renal cell carcinoma, clinical experience with subcutaneous IL-2 plus IFN-alfa in melanoma is limited and does not permit definitive conclusions to be made about its activity.
Other Cytokines
Other cytokines that have been studied in melanoma but have shown limited antitumor activity when used alone include TNF-alfa, IL-1, and macrophage colony-stimulating factor (M-CSF) [5]. These cytokines may prove useful when combined with other biologic or cytotoxic agents, however. In addition, TNF-alfa, which has been shown to be too toxic and inactive in the systemic treatment of advanced melanoma, has found an application in recent studies of isolated limb perfusion therapy for patients with locoregional cutaneous involvement [5].
Melanoma Vaccines and Monoclonal Antibodies
Vaccine therapy can be categorized into several types, including autologous melanoma cell preparations, allogeneic cell fraction preparations, purified melanoma antigens, and anti-idiotypic antibodies. Vaccine development in melanoma and other malignancies has progressed steadily in recent years, but objective responses have been seen in only approximately 5% to 20% of patients with advanced disease, and the impact on survival remains questionable [5]. If vaccines eventually play a useful role in the treatment of melanoma, it will likely be in the adjuvant setting in high-risk patients rather than in patients with measurable disseminated disease. The identification of cell surface antigens of melanoma, defined by serology (eg, gangliosides) or by autologous T-cells (MAGE-1, MAGE-2, and MART-1), will likely provide the most promising new approach for developing specific immunotherapy.
Anti-idiotypic antibodies (monoclonal antibodies directed against the variable region of antimelanoma antigen antibodies, thereby mimicking the antigen itself) have also been used as vaccines. These antibodies stimulate humoral immune response with little toxicity but have low response rates [5]. In addition to the antiidiotypic antibodies, other monoclonal antibodies have been used [5]. Most of these agents have been directed against glycolipid antigens that are preferentially expressed on melanocytes and melanoma cells.
Although responses to monoclonal antibodies have been observed in less than 20% of patients treated, toxicity usually has been low. The combinations of antibodies with cytokines such as IL-2, granulocyte-macrophage colony stimulating factor, and M-CSF are also being evaluated currently [5].
"Biochemotherapy" is a term used by Legha et al at M.D. Anderson Cancer Center to describe the combination of chemotherapy with biologic-response modifiers, particularly IL-2 and IFN-alfa, for the treatment of advanced melanoma [2]. Other investigators refer to the combination of these two treatment modalities as "chemoimmunotherapy." Although the strategy of combining nonspecific immunomodulatory agents (eg, BCG and C parvum) with chemotherapy was initially studied more than 10 years ago, the combination of cytokines, particularly IL-2 and IFN-alfa, with chemotherapy has been the focus of more intense investigation primarily over the last 5 years.
Chemotherapy Plus Interferon-Alfa
Interferon-alfa has been evaluated in combination with many single-agent chemotherapeutic drugs and with multiagent chemotherapy. Results of phase II studies of IFN-alfa with dacarbazine, cisplatin, vinca alkaloids, and nitrosoureas showed activity similar to that of single-agent chemotherapy alone, suggesting a lack of additional benefit of IFN-alfa [5,37-39]. Likewise, phase II studies combining IFN-alfa with the Dartmouth regimen [40-42] or with CVD [32] showed response rates comparable to those for chemotherapy alone.
In contrast to these studies, Pyrhonen et al [5] reported encouraging results with the combination of BOLD plus IFN-alfa in 45 patients, with an overall response rate of 62% and a complete remission rate of 13%. These provocative results with a relatively nontoxic regimen merit further evaluation.
Phase III Trials--To date, only four phase III randomized trials comparing chemotherapy alone vs chemotherapy combined with IFN-alfa have been reported, and all these studies used dacarbazine alone as the cytotoxic agent. The results, which have been conflicting, are summarized in Table 4 [31,43-45]. Kirkwood et al [43] observed no difference in response rate or survival for the combination of dacarbazine plus IFN-alfa compared to dacarbazine alone. Falkson et al [45] reported that the addition of IFN-alfa significantly improved the response rate, duration of response, and survival. Bajetta et al [44] found that both high- and low-dose IFN-alfa in combination with dacarbazine increased the duration of response but did not significantly affect response rate or survival. Thomson et al [31] failed to detect a beneficial effect of the addition of IFN-alfa on response rate, duration of response, or survival. The results are compromised, however, because use of escalating doses of dacarbazine in the IFN arm precluded optimal dacarbazine dosing during the first three cycles.
The Eastern Cooperative Oncology Group is currently conducting a large randomized trial that is comparing dacarbazine alone with dacarbazine plus IFN-alfa. The results of this important study will better define the role of IFN-alfa in combination with dacarbazine.
Chemotherapy Plus Interleukin-2
The addition of IL-2 to chemotherapy has been reported by a number of investigators. The most thoroughly evaluated combination, IL-2 plus dacarbazine, yielded response rates of 13% to 33% (mean, 25%), which are not clearly superior to those for dacarbazine alone, and the combination is definitely more toxic [46].
Interleukin-2 has also been studied in combination with cisplatin-based regimens and has produced better results than IL-2 plus dacarbazine (Table 5) [47-49]. These improved results, which may be due to a particular interaction between cisplatin and IL-2, need to be confirmed in a trial in which assessment of survival is the major end point.
Chemotherapy, IL-2, and IFN-alfa
Four groups have published results of studies using cytotoxic drugs in combination with IL-2 plus IFN-alfa in patients with metastatic melanoma (Table 6) [46,50-55]. The treatment schema of the most active biochemotherapy programs are shown in Figure 1. Richards et al [50] from the University of Chicago integrated biotherapy with the Dartmouth regimen. Chemotherapy was administered on days 1 through 3 followed by IFN-alfa and IL-2 on days 4 through 8 and days 17 through 21 (Figure 1). The overall response rate was 57% in 42 patients. In a more recent update, 15% of 74 patients achieved complete responses with the same overall response rate and a median survival of more than 15 months for the complete responders [53].
Rixe et al [51] recently reported the results of a French multicenter trial that included the Salpetriere Hospital experience; in this trial, the combination of cisplatin, IL-2, and IFN-alfa showed an overall objective response rate of 52% among 80 assessable patients. Of note, the addition of tamoxifen to the treatment regimen in the second cohort of patients in this trial did not increase the complete or overall response rates. In contrast, another multicenter trial, also from France, comparing the Salpetriere Hospital regimen vs cisplatin plus IFN-alfa alone reported response rates of only 26% and 17%, respectively [52]. The reason for these discrepant results is unclear, but may be related, in part, to the different levels of experience in using IL-2 between the two study groups.
M. D. Anderson Hospital Experience--To explore the effect of different schedules of biochemotherapy, Legha et al have conducted a series of sequential phase II trials that integrated IFN-alfa (given for 5 days) and IL-2 (4 days) (BIO) with cisplatin (4 days), vinblastine (4 or 5 days), and dacarbazine (1 day) (CVD) [46,54]. All patients had advanced melanoma, a performance status of 0 to 3, and no evidence of symptomatic or progressive brain metastases.
In the first study, BIO and CVD were alternated every 6 weeks (referred to as "alternating biochemotherapy"; Figure 1) in order to minimize toxicity and to avoid the theoretical possibility that chemotherapy could interfere with the immunologic effects of biotherapy. Patients were randomly assigned to receive either CVD followed by BIO, or BIO followed by CVD. The two regimens produced similar results and were analyzed together. The observed response rate of 33% was not superior to the previous experience with CVD alone used at our institution.
In view of the suboptimal results with the alternating biochemotherapy program, the protocol was modified so that the BIO and CVD components were given in sequence, one followed immediately by the other. This second study was thus called "sequential biochemotherapy." Because it was unclear whether the chemotherapy should precede the biotherapy or vice versa, patients were randomized so that half received CVD followed by BIO (CVD/BIO, see Figure 1), and 1 week later, a "sandwich" consisting of biotherapy followed by CVD followed by biotherapy (BIO/CVD/BIO). The other half received the opposite sequence, starting with the BIO/CVD/BIO sandwich, and 1 week later BIO followed immediately by CVD (BIO/CVD).
Compared with CVD alone, CVD/BIO produced a higher response rate (73% vs 40%, P = 0.008), progression-free survival (8 vs 4 months, P = 0.005), and overall survival (12 vs 9 months, P = 0.006). CVD/BIO was also superior to BIO/CVD on the basis of response rate (73% vs 47%, P = 0.065) and progression-free survival (8 vs 7 months, P = 0.007) but not overall survival (P = 0.18).
In the most recent study, the biotherapy and the chemotherapy were administered at the same time ("concurrent biochemotherapy") to reduce the treatment delivery time from 10 days to 5. Biochemotherapy was given for 5 days, repeated every 21 days. The doses were identical to those in the previous trials, except for vinblastine, which was given for 4 days instead of 5. In addition, IFN-alfa was repeated during the second week of therapy on days 7, 9, 11, and 13. The overall response rate was 63%, which was superior to that of CVD alone (P = 0.030). In this study, the median duration of response was only 6 months, primarily because of recurrences in the central nervous system.
Taken together, the M.D. Anderson Hospital phase II studies suggest that whereas alternating biotherapy and chemotherapy does not produce additive antitumor activity, sequential biochemotherapy using the CVD/BIO sequence appears to produce superior results when compared with CVD alone and with BIO/CVD. Concurrent biochemotherapy also appears to be superior to CVD alone and is more convenient and less toxic than sequential therapy. It is unclear, however, whether concurrent biochemotherapy is as effective as sequential biochemotherapy.
Ongoing Trials--Because the above-described biochemotherapy regimens have shown encouraging phase II results with response rates consistently above 50% and possible improvement in survival, a randomized phase III trial is currently being conducted at M.D. Anderson Hospital to compare sequential biochemotherapy with CVD alone. A similar study is being conducted at the NCI. In addition, based on the high response rate with concurrent biochemotherapy in patients with advanced disease and the lower toxicity of this biochemotherapy regimen compared with that of sequential biochemotherapy, we are evaluating the use of concurrent biochemotherapy in the neoadjuvant setting for patients with measurable locoregional disease. Finally, a series of laboratory studies is being performed in conjunction with these protocols in an attempt to better understand the mechanism of antitumor effect of the biochemotherapy regimens.
References:
1. Wingo P, Tong T, Bolden S: Cancer Statistics, 1995. CA Cancer J Clin 45:8-30, 1995.
2. Legha S: Current therapy for malignant melanoma. Semin Oncol 16: 34-44, 1989.
3. Jacquillat C, Khayat D, Banzet P, et al: Final report of the French multicenter phase II study of the nitrosourea fotemustine in 153 evaluable patients with disseminated malignant melanoma including patients with cerebral metastases. Cancer 66:1873-1878, 1990.
4. Khayat D, Avril M, Auclerc G, et al: Clinical value of the nitrosourea fotemustine in disseminated malignant melanoma: Overview on 1022 patients including 144 patients with cerebral metastases. Proc Am Soc Clin Oncol 12:393, 1993.
5. Kirkwood J, Agarwala S: Systemic cytotoxic and biologic therapy of melanoma. PPO Updates 7:1-16, 1993.
6. Einzig A, Schuchter L, Wadler S, et al: Phase II trial of taxotere (RP 56976) in patients with metastatic melanoma previously untreated with cytotoxic chemotherapy. Proc Am Soc Clin Oncol 13:395, 1994.
7. Bedikian A, Legha S, Eton O, et al: Phase II trial of docetaxel (taxotere, RP 56976) in patients with advanced cutanous malignant melanoma previously untreated with chemotherapy. Proc Am Assoc Cancer Res 35:86, 1994.
8. Bleehen N, Newlands E, Lee S, et al: Cancer Research Campaign phase II trial of temozolomide in metastatic melanoma. J Clin Oncol 13:910-913, 1995.
9. Ahmann D, Hahn R, Bisel H: Evaluation of 1-(2 chloroethyl-3,4-methylcyclohexyl)-1-nitrosourea (methyl-CCNU, NSC 9541 1) vs combined imidazole carboxamide (NSC 45388) and vincristine (NSC 67574) in palliation of disseminated malignant melanoma. Cancer 33:615-620, 1973.
10. Wittes R, Wittes J, Golbey R: Combination chemotherapy in metastatic melanoma: A randomized study of three dacarbazine-containing combinations. Cancer 41:415-421, 1978.
11. Chauvergne J, Bui N, Cappelaere P, et al: Chemotherapy in advanced malignant melanoma: Results of a controlled trial comparing a combination of dacarbazine and detorubicin with dacarbazine alone. Semaine Des Hopitaux 58:2696-2701, 1982.
12. Costanzi J, Al-Sarraf M, Groppe C, et al: Combination chemotherapy plus BCG in the treatment of disseminated malignant melanoma: A Southwest Oncology Group study. Med Ped Oncol 10:251-258, 1982.
13. Luikart S, Kemealey G, Kirkwood J: Randomized phase III trial of Vinblastine, bleomycin, cis-dichlorodiammine-platinum versus dacarbazine in malignant melanoma. J Clin Oncol 2:164-168, 1984.
14. Bajetta E, Buzzoni R, Viviani S, et al: Prospective randomized trial in advanced malignant melanoma with cisplatin, vindesine, and etoposide vs. cisplatin, vindesine, and lomustine. Am J Clin Oncol 8:401-405,1985.
15. Carmo-Pereira J, Costa F, Henriques E: Cytotoxic chemotherapy of disseminated cutaneous malignant melanoma-a prospective and randomized clinical trial of procarbazine, vindesine, and lomustine versus procarbazine, dacarbazine, and lomustine. Br J Cancer 22:1435-1439, 1986.
16. Buzaid A, Legha S, Winn R, et al: Cisplatin, vinblastine, and dacarbazine versus dacarbazine alone in metastatic melanoma: preliminary results of a phase III Cancer Community Oncology Program (CCOP) trial. Proc Am Soc Clin Oncol 12:389, 1993.
17. McClay E, McClay M: Tamoxifen: Is it useful in the treatment of patients with metastatic melanoma. J Clin Oncol 12:617-626, 1994.
18. Del Prete S, Maurer L, O'Donnell J, et al: Combination chemotherapy with cisplatin, carmustine, dacarbazine, and tamoxifen in metastatic melanoma. Cancer Treat Rep 68:1403, 1984.
19. McClay E, Mastrangelo M, Berd D, et al: Effective combination chemo/hormonal therapy for malignant melanoma: Experience with three consecutive trials. Int J Cancer 50:553-556, 1992.
20. Lattanzi S, Tosteson T, Maurer L, et al: Dacarbazine (D), cisplatin (C), and carmustine (B), ± tamoxifen (T) in the treatment of patients with metastatic melanoma (MM). Proc Am Soc Clin Oncol 12:390, 1993.
21. Mastrangelo M, Nathan F, Maguire H, et al: Trials with combination chemotherapy and with active specific immunotherapy. Melanoma Res 3:33, 1993.
22. Richards J, Gilewski T, Ramming K, et al: Effective chemotherapy for melanoma after treatment with interleukin-2. Cancer 69:427, 1992.
23. Fierro M, Bertero M, Novelli M, et al: Therapy for metastatic melanoma: effective combination of dacarbazine, carmustine, cisplatin and tamoxifen. Melanoma Res 3:127-131, 1993.
24. Reintgen D, Saba H: Chemotherapy for stage 4 melanoma: A three-year experience with cisplatin, DTIC, BCNU, and tamoxifen. Semin Surg Oncol 9:251-255, 1993.
25. Spitler L, Good J, Jacobs M, et al: The use of high-dose tamoxifen to potentiate the anti-tumor effects of cytotoxic chemotherapy in patients with metastatic melanoma. Proc Am Soc Clin Oncol 13:397, 1994.
26. Buzaid A, Murren J, Durivage H: High-dose cisplatin with dacarbazine and tamoxifen in the treatment of metastatic melanoma. Cancer 68:1238-1241, 1991.
27. Flaherty L, Liu P, Daniels D, et al: The addition of tamoxifen to dacarbazine and cisplatin in a SWOG phase II trial in metastatic malignant melanoma stage IV. Proc Am Soc Clin Oncol 12:394, 1993.
28. Thomson D, Walpole E, Beadle G, et al: High-dose tamoxifen does not enhance the activity of dacarbazine in metastatic melanoma. Proc Am Soc Clin Oncol 12:392, 1993.
29. Foshag L, Morton D, Nizze J, et al: Response to chemotherapy in melanoma patients after active specific immunotherapy (ASI) with melanoma cell vaccine. Proc Am Soc Clin Oncol 12:396, 1993.
30. Berd D, McLaughlin C, Hart E, et al: Short course, high-dose tamoxifen with cytotoxic chemotherapy for metastatic melanoma. Proc Am Soc Clin Oncol 10:291, 1991.
31. Thomson D, Adena M, McLeod G, et al: Interferon-alfa-2a does not Improved response or survival when combined with dacarbazine in metastatic malignant melanoma. Melanoma Res 3:133-138, 1993.
32. Legha S, Ring S, Bedikian A, et al: Lack of benefit from tamoxifen added to a regimen of cisplatin (C), vinblastine (V), DTIC (D) and alpha interferon (IFN) in patients with metastatic melanoma. Proc Am Soc Clin Oncol 12:388, 1993.
33. Ferri W, Agarwala S, Kirkwood J, et al: Carboplatin and dacarbazine +/- tamoxifen for metastatic melanoma. Proc Am Soc Clin Oncol 13:394, 1994.
34. Cocconi G, Bella M, Calabresi F, et al: Treatment of metastatic malignant melanoma with dacarbazine plus tamoxifen. N Engl J Med 327:516-523, 1992.
35. Nathanson L, Meelu M, Losada R: Chemohormone therapy of metastatic melanoma with megestrol acetate plus dacarbazine, carmustine, and cisplatin. Cancer 73:98-102, 1994.
36. Gonzales R, Sanchez A, Ferguson J, et al: Melatonin therapy of advanced human malignant melanoma. Melanoma Res 1:237-243, 1991.
37. Margolin K, Doroshow J, Akman S, et al: Treatment of advanced melanoma with cisdiamminedichloroplatinum (CDDP) and alpha interferon (aIFN). Proc Am Soc Clin Oncol 9:277, 1990.
38. Morton R, Creagan E, Schaid D, et al: Phase III trial of recombinant leukocyte A interferon (IFN-alpha-2a) plus 1,3-bis(2-chloroethyl)-l-nitrosourea (BCNU) and the combination cimetidine with BCNU in patients with disseminated malignant melanoma. Am J Clin Oncol (CCT) 14:152-155, 1991.
39. Smith K, Green J, Eccles J: Interferon alpha-2a and vindesine in the treatment of advanced malignant melanoma. Eur J Cancer 28:438-441, 1992.
40. Stark J, Schulof R, Wiemann M, et al: Alpha interferon and chemo-hormonal therapy in advanced melanoma: A phase I/II NBSG/MAOP study. Proc Am Soc Clin Oncol 12:392, 1993.
41. Feun L, Savaraj N, Moffat F, et al: Combination of BCNU, DTIC, cisplatin, and tamoxifen with alpha-interferon in stage IV melanoma, in Advances in the Biology and Clinical Management of Melanoma: 38th Annual Clinical Conference, p 101. Houston, Texas, 1995.
42. Schultz M, Buzaid A, Poo W: A phase II study of interferon-alpha 2b with dacarbazine, cisplatin, carmustine, and tamoxifen in metastatic melanoma. Melanoma Res in press, 1995.
43. Kirkwood J, Emstoff M, Giuliano A, et al: Interferon alpha 2a and dacarbazine in melanoma. J Natl Cancer Inst 82:1062-1063, 1990.
44. Bajetta E, Di Leo A, Zampino M, et al: Multicenter randomized trial of dacarbazine alone or in combination with two different doses and schedules of interferon alfa-2a in the treatment of advanced melanoma. J Clin Oncol 12:806, 1994.
45. Falkson C, Falkson G, Falkson H: Improved results with the addition of interferon alfa-2a to dacarbazine in the treatment of patients with metastatic malignant melanoma. J Clin Oncol 9:1403-1408, 1991.
46. Buzaid A, Legha S: Combination of chemotherapy with interleukin-2 and interferon-alfa for the treatment of advanced melanoma. Semin Oncol 21(6;suppl 1):23-28, 1994.
47. Demchak P, Mier J, Robert N, et al: Interleukin-2 and high-dose cisplatin in patients with metastatic melanoma: A pilot study. J Clin Oncol 9:1821-1830, 1991.
48. Flaherty L, Robinson W, Redman B, et al: A phase II study of dacarbazine and cisplatin in combination with outpatient administered IL-2 in metastatic melanoma. Cancer 71:3520, 1993.
49. Atkins M, O'Boyle K, Sosman J, et al: Multiinstitutional phase II trial of intensive combination chemoimmunotherapy for metastatic melanoma. J Clin Oncol 12:1553-1560, 1994.
50. Richards J, Mehta N, Ramming K, et al: Sequential chemoimmunotherapy in the treatment of metastatic melanoma. J Clin Oncol 10: 1338-1343, 1992.
51. Rixe O, Benhammouda A, Antoine E, et al: Final results of a prospective multicentric study on 91 metastatic malignant melanoma patients treated by chemoimmunotherapy with cisplatin, IL-2, and interferon-alpha. Proc Am Soc Clin Oncol 13:399, 1994.
52. Dorval T, Negrier S, Chevreau C, et al: Results of a French multicentric randomized trial of chemoimmunotherapy (cisplatin, IL-2, with or without IFN) in metastatic malignant melanoma. Proc Am Soc Clin Oncol 13:395, 1994.
53. Richards J, Mehta N, Schroeder L, et al: Sequential chemotherapy/immunotherapy for metastatic melanoma. Proc Am Soc Clin Oncol 11:346, 1992.
54. Legha S, Buzaid A, Ring S, et al: Improved results of treatment of metastatic melanoma with combined use of biotherapy and chemotherapy. Proc Am Soc Clin Oncol 13:394, 1994.
55. Ron I, Mordish Y, Eisenthal A, et al: A phase II study of combined administration of dacarbazine and carboplatin with home therapy of recombinant IL-2 and interferon-alpha 2a in patients with advanced malignant melanoma. Cancer Immunol Immunother 38:379-384, 1994.
Articles in this issue
over 30 years ago
PET Scanning Said to Save Money and Improve Staging of Lung Cancerover 30 years ago
Ribozyme Gene Therapy for Cancer Nears Clinical Trialsover 30 years ago
Networking May Be Key to Academic Cancer Survival Under Managed Careover 30 years ago
Chances of Worldwide Plagues Increasing, Scientists Sayover 30 years ago
Changes in Laryngeal Preservation Study Help Increase Accrualover 30 years ago
Initiatives Can Contain Costs and Increase Quality of Nursing Careover 30 years ago
New 'Calibrator' Should Improve Prostate Cancer TestingNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.
Related Content



MCL Workshop Proves Essential for Moving the Needle Forward in Research









































