- ONCOLOGY Vol 34 Issue 4
- Volume 34
- Issue 4
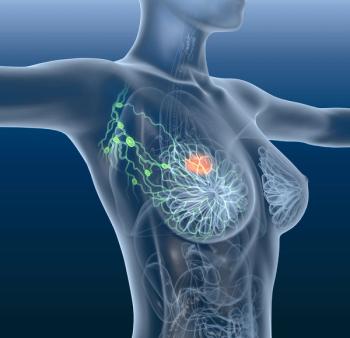
Advancing the Field of Breast Cancer Care
ONCOLOGY® recently sat down with Joyce A. O’Shaughnessy, MD, to discuss the recent trends in breast cancer treatment and the avalanche of agents moving through the development pipeline that have the potential to redefine the accepted standards of care.
With the development of immunotherapy and targeted agents, the treatment landscape for patients with breast cancer has evolved immensely, progressing from one-size-fits-all surgeries to the current state of individualized precision medicine. ONCOLOGY® recently sat down with Joyce A. O’Shaughnessy, MD, to discuss the recent trends in breast cancer treatment and the avalanche of agents moving through the development pipeline that have the potential to redefine the accepted standards of care.
Q: What are the major trends in breast cancer today? Do you think there is an overarching theme that is going to be reflected at the breast cancer conferences this year?
DR O’Shaughnessy: Yes. At all the breast cancer conferences, the novel therapeutics are basically all focused on the molecular drivers of the cancer. For every subtype of breast cancer, there are multiple agents being developed that [target that. So, those are always highlighted because they go hand in hand with…any data on the new agents. Besides that, other things highlighted at the congresses will be advances in immunotherapy for breast cancer. We are kind of new in breast cancer in the immunotherapy space, but we do have exciting data emerging, particularly in the curative setting with triple-negative breast cancer. We also have a new approval in the metastatic setting for triple-negative breast cancer that is programmed cell death protein-ligand 1-positive with atezolizumab (Tecentriq). Everybody is keenly interested in checkpoint inhibitor therapy in the breast cancer space. At all of our congresses, we also highlight locoregional control. There is a trend towards doing less surgery over time, and probably radiation therapy has become a bit more comprehensive for the high-risk patients, but [it is a] shorter course. And even more limited is partial breast irradiation, not whole breast irradiation for lower risk patients. Radiation therapy is becoming personalized. The surgery is becoming personalized. So, we spend a lot of time, because those are very rapidly evolving areas, in locoregional control.
Q: When you talk about “less breast cancer surgery,” are you referring to the trend toward neoadjuvant therapy to see if tumors can be shrunk instead of surgically removed?
DR O’Shaughnessy: Yes, and so [we are] able to do a lumpectomy instead of a mastectomy because [we] shrunk [the tumor] down, but also less axillary surgery which is very important. [We are] taking out fewer axillary lymph nodes and decreasing the risk of lymphedema.
Q: What are some of the more important recent treatment breakthroughs, and which studies in particular are you looking forward to learning about or hearing about this year?
DR O’Shaughnessy: We just recently had the FDA approval [of trastuzumab deruxtecan (Enhertu)], and a lot of these data came out at [the] San Antonio [Breast Cancer Symposium]. All these [results] are so new that it is very important to have our congresses to help bring clinicians up to speed on the data.
We [can also] expect FDA approval very soon of the oral HER2 tyrosine kinase inhibitor, tucatinib, and for metastatic breast cancer, oral neratinib (Nerlynx). We already have neratinib approved in the extended adjuvant setting for patients with HER2-positive breast cancer. Now we are waiting for neratinib to be approved in the metastatic setting. Hope[fully] later this year we will see approval by the FDA [for margetuximab], another agent for HER2-positive breast cancer, a molecularly enhanced form of trastuzumab.
With regard to triple-negative breast cancer, we are looking forward, we hope, to the FDA approval of the antibody-drug conjugate, sacituzumab. We are waiting for that. Then we are really keeping our fingers crossed, crossed, crossed. We will have to see what additional data show, but we are keeping our fingers crossed for the preoperative pembrolizumab (Keytruda) trial [KEYNOTE-522] in triple-negative breast cancer to continue with further follow-up [and demonstrate] improvement in event-free survival. [If so, it] should lead to FDA approval.
The other thing [that] we are waiting for [are data from] some of the adjuvant cyclin-dependent kinase (CDK) 4/6 inhibitor trials…in [patients with] high-risk, estrogen receptor (ER)-positive breast cancer, such as the PENELOPE-B trial which…should [have results] later this year. [In that trial,] patients with ER-positive breast cancer received preoperative [chemotherapy], they still have residual disease at surgery, then they [were given] endocrine therapy, and [finally,] they were randomized to receive 1 year of palbociclib or placebo. [Data] should be [available] soon. [Data are expected from] a couple of other adjuvant CDK4/6 inhibitor trials…within the next year, we hope. That could lead to FDA approvals of CDK4/6 inhibitors in the curative setting, which will be very exciting.
Q: Do you believe that a lot of the recent progress has to do with gaining a better understanding of the molecular mechanisms behind breast cancer?
DR O’Shaughnessy: Yes, and being able to choose the right patient populations. You could have a great agent, but if you do not choose the right patient population, it [will not] have the level of effectiveness it needs [to be granted] FDA approval.
Q: On the community level, is matching treatments and sequencing tumors widespread or is it an area that still requires more education?
DR O’Shaughnessy: We have had a sea change in breast cancer just within the last 6 months with the FDA approval of alpelisib (Piqray). It is the first PI3K alpha-specific inhibitor. [However,] it is for ER-positive breast cancers that have the PIK3CA mutation, and that is about 40% of ER-positive breast cancers. And it is for [patients with] metastatic [disease]. So, you have…to now go looking [for the mutations]. You have…to sequence the breast cancer. You can also get circulating tumor DNA [through] a blood test, because many times you will find the PIK3CA mutation in the blood or in the tumor. For the first time, we have a definite reason for [patients with] ER-positive metastatic [breast cancer] to get next-generation sequencing (NGS).
The FDA approved pembrolizumab for patients with mismatch repair deficient or microsatellite instability-high breast cancers. [That is] only about 2% of breast cancers, but nonetheless, they can do very, very well with this immune-based therapy. Then the FDA approved the neurotrophic tyrosine kinase (NTRK) inhibitors-[larotrectinib (Vitrakvi) and entrectinib (Rozlytrek)]. [They are] for any cancer. It’s a tumor agnostic approval that has an NTRK fusion at the genomic level… a gene fusion. And, again, rare in breast cancer, [approximately] 1%, but if [a patient has] it, you can do NGS to find the NTRK fusion, [the] microsatellite instability, and [the] PIK3CA mutations.
In breast cancer,…we have had a reason to do germline testing, blood [tests] looking for BRCA1 and 2, since the FDA approved the 2 poly (ADP-ribose) polymerase (PARP) inhibitors that we have for patients with germline BRCA1 and 2. So, we have been doing germline genetic testing because in the metastatic setting, we have…2 PARP inhibitors. So, the whole [NGS] thing is really gaining traction in breast cancer.
Q: How many agents do you anticipate being approved in the breast cancer space this year, and perhaps over the next year or 2 as well?
DR O’Shaughnessy: [I]n the metastatic setting, we are expecting sacituzumab, tucatinib, neratinib, and margetuximab this year. And then hopefully preoperative pembrolizumab. That is a little bit aspirational, but the data [to facilitate approval] should be there. The data look good, they just have to hold up. So, I will say pembrolizumab this year. And then next year, I…hope we have another antibody-drug conjugate called SYD985, which is another anti-HER2-based therapy. I am hoping we are going to have adjuvant palbociclib (Ibrance) and adjuvant abemaciclib (Verzenio). Ribociclib (Kisqali) will take another year or 2 thereafter.
Within 2 years, we might have adjuvants. We hope capivasertib, [and the other] Akt inhibitors. [Although it may] be more like 2022…the Akt inhibitor capivasertib by AstraZeneca, and ipatasertib by Genentech Roche, [which] are in active development, [may be available for]…ER-positive breast cancer [and] triple-negative breast cancer.
Hopefully [we will have] some of the oral selective ER degraders in ER-positive [breast cancer]. There is one called elacestrant that is in [a] phase III [trial] right now,…the EMERALD trial, and maybe by [the end of] 2020 we will have [data]. One I really do hope we have next year is the oral taxane, tesetaxel, by a company called Odonate. Now, there were data…at San Antonio [Breast Cancer Conference], and the study was not done in the United States, but it was a very positive trial. It is called OPE. It is oral paclitaxel with encequidar, which basically allows the [taxane] to be absorbed into the bloodstream from the gastrointestinal tract. It is an oral taxane by a company called Athenex. The data looked very good. I hope it will lead to [an] FDA approval. It may be later this year, [or] it could be next year.
An important new area…is with trastuzumab deruxtecan. It was just approved by the FDA for HER2-positive breast cancer. A very, very important…new strategy is [when the] antibody against HER2 [is] hooked up to this powerful chemotherapy drug, deruxtecan. It can bind to breast cancers, particularly ER-positive breast cancers that…have a low level of HER2. So, they are really not HER2-positive, but they [have] some HER2 protein and [the drug is] looking really, really active. It is being compared in phase III trials with [physician’s choice of] chemotherapy and [results could] redefine the subtypes of breast cancer. [With] HER2-positive,…[there is] HER2 amplification, lots of gene copies. But then [there is] this HER2-low, low positive, and that is where…we do not have [agents] right now. So that would be very, very exciting. I suppose that [this strategy] could be with us in 2022. These are my sort of broad estimates based on how quickly I think the studies will accrue [data] and the ones I think are going to be positive.
The other is the atezolizumab, the competitor basically to pembrolizumab. Atezolizumab is already approved for triple-negative [breast cancer] in the metastatic setting. It too is in preoperative studies in triple-negative breast cancer. I hope [it will] be approved [by the FDA for this indication]. We are waiting on the data to be released, but hopefully [it] will be approved in 2021. We also hope that pembrolizumab, will be approved in 2021 for patients with metastatic breast cancer. So, we are waiting for pembrolizumab for both metastatic triple-negative and then most importantly, in the curative setting preoperatively.
Q: I know that patients, obviously, are a big part of what continues to drive your interest in research. But putting it into practice, are there any patient cases that particularly jump out at you or any particular experience that you had with a patient that was really rewarding?
DR O’Shaughnessy: Thankfully a lot of them, because I actually have a strong interest in the area of exceptional responders. These are [patients with] metastatic breast cancer that basically go on to… get cured or they just do well for 5 or more years. Those [patients] are extremely gratifying because they are not expected. [W]hen somebody develops metastatic triple-negative breast cancer, the median lifespan is about 16 months. So, when somebody gets cured, you are standing up, you are doing cartwheels, big-time cartwheels. [Therefore], I have a strong interest in trying to understand the molecular basis for why a particular breast cancer would [be] so responsive, so unexpectedly responsive to…treatment. I have a number of those exceptional responders that are just absolutely fascinating to me, [and it is] extremely gratifying to take care of…patients. I have…a number of stories in that regard.
Q: Is there any one story that you could share?
DR O’Shaughnessy: Because this woman basically has directed a lot of my subsequent research, and she does not mind me using her name. Her first name is Donna. She does not mind because she has…done videos for our fundraising activities around clinical trials to follow up on her success, etcetera. She was diagnosed in 2006 I think, [she] was in her mid-50s, with triple-negative breast cancer, and [she] had [a] lumpectomy,…chemotherapy, and radiation therapy. Her breast cancer recurred in 2008 in her breast. It was node-positive. She had a mastectomy. She had axillary dissection. She had more chemotherapy. She had more radiation therapy.
Between 2008 and 2011 (when I first met her), she had multiple recurrences, locoregionally on the chest wall, in the supraclavicular, infraclavicular lymph node beds, [and in the] subpectoral [lymph node beds]. But it was only [in the] lymph node[s], nowhere else. She kept having multiple surgeries, targeted radiation therapy, and more and more chemotherapy. So, she had had all our major chemotherapy agents for triple-negative breast cancer, including taxanes and carboplatin, etcetera. But the disease just kept recurring. It was not very fast, but it kept recurring.
I met her in 2011 when she came over from UT Southwestern for a clinical trial that we had, and she had [the disease in] a left supraclavicular lymph node. It was about 3 cm in size and that was the only disease she had. So, we biopsied it. We did next-gen[eration] sequencing, and we did not find any particular mutation to go after except that she [had] a FOXM1 amplicon, and…somatic loss of function mutations in SMARCA4 (which among other things…is part of the SWI/SNF family of proteins that are very involved in DNA repair, double-strand DNA repair).
She happened to go on to a clinical trial, a single-agent trial of an agent called BEZ235 (dactolisib) which is a PI3K inhibitor, a target of rapamycin complex (TORC) 1, TORC2 inhibitor, and it also inhibits DNA repair. So, her cancer…respond[ed] to that. Her left supraclavicular lymph node went from 3 cm down to 1.5 cm, but, [it] was a short-lived response. After about 6 weeks on therapy, she responded and then the left supraclavicular lymph node started growing very, very quickly which is unusual because it had been pretty slow. So that was resected.
A few months later, she came in again and a computed tomography scan showed some pectoral lymph node [growth] but that was all she had. Again, that was resected. All she had was [a] resection. When she recovered from that surgery, [the] subpectoral lymph node, she came [back] in January 2012. She had very, very rapidly growing internal mammary lymph nodes and some of it was substernal underneath the sternum. It was growing [so] fast that it was bowing out her sternum. It was not eroding. The cancer was not eroding through her sternum, but it was pushing the sternum out. The sternum is flat. It was being bowed out [because the tumor] was growing so fast, and she was in pain. So, big, big nodal disease. And so very fast. I treated her with [high-dose] nab-paclitaxel (Abraxane) and cisplatin every 3 weeks. She [received] 6 cycles. She was in a complete response after 2 cycles and…is cured. Her disease never came back.
And so, I have tissue all along the way, all the biopsies. She had biopsies. She had multiple surgeries. I have done a lot of analysis of the molecular characteristics and also the reverse phase protein array…which is the protein expression…the activation of proteins in her breast cancer. I really think that…the BEZ235 remodeled her cancer. It got rid of the signaling through the PI3K pathway. It inhibited DNA-dependent protein kinase, and it basically [made] her cancer shift over to a highly proliferative mitogen-activated protein kinase, mitogen-activated protein kinase kinase/extracellular signal-regulated kinase-driven breast cancer. It reexposed the homologous recombination deficiency in her breast cancer which we think [was] there because [of] the SMARCA4 loss of function deletion.
So, it made her cancer much more sensitive to chemotherapy, DNA-damaging chemotherapy, such as the cisplatin. Also, [it was] so fast growing that the nab-paclitaxel stopped [the] fast growing cancer cells, too. It made her cancer exquisitely sensitive to chemotherapy even though she never benefitted from chemotherapy before. I think the BEZ235 changed the nature of that cancer and made it much more chemotherapy sensitive, more BRCA like. These kinds of trials are called priming the breast cancer, priming it to make it more…BRCA like, basically. So, that shifted the direction of my pilot trial, my translational research that I do on my own, doing…biopsies and such, trying to recapitulate, try[ing] to repeat that in other patients.
Q: That is a remarkable case.
DR O’Shaughnessy: Oh yeah.
Q: What should receive more emphasis in the discussion and clinical attention among oncologists today in your field? What should be emphasized more overall?
DR O’Shaughnessy: Well, so where we really need help is with insurance coverage or national guidelines and insurance coverage for our patients who are obese or who are obese at diagnosis or who become obese during their breast cancer journey. Many of our therapies slow patients’ metabolic rates because it puts them into a deeper menopause, [the] antiestrogen therapies. Some of the therapies make patients fatigued and so they are less active. But many of our [patients with] ER-positive [breast cancer] on…aromatase inhibitors…gain weight. A…weight gain [of 10% or more] in women with ER-positive breast cancers increases the risk of breast cancer recurrence. And [if a patient has] node-positive disease, [it] can happen 20 years later. We know [that] our obese patients, in general, not 100%,…have less favorable outcomes, [poorer] outcomes with our therapies.
We know from studies like…WINS…(Women’s Intervention Nutrition Study) by Rowan Chlebowski [et al],…that in ER-negative breast cancer,…a low-fat diet, which was associated with a modest weight loss, 5% weight loss, made a big difference in decreasing the risk of recurrence. We do not know whether it was the low-fat diet, or…the weight loss, but we are pretty desperate for structured approaches. [We need] structured approaches that will be supported by insurance for weight loss and to increase the fitness of our patients with exercise. That is the big, big thing we are lacking.
Q: Can you expand on what you mean by structured programs?
DR O’Shaughnessy: By structure, I mean things that women are expected to show up to, like [a] meeting with the nutritional counselor or weekly meetings in groups to support each other through weight loss. [Other examples include]…programs that might pay for parking,…gas,…[or] the instructor, [and] exercise programs that are covered. Or, paying for [a] YMCA membership, covering the classes and then having classes for survivors, etcetera, but real structure. A lot of it [centers] around community, having a community to walk this journey with. But you cannot [just] tell people to diet and eat healthy and exercise. It does not help people.
Q: Is there anything else that you wanted to discuss?
DR O’Shaughnessy: I always like to plug my School of Breast Oncology®. It’s a 3-day, deep dive breast cancer boot camp. Soup to nuts, all the important literature in breast cancer but [it is] very practical. It is all case-based discussion for the surgical oncologist, medical oncologist, [and] radiation oncologist to come and really get a very in-depth update on all of the key data around [the] management strategies for breast cancer, including breast cancer prevention, genetic germline evaluation, [etcetera]. What are the data [surrounding] diet and exercise? What about breast cancer in pregnancy? What about toxicity management? [All questions with a] big emphasis on radiation and surgical issues. So, a big, multidisciplinary course.
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
Articles in this issue
almost 6 years ago
Oncology in the Time of COVID-19almost 6 years ago
FDA Approves Nivolumab Plus Ipilimumab for the Treatment of Advanced HCCNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.