- ONCOLOGY Vol 35, Issue 7
- Volume 35
- Issue 7
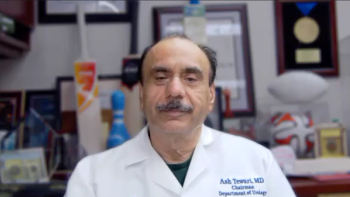
Advanced Penile Cancer Presenting With Renal Failure
“MK,” a man aged 67 years, presented with fatigue and nausea to his primary care physician. CT staging scans confirmed the primary tumor and a suspicious left 1.2-cm inguinal lymph node but no distant metastases. MRI of the pelvis revealed complete replacement of the penis with tumor as well as invasion into the scrotum and bilateral groin soft tissue; additionally, early pubic bone invasion was present, with left groin lymphadenopathy. Biopsy verified squamous cell carcinoma of the penis, and discussion with the multidisciplinary team uroradiologist confirmed bony invasion.
Oncology (Williston Park). 2021;35(7):425-428.
DOI: 10.46883/ONC.2021.3507.0425
“MK,” a man aged 67 years, presented with fatigue and nausea to his primary care physician. Routine blood tests showed a stage III acute kidney injury and the patient was admitted urgently into the hospital for investigation. On initial assessment by the nursing staff, with urine dip and bladder scan, he was found to have a large fungating mass on his penis. Upon further questioning, MK reported having had trouble with urination for a number of years and that he had been concealing the mass for at least 1 year due to embarrassment. He required a suprapubic catheter as the mass had completely obstructed his urethra. Clinical examination revealed that the external component on the penile shaft was entirely destroyed by the tumor, with extension deep into the entirety of the scrotum, and perineal soft-tissue invasion was also apparent.
CT staging scans confirmed the primary tumor and a suspicious left 1.2-cm inguinal lymph node but no distant metastases. MRI of the pelvis revealed complete replacement of the penis with tumor as well as invasion into the scrotum and bilateral groin soft tissue; additionally, early pubic bone invasion was present, with left groin lymphadenopathy. Biopsy verified squamous cell carcinoma of the penis, and discussion with the multidisciplinary team uroradiologist confirmed bony invasion (Figure 1).
What treatment options would you consider for this patient?
CORRECT ANSWER: C
A. While palliative or neoadjuvant chemotherapy may be an appropriate option, bleomycin/methotrexate/cisplatin, which has been used neoadjuvantly in penile cancer, may result in high levels of bleomycin-related toxicity.1
B. Debulking in this patient would be an extremely morbid surgery, requiring bony resection; it would also likely result in positive margins and so would not be appropriate. Surgical treatment is discussed later in the article, including management of pelvic and inguinal lymph nodes.
C. Correct
D. Palliative local debulking for penile cancer may be appropriate in some circumstances, but this case displays extensive cutaneous and bony involvement. Therefore, local debulking is likely to result in positive margins and poor wound healing, potentially causing further morbidity in what is likely to be a palliative case.
E. While palliative radiotherapy may be an appropriate treatment option, a single 8 Gy fraction is unlikely to be effective given the large area requiring treatment.
Due to the extent of disease and after local bony involvement was confirmed, the disease was deemed inoperable. Given MK’s surprisingly limited disease and relative fitness otherwise, he was referred to oncology for assessment of fitness for treatment. It was felt that given the extent of disease and patient fitness, radiotherapy for local control might be the best option to palliate symptoms. Physicians considered concurrent and neoadjuvant chemotherapy, but because MK’s renal failure was slow to improve, the concern was that the delay in time caused by chemotherapy might result in the radiotherapy field no longer being feasible if the cancer were to progress further.
Therefore, treatment was planned with 60 Gy in 30 fractions, with a 6-Gy boost to the primary site using volumetric arc technique, and the use of 1-cm wax bolus covering the gross total volume of the penis and nodes plus margin (Figure 2). MK successfully completed radical radiotherapy with acute grade 2 radiation dermatitis. Initial scans showed a response to treatment, although some of the necrotic residual tumor bed was slow to resolve. The suprapubic catheter was required for ongoing urinary diversion as the tumor shrinkage had essentially resulted in a loss of any normal penile anatomy (Figure 3). Scans continued to show an improvement in the appearance of the tumor bed until there was no discernible remaining cancer. The patient has remained on follow-up for 2 years with no evidence of distant disease or local progression. Of interest, MK developed a transient viral human papillomavirus (HPV) infection in the form of warts at the scrotum 18 months after completing radiotherapy and went on to have HPV immunization.
Background
Penile cancer incidence in developed countries is rare, and management requires careful consideration. In the United Kingdom, it accounts for only about 0.2% to 0.6% of cancers in men and 2.9 new cases per year per 100,000 in Scotland.2,3 Similarly, in the United States, reported incidence is low at 0.81 per 100,000.4 However, in developing countries the incidence can be significantly higher, with incidence of up to 6.15 per 100,000 in such localities as Maranhão, Brazil.5 Evidence indicates, however, that incidence may be increasing in developed countries: For example, in Saxony, Germany, reported incidence has increased from 1.2 per 100,000 in 1961 to 1.8 per 100,000 in 2012.6
Risk factors for penile cancer that have been investigated include age, sexual history, and socioeconomic status.3 Historically, penile cancer has been considered primarily a disease of the elderly; however, evidence increasingly supports that a significant proportion of cases occur in younger men; a prospective study showed that a quarter of patients were diagnosed when aged less than 50 years.7 This may relate to cases driven by HPV, as it is known that HPV-related cancer incidence has generally increased in past decades and prior sexual history can play an important role in this particular cancer subgroup.8 Interestingly, HPV-positive disease may be associated with better survival, a phenomenon that has also been seen in head-and-neck and oropharyngeal cancers.9 The proportion of penile cancers that are HPV driven is lower than in other related groups, such as cervical cancer, but up to one-third of penile cancers may be HPV related.10,11 Some penile cancers are associated with inflammation or chronic inflammatory processes, as chronic inflammatory processes including balanitis, phimosis, and lichen sclerosis increase penile cancer risk. Smoking is another risk factor.12 Interestingly, neonatal circumcision appears to be associated with a reduced risk of penile cancer.13 Lower socioeconomic status has also been associated with an increased risk of penile cancer, and low educational level has also been associated with later presentation of more advanced primary tumors.14 Increased rates of penile cancer have been noted in patients of lower socioeconomic backgrounds, both in developing and developed countries.14,15
Presentation and Staging
Staging of penile cancer is important (Table). The factor that most strongly influences survival and outcome is lymph node staging; 5-year survival is only 25% in patients with 3 or more positive lymph nodes compared with 77% in patients with 2 or fewer positive nodes.16 Similarly, pelvic disease and bilateral disease are also associated with poor prognosis; there are few survivors at 5 years in the presence of pelvic nodes.17 Groin node dissection is therefore an important consideration in patients undergoing radical surgery. However, nodal dissection significantly increases the risk of complications such as lymphedema.17 Another complicating factor is the presence of clinically occult lymph node metastases, which affects a significant proportion (up to 20%) of patients.18 While advanced-stage penile cancer can cause significant problems locoregionally, the risk of distant metastasis is low and tends to occur late in the course of disease. Metastatic disease at presentation is seen in less than 5% of patients.19
Treatment
Early disease
Penile cancer treatment varies depending on stage, site, and grade of disease. Early-stage T1 cancers that are grade 1 or 2 may be treated with conservative organ-preserving techniques such as surgery, but treatments have also included Mohs micrographic surgery, laser therapy, and radiotherapy in the form of interstitial implant brachytherapy.20-22 More than 90% of recurrences occur in the first 5 years, and patients therefore require close follow-up for locoregional recurrence, particularly in the first 2 years after follow-up when the risk of local recurrence is highest.23 In T1, grade 3 disease, surgery tends to require more extensive intervention and may require glansectomy with reconstruction with wider margins (8 mm), due to the high risk of regional spread.24,25 Depending on site, it may still be possible to maintain functionality for urination and in some cases sexual function. Brachytherapy and external beam therapy can also be considered but require close surveillance for recurrence.26,27 Brachytherapy can be an attractive option as it is superior to external beam treatment in providing organ preservation, particularly in T1 or T2 disease.28
Locally advanced disease
The management of locally advanced penile cancer is somewhat complex and can be controversial. In particular, management of lymph nodes can be a matter of debate. As previously mentioned, even clinically node-negative cancers can hide occult lymph node metastases, and for patients with T1b or greater disease, a modified lymph node dissection or sentinel node biopsy is recommended.29 In clinically node-positive disease, inguinal lymph node dissection is generally recommended, and consideration should be given to neoadjuvant chemotherapy in bulky or fixed N3 disease.30 Further, the presence of inguinal lymph nodes increases the risk of pelvic nodal involvement; the presence of 3 or more inguinal nodes has been associated with at least a 4-fold greater risk of pelvic nodal disease, with a rate of more than 20%.31 The European Association of Urology (EAU) recommends pelvic lymph node dissection in all patients with 2 or more inguinal node metastases.32 Adjuvant chemotherapy may also be considered in N2 or N3 disease following lymphadenectomy; retrospective data support this and demonstrate good rates of disease-free survival compared with historical controls.33 Several chemotherapy regimens, including cisplatin/5-fluorouracil (5FU), have been proposed in the adjuvant and neoadjuvant settings.34,35 More recently, the more intensive paclitaxel/cisplatin/ifosfamide regimen showed a good objective response rate (ORR; 50%) in the neoadjuvant setting, and 3 of 30 men had complete responses in a phase 2 trial (NCT00512096).36
The role of radiotherapy
The role of adjuvant radiotherapy remains a matter for debate, and management guidelines do not universally agree. The EAU penile cancer guidelines do not routinely recommend consideration of adjuvant radiotherapy; however, a number of centers propose a role for adjuvant radiotherapy, particularly in disease that may not be feasibly operable or has not responded to neoadjuvant chemotherapy.9,37-39 Considering radiotherapy also may have some advantage in cases of extracapsular spread, which is a particularly poor prognostic factor.40 In this controversial field of perioperative treatment, the InPACT trial (International Penile Advanced Cancer Trial, an
In some patients, surgery is not feasible due to the location of disease or its extent, or due to patient fitness or wishes. In these cases, radiotherapy can be considered with or without chemotherapy for aggressive local control, as demonstrated in MK’s case.42
Systemic palliative options
Cisplatin tends to be the backbone for penile cancer treatment regimens. Taxanes, however, have also demonstrated response. Still, because trials have been small, reported responses to treatment have been variable.43,44 The combination of docetaxel, cisplatin, and 5FU was evaluated in 29 patients with locally advanced or metastatic disease by the UK National Cancer Research Institute penile cancer subgroup; the overall ORR was 38.5%.45 More recently, the VinCap trial (NCT02057913) evaluated vinflunine in locally advanced or metastatic penile cancer and reported a clinical benefit rate of 45.5%. The authors concluded that further research could be of value with this novel vinca alkaloid.46 Other systemic options reviewed in penile cancer have included EGFR-targeted therapies such as cetuximab (Erbitux); a review of treatment with cetuximab, erlotinib (Tarceva), and gefitinib (Iressa) demonstrated response in 23.5% of patients.47
Penile cancer is rare, and like many rare cancers, it does not attract a great deal of investigation of novel agents. Therefore, treatments such as immunotherapy in penile cancer have not been rigorously tested.48 Indeed, 1 phase 2 trial attempted to investigate the use of pembrolizumab
(Keytruda) in penile cancer but was closed early due to poor recruitment (NCT02837042). Case reports of immunotherapy use in penile cancer have indicated that durable responses can be seen even after the failure of multimodal treatment. One report described a man, aged 79 years, with chemo- and radioresistant disease who showed durable response on atezolizumab. Further responses of up to 38 months were demonstrated in a case series using pembrolizumab.49,50 These case reports demonstrate the challenge of caring for patients with rare cancers as trials are expensive and difficult to recruit to. Results are eagerly awaited of current clinical trials that are assessing the efficacy of immunotherapy as monotherapy or in combination with radiotherapy in penile carcinoma (NCT03686332; NCT03391479). Our center also has experience in using palliative immunotherapy in penile cancer that generated objective response in otherwise treatment-resistant disease (unpublished data).
More broadly, the use of T-cell therapy in HPV-related cancers has been investigated with durable response rates. Although this is a majority cervical cancer population, treatment by molecular profiling may have application for HPV-related penile cancers.51 Participation in trials that distinguish disease by molecular subtype may be advantageous in penile cancer, due to its overlap with other squamous cancers and targetable pathways may be utilized.52
Final Thoughts
It is rare for specialists, much less primary care physicians, to see penile cancer. Disease heterogeneity and late presentation mean that treatment planning can be challenging and is often fraught with controversy. Cumulative investigation into the importance of HPV and of key driver mutations affecting prognosis is broadening our understanding of this disease. The crucial factor to improving outcomes in penile cancer will be clinical trial engagement and successful recruitment of patients, with utilization of early-phase and basket-design trials. An important step in recognizing the challenge of treating these rare cancers is the formation of the Global Society of Rare Genitourinary Tumors (
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References
1. Haas GP, Blumenstein BA, Gagliano RG, et al. Cisplatin, methotrexate and bleomycin for the treatment of carcinoma of the penis: a Southwest Oncology Group study. J Urol.1999;161(6):1823-1825.
2. Campbell RA, Slopnick EA, Ferry EK, Zhu H, Kim SP, Abouassaly R. Disparity between pre-existing management of penile cancer and NCCN guidelines. Urol Oncol.2017;35(8):531.e9-531.e14. doi:10.1016/j.urolonc.2017.03.002
3. National Cancer Intelligence Network; Cancer Research UK. Cancer by deprivation in England: incidence, 1996-2010, Mortality, 1997-2011. Public Health England. 2014. Accessed November 30, 2019.
4. Douglawi A, Masterson TA. Updates on the epidemiology and risk factors for penile cancer. Transl Androl Urol.2017;6(5):785-790. doi:10.21037/tau.2017.05.19
5. Coelho RWP, Pinho JD, Moreno JS, et al. Penile cancer in Maranhão, Northeast Brazil: the highest incidence globally? BMC Urol.2018;18(1):50. doi:10.1186/s12894-018-0365-0
6. Schoffer O, Neumann A, Stabenow R, et al. Penile cancer - incidence, mortality, and survival in Saxony, Germany. Urol Oncol.2019;37(4):295.e1-295.e8. doi:10.1016/j.urolonc.2018.12.003
7. Hegarty PK, Kayes O, Freeman A, Christopher N, Ralph DJ, Minhas S. A prospective study of 100 cases of penile cancer managed according to European Association of Urology guidelines. BJU International.2006;98(3):526-531. doi:10.1111/j.1464-410X.2006.06296.x
8. Hansen BT, Campbell S, Nygård M. Long-term incidence trends of HPV-related cancers, and cases preventable by HPV vaccination: a registry-based study in Norway. BMJ Open.2018;8(2):e019005. doi:10.1136/bmjopen-2017-019005
9. Yuan Z, Naghavi AO, Tang D, et al. The relationship between HPV status and chemoradiotherapy in the locoregional control of penile cancer. World J Urol.2018;36(9):1431-1440. doi:10.1007/s00345-018-2280-0
10. Alemany L, Cubilla A, Halec G, et al; HPV VVAP Study Group. Role of human papillomavirus in penile carcinomas worldwide. Eur Urol.2016;69(5):953-961. doi:10.1016/j.eururo.2015.12.007
11. Alemany L, Saunier M, Alvarado-Cabrero I, et al; HPV VVAP Study Group. Human papillomavirus DNA prevalence and type distribution in anal carcinomas worldwide. Int J Cancer.2015;136(1):98-107. doi:10.1002/ijc.28963
12. Dillner J, von Krogh G, Horenblas S, Meijer CJ. Etiology of squamous cell carcinoma of the penis. Scand J Urol Nephrol Suppl.2000;(205):189-193. doi:10.1080/00365590050509913
13. Daling JR, Madeleine MM, Johnson LG, et al. Penile cancer: importance of circumcision, human papillomavirus and smoking in in situ and invasive disease.Int J Cancer.2005;116(4):606-616. doi:10.1002/ijc.21009
14. Torbrand C, Wigertz A, Drevin L, et al. Socioeconomic factors and penile cancer risk and mortality; a population-based study. BJU Int.2017;119(2):254-260. doi:10.1111/bju.13534
15. Bezerra Vieira C, Feitoza L, Pinho J, et al. Profile of patients with penile cancer in the region with the highest worldwide incidence. Sci Rep. 2020;10(1):2965. doi:10.1038/s41598-020-59831-5
16. Zhu Y, Ye D-W. Lymph node metastases and prognosis in penile cancer. Chin J Cancer Res. 2012;24(2):90-96. doi:10.1007/s11670-012-0090-2
17. Pandey D, Mahajan V, Kannan RR. Prognostic factors in node-positive carcinoma of the penis. J Surg Oncol. 2006;93(2):133-138. doi: 10.1002/jso.20414
18. Kieffer JM, Djajadiningrat RS, Van Muilekom EAM, Graafland NM, Horenblas S, Aaronson NK. Quality of life for patients treated for penile cancer. J Urol. 2014;192(4):1105-1110. doi:10.1016/j.juro.2014.04.014
19. Rippentrop JM, Joslyn SA, Konety BR. Squamous cell carcinoma of the penis: evaluation of data from the Surveillance, Epidemiology, and End Results Program. Cancer. 2004;101(6):1357-1363. doi:10.1002/cncr.20519
20. Windahl T, Andersson S-O. Combined laser treatment for penile carcinoma: results after long-term followup. J Urol. 2003;169(6):2118-2121. doi:10.1097/01.ju.0000067361.81295.a2
21. Shindel AW, Mann MW, Lev RY, et al. Mohs micrographic surgery for penile cancer: management and long-term followup.J Urol. 2007;178(5):1980-1985. doi:10.1016/j.juro.2007.07.039
22. de Crevoisier R, Slimane K, Sanfilippo N, et al. Long-term results of brachytherapy for carcinoma of the penis confined to the glans (N- or NX). Int J Radiat Oncol Biol Phys. 2009;74(4):1150-1156. doi:10.1016/j.ijrobp.2008.09.054
23. Leijte JAP, Kirrander P, Antonini N, Windahl T, Horenblas S. Recurrence patterns of squamous cell carcinoma of the penis: recommendations for follow-up based on a two-centre analysis of 700 patients. Eur Urol.2008;54(1):161-168. doi:10.1016/j.eururo.2008.04.016
24. Ornellas AA, Kinchin EW, Lindenberg Braga Nóbrega B, Wisnescky A, Koifman N, Quirino R. Surgical treatment of invasive squamous cell carcinoma of the penis: Brazilian National Cancer Institute long-term experience. J Surg Oncol.2008;97(6):487-495. doi:10.1002/jso.20980
25. Philippou P, Shabbir M, Malone P, et al. Conservative surgery for squamous cell carcinoma of the penis: resection margins and long-term oncological control. J Urol.2012;188(3):803-808. doi:10.1016/j.juro.2012.05.012
26. Crook JM, Jezioranski J, Grimard L, Esche B, Pond G. Penile brachytherapy: results for 49 patients. Int J Radiat Oncol Biol Phys.2005;62(2):460-467. doi:10.1016/j.ijrobp.2004.10.016
27. Ozsahin M, Jichlinski P, Weber DC, et al. Treatment of penile carcinoma: to cut or not to cut? Int J Radiat Oncol Biol Phys.2006;66(3):674-679. doi:10.1016/j.ijrobp.2006.05.053
28. Crook J, Jezioranski J, Cygler JE. Penile brachytherapy: technical aspects and postimplant issues. Brachytherapy.2010;9(2):151-158. doi:10.1016/j.brachy.2009.05.005
29. Zou ZJ, Liu ZH, Tang LY, et al. Radiocolloid-based dynamic sentinel lymph node biopsy in penile cancer with clinically negative inguinal lymph node: an updated systematic review and meta-analysis. Int Urol Nephrol.2016;48(12):2001-2013. doi:10.1007/s11255-016-1405-x
30.Bermejo C, Busby JE, Spiess PE, Heller L, Pagliaro LC, Pettaway CA. Neoadjuvant chemotherapy followed by aggressive surgical consolidation for metastatic penile squamous cell carcinoma.J Urol.2007;177(4):1335-1338. doi:10.1016/j.juro.2006.11.038
31. Lughezzani G, Catanzaro M, Torelli T, et al. The relationship between characteristics of inguinal lymph nodes and pelvic lymph node involvement in penile squamous cell carcinoma: a single institution experience. J Urol.2014;191(4):977-982. doi:10.1016/j.juro.2013.10.140
32. Hakenberg OW, Compérat EM, Minhas S, Necchi A, Protzel C, Watkin N. EAU guidelines on penile cancer: 2014 update. Eur Urol.2015;67(1):142-150. doi:10.1016/j.eururo.2014.10.017
33. Lucky MA, Rogers B, Parr NJ. Referrals into a dedicated British penile cancer centre and sources of possible delay. Sex Transm Infect.2009;85(7):527-530. doi:10.1136/sti.2009.036061
34. Hussein AM, Benedetto P, Sridhar KS. Chemotherapy with cisplatin and 5-fluorouracil for penile and urethral squamous cell carcinomas. Cancer.1990;65(3):433-438. doi:10.1002/1097-0142(19900201)65:3<433::aid-cncr2820650310>3.0.co;2-g
35. Pizzocaro G, Piva L, Bandieramonte G, Tana S. Up-to-date management of carcinoma of the penis. Eur Urol. 1997;32(1):5-15.
36. Pagliaro LC, Williams DL, Daliani D, et al. Neoadjuvant paclitaxel, ifosfamide, and cisplatin chemotherapy for metastatic penile cancer: a phase II study. J Clin Oncol.2010;28(24):3851-3857. doi:10.1200/JCO.2010.29.5477
37. Robinson R, Marconi L, MacPepple E, et al. Risks and benefits of adjuvant radiotherapy after inguinal lymphadenectomy in node-positive penile cancer: a systematic review by the European Association of Urology Penile Cancer Guidelines Panel. Eur Urol.2018;74(1):76-83. doi:10.1016/j.eururo.2018.04.003
38. Chen M-F, Chen W-C, Wu C-T, Chuang C-K, Ng K-F, Chang JT-C. Contemporary management of penile cancer including surgery and adjuvant radiotherapy: an experience in Taiwan. World J Urol.2004;22(1):60-66. doi:10.1007/s00345-003-0383-7
39. Azizi M, Chipollini J, Peyton CC, Cheriyan SK, Spiess PE. Current controversies and developments on the role of lymphadenectomy for penile cancer. Urol Oncol. 2019;37(3):201-208. doi:10.1016/j.urolonc.2018.08.017
40. Franks KN, Kancherla K, Sethugavalar B, Whelan P, Eardley I, Kiltie AE. Radiotherapy for node positive penile cancer: experience of the Leeds teaching hospitals. J Urol.2011;186(2):524-529. doi:10.1016/j.juro.2011.03.117
41. Crook J. Radiotherapy approaches for locally advanced penile cancer: neoadjuvant and adjuvant. Curr Opin Urol.2017;27(1):62-67. doi:10.1097/MOU.0000000000000346
42. Pagliaro LC, Crook J. Multimodality therapy in penile cancer: when and which treatments? World J Urol. 2009;27(2):221-225. doi:10.1007/s00345-008-0310-z
43. Pond GR, Di Lorenzo G, Necchi A, et al. Prognostic risk stratification derived from individual patient level data for men with advanced penile squamous cell carcinoma receiving first-line systemic therapy. Urol Oncol.2014;32(4):501-508. doi:10.1016/j.urolonc.2013.10.007
44. Theodore C, Skoneczna I, Bodrogi I, et al; EORTC Genito-Urinary Tract Cancer Group. A phase II multicentre study of irinotecan (CPT 11) in combination with cisplatin (CDDP) in metastatic or locally advanced penile carcinoma (EORTC PROTOCOL 30992). Ann Oncol.2008;19(7):1304-1307. doi:10.1093/annonc/mdn149
45. Nicholson S, Hall E, Harland SJ, et al. Phase II trial of docetaxel, cisplatin and 5FU chemotherapy in locally advanced and metastatic penis cancer (CRUK/09/001). Br J Cancer.2013;109(10):2554-2559. doi:10.1038/bjc.2013.620
46. Pickering LM, Tovey H, Elliott T, et al. VinCaP: a phase II trial of vinflunine chemotherapy in locally-advanced and metastatic carcinoma of the penis (CRUK/12/021). J Clin Oncol.2018;36(Suppl 15):abstr 4514. doi: 10.1200/JCO.2018.36.15_suppl.4514
47. Carthon BC, Ng CS, Pettaway CA, Pagliaro LC. Epidermal growth factor receptor-targeted therapy in locally advanced or metastatic squamous cell carcinoma of the penis. BJU Int. 2014;113(6):871-877. doi:10.1111/bju.12450
48. Buonerba C, Pagliuca M, Vitrone FM, et al. Immunotherapy for penile cancer. Future Sci OA. 2017;3(3):FSO195. doi:10.4155/fsoa-2017-0031
49. Hui G, Ghafouri SN, Shen J, Liu S, Drakaki A. Treating penile cancer in the immunotherapy and targeted therapy era. Case Rep Oncol Med.Published online March 25, 2019. doi:10.1155/2019/8349793
50. Chahoud J, Skelton WP IV, Spiess PE, et al. Case report: two cases of chemotherapy refractory metastatic penile squamous cell carcinoma with extreme durable response to pembrolizumab. Front Oncol. Published online December 23, 2020. doi:10.3389/fonc.2020.615298
51. Doran SL, Stevanović S, Adhikary S, et al. T-cell receptor gene therapy for human papillomavirus–associated epithelial cancers: a first-in-human, phase I/II study. J Clin Oncol. 2019;37(30):2759-2768. doi:10.1200/JCO.18.02424
52. Chahoud J, Pickering CR, Pettaway CA. Genetics and penile cancer: recent developments and implications. Curr Opin Urol. 2019;29(4):364-370. doi:10.1097/MOU.0000000000000640
Articles in this issue
over 4 years ago
Clinical Trials in Progress: GOZILAover 4 years ago
Profilin 1 Protein and Its Implications for Cancersover 4 years ago
Questions Linger Around COVID-19’s Originover 4 years ago
The Future of Telehealth for Hematology/Oncology CareNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.