Oncology NEWS International
- Oncology NEWS International Vol 7 No 2
- Volume 7
- Issue 2
Cancer Groups Protest New Medicare Policy on Epoetin
ATLANTA-A local effort by a state Medicare director to restrict Medicare reimbursement for use of epoetin-alpha (recombinant erythropoietin, Epogen, Procrit) in chemotherapy-induced anemia has now become nationwide policy, even though it contradicts current practice, LaMar S. McGinnis, MD, of the American Cancer Society, told Oncology News International in an interview.
ATLANTAA local effort by a state Medicare director to restrict Medicare reimbursement for use of epoetin-alpha (recombinant erythropoietin, Epogen, Procrit) in chemotherapy-induced anemia has now become nationwide policy, even though it contradicts current practice, LaMar S. McGinnis, MD, of the American Cancer Society, told Oncology News International in an interview.
The revised policy allows Medicare reimbursement for epoetin-alpha in patients receiving aggressive chemotherapy only if the patient has a hemoglobin of less than 8 g/dL and a hematocrit of less than 25%, with symptoms of anemia documented before initiating treatment.
The American Cancer Society is particularly concerned about this ruling because, Dr. McGinnis said, it seems an intrusion into medical practice.
The ruling affects the quality of cancer care and the rights of physicians to make clinical decisions based on individual need, he said. It flies in the face of what everybody is trying to do now, that is, to decrease the use of blood transfusions.
Dr. McGinnis was critical not only of the content of the new policy but also of the process by which it was developed. The policy was developed by the Medicare Carrier Director of Mississippi, with input from a state advisory committee, and was issued by the Health Care Finance Administration (HCFA) as a Medicare Part B Model Local Medical Review Policy. Dr. McGinnis contends that the new policy was made without a proper review of the scientific literature or adequate input from medical oncologists nationwide.
Based on discussions with colleagues in Mississippi, he said that the new rule was universally opposed by the medical oncology community in that state.
Opposed to Mandates
Dr. McGinnis called the adoption of the policy a diversion from what we had hoped would be an appropriate evolution of Medicare recommendations based on guidelines developed by responsible organizations. Rather, he said, this provision came down as a mandate, and we are opposed to mandates.
The ACS is working through its Washington office, where Susan Polan, PhD, is director of government relations, to draw attention to the issue.
Also, last December, Harmon Eyre, MD, the ACSs executive vice president for Research & Cancer Control, wrote a letter about the ruling to Grant Bagley, MD, director of the Coverage and Analysis Group of HCFAs Office of Clinical Standards and Quality. In the letter, he outlined the Societys objections to the new reimbursement policy and the way it was developed.
The ACS is not alone in this effort, Dr. McGinnis said, noting that ASCO has also petitioned Dr. Bagley to change the ruling and the process by which it arose. The ACS has not yet received a reply to Dr. Eyres letter, he added.
In his letter to Dr. Bagley, Dr. Eyre said that erythropoietin, though needed infrequently, offers significant benefit with no significant side effects for patients suffering anemia from aggressive chemotherapy, and explained that the decision to use erythropoietin in these patients depends upon a variety of factors, not hemoglobin level alone.
He noted in the letter that two organizations, the American Society of Clinical Oncology (ASCO) and the American Society of Hematology (ASH), together will undertake a critical review in 1998 of all available scientific data to develop appropriate guidelines for the use of hematinics. Until the ASCO/ASH or other authoritative review has been completed, there should be no mandate to change Medicare Part B coverage guidelines.
Dr. Eyre concluded the letter by urging that the new policy be voided and that, in future, Medicare coverage policies be based on an open process involving expert national organizations, current clinical guidelines and practice, and peer-reviewed scientific literature.
Articles in this issue
about 28 years ago
Tobacco Companies Reach Settlement With Texas for $15.3 Billionabout 28 years ago
Archives to Collect Info on Radiation Exposure Worldwideabout 28 years ago
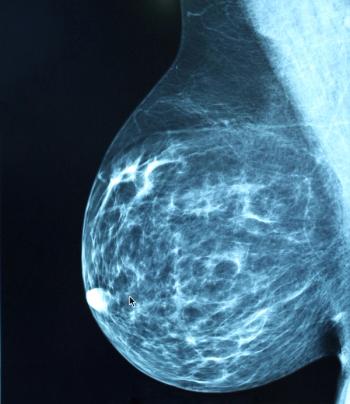
Few BRCA-1 Carriers Take Recommended Precautionsabout 28 years ago
Lifelong Weight Control a Key to Breast Ca Preventionabout 28 years ago
Eight-Year Prostate Brachytherapy Update Shows Good Resultsabout 28 years ago
Patient Brochure on Breast Cancer Tumor Markersabout 28 years ago
Gay Men’s Health Crisis Calls for HIV Reporting in New Yorkabout 28 years ago
Single-Agent Taxanes in Advanced Breast Cancer: A Commentaryabout 28 years ago
ODAC Declines to Vote on DepoCyt FDA Recommendationabout 28 years ago
Photofrin Approved for Early-Stage Lung CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.