T-DM1 in Early HER2+/HR+ Breast Cancer Offers Good Response Rates
T-DM1 administered for 12 weeks with or without endocrine therapy yields good rates of pathologic complete response in women with HER2-positive/hormone receptor–positive breast cancer, according to a new randomized trial.
Trastuzumab emtansine (T-DM1) administered for 12 weeks with or without endocrine therapy yields good rates of pathologic complete response in women with HER2-positive/hormone receptor (HR)-positive breast cancer, according to a new randomized trial. Responses were better than with trastuzumab combined with endocrine therapy.
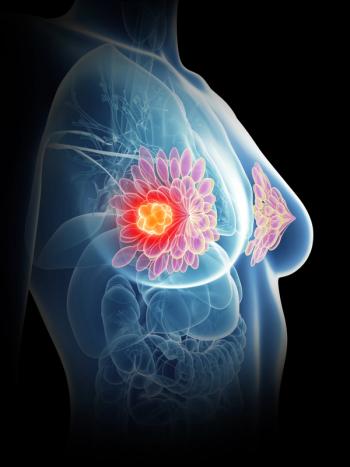
HER2-positive/HR-positive breast cancer is associated with both lower sensitivity to chemotherapy and slightly better outcomes, compared with HER2-positive/HR-negative disease. The West German Study Group’s ADAPT trial “was conducted specifically in patients with HR-positive/HER2-positive early breast cancer because the addition of another targeted anti-endocrine therapy represented a valid alternative to systemic chemotherapy,” wrote authors led by Nadia Harbeck, MD, of the University of Munich in Germany.
The prospective, neoadjuvant trial included 375 patients with early breast cancer that was HER2-positive/HR-positive. They were randomized to receive either 12 weeks of T-DM1 with (127 patients) or without endocrine therapy (119 patients), or to trastuzumab with endocrine therapy (129 patients); patient characteristics were well-balanced between the groups. Results were
Pathologic complete response was observed in 41.5% of the T-DM1 plus endocrine therapy patients, 41% of the T-DM1 alone patients, and in 15.1% of the trastuzumab plus endocrine therapy patients (P < .001 for both T-DM1 arms vs trastuzumab). Though pathologic complete response rates were higher in postmenopausal women across the study arms, these differences did not reach significance.
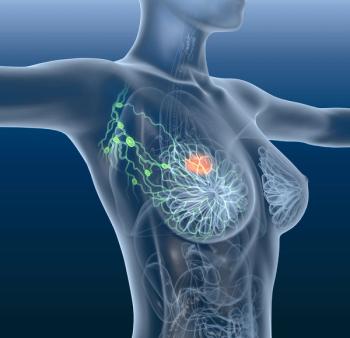
Approximately two-thirds of patients (67.1%) were deemed to be early responders, as determined by changes to Ki-67 level or low cellularity of tumors. Pathologic complete responses were significantly more likely in these early responders than in nonresponders, at 35.7% compared with 19.8%, for an odds ratio of 2.2 (95% CI, 1.24–4.19; P = .005).
Toxicity was similar in the two T-DM1 arms. In those two groups, 7.5% of patients had at least one grade 3 or higher adverse event, compared with 4.1% of trastuzumab patients (P = .26). The most common adverse events were increases in transaminases. The authors noted that no new T-DM1 safety signals were found in the study.
“In summary, only 4 cycles of neoadjuvant T-DM1 in HER2-positive/HR-positive early breast cancer yield substantial pathologic complete response rates-quite comparable to standard chemotherapy plus trastuzumab (or even to dual HER2 blockade),” the authors concluded. “T-DM1 may be an efficient and safe alternative for patients who are not suited for systemic chemotherapy in this setting; the addition of endocrine therapy does not seem to play a crucial role.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.