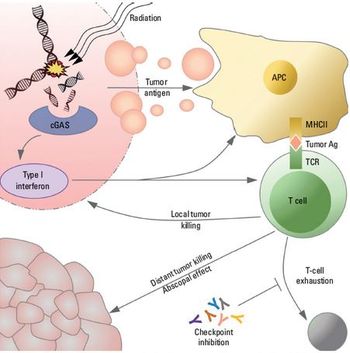
In this article, we discuss radiation’s immunomodulatory effects, with particular attention to the impact of dose and fractionation on the antitumoral response.

Your AI-Trained Oncology Knowledge Connection!

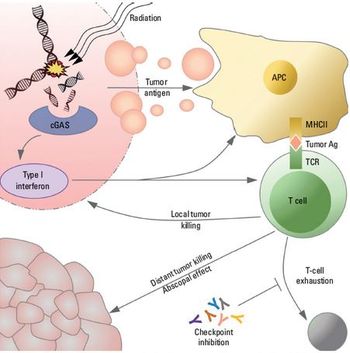
In this article, we discuss radiation’s immunomodulatory effects, with particular attention to the impact of dose and fractionation on the antitumoral response.

Primary neuroendocrine neoplasms of the lung represent a clinical spectrum of tumors ranging from the relatively benign and slow-growing typical carcinoid to the highly aggressive small-cell lung carcinoma. The rarity of carcinoids has made the role of radiation therapy in their management controversial. This review considers the results of published studies to generate treatment recommendations and identify areas for future research. Surgery remains the standard of care for medically operable disease. Histology plays the most important role in determining the role of adjuvant radiation. Resected typical carcinoids likely do not require adjuvant therapy irrespective of nodal status. Resected atypical carcinoids and large-cell neuroendocrine carcinomas have a significant risk of local failure, for which adjuvant radiation likely improves local control. Definitive radiation is warranted in unresectable disease. Palliative radiation for symptomatic lesions has demonstrated efficacy for all histologies. Collaborative group trials are warranted.

Lung cancer is estimated to be the second most commonly diagnosed cancer in both men and women in 2006, and the leading cause of cancer mortality. Non-small-cell lung cancer represents the majority of such cases. Most of these patients have locally advanced disease at presentation and are not eligible for curative resection. For the minority of patients who are technically resectable at presentation, lobectomy or pneumonectomy and pathologic mediastinal nodal staging offer the best overall survival. The high rate of comorbid medical illness and poor baseline pulmonary function in this population, however, make many such early-stage patients medically inoperable. For these patients, conventional single-modality radiotherapy has been the primary definitive treatment option, as discussed in part 1 of this article, which appeared in last month's issue. Numerous retrospective reports demonstrate long-term disease-free and overall survival data that are modestly superior to that expected after observation, but both local and distant failure continue to be significant risks. Investigation of radiotherapy dose escalation is ongoing, in an effort to improve local control while maintaining minimal toxicity. Additionally, emerging evidence suggests that new modalities, such as stereotactic radiosurgery and radiofrequency ablation, may also be potentially curative treatment alternatives. These modalities are addressed in part 2.

Lung cancer is estimated to be the second most commonly diagnosed cancer in both men and women in 2006, and the leading cause of cancer mortality. Non-small-cell lung cancer represents the majority of such cases. Most of these patients have locally advanced disease at presentation and are not eligible for curative resection. For the minority of patients who are technically resectable at presentation, lobectomy or pneumonectomy and pathologic mediastinal nodal staging offer the best overall survival. The high rate of comorbid medical illness and poor baseline pulmonary function in this population, however, make many such early-stage patients medically inoperable. For these patients, conventional single-modality radiotherapy has been the primary definitive treatment option, as discussed in part 1 of this two-part article. Numerous retrospective reports demonstrate long-term disease-free and overall survival data that are modestly superior to that expected after observation, but both local and distant failure continue to be significant risks. Investigation of radiotherapy dose escalation is ongoing, in an effort to improve local control while maintaining minimal toxicity. Additionally, emerging evidence suggests that new modalities, such as stereotactic radiosurgery and radiofrequency ablation, may also be potentially curative treatment alternatives. These modalities will be addressed in part 2.

Malnutrition plays a key role in the morbidity of head and neckcancer patients receiving surgery, chemotherapy, radiotherapy, or combined-modality therapy. In addition to weight lost prior to the diagnosisof head and neck cancer, the patient may lose an additional 10% ofpretherapy body weight during radiotherapy or combined-modality treatment.A reduction of greater than 20% of total body weight results inan increase in toxicity and mortality. Severe toxicity can result in prolongedtreatment time, which has been implicated in poor clinical outcome.Early intervention with nutritional supplementation can reducethe chance of inferior outcome in patients at high risk of weight loss.The preferred route of nutritional support for these patients is enteralnutrition. Two commonly used methods for enteral feedings arenasoenteric and percutaneous endoscopic gastrostomy. It is importantto take into account the ethical considerations involved in providinglong-term nutritional support, particularly for patients with terminalconditions. Nutritional directives are best evaluated throughmultidisciplinary efforts, including input from the patient as well asmembers of the nursing, nutritionist, and medical staff.

Published: November 1st 2006 | Updated:

Published: June 1st 2006 | Updated:

Published: July 1st 2006 | Updated:

Published: March 1st 2005 | Updated:

Published: July 15th 2018 | Updated: