- ONCOLOGY Vol 19 No 9
- Volume 19
- Issue 9
Commentary (Brown)-Mohs Micrographic Surgery: Established Uses and Emerging Trends
Drs. Pennington and Leffellhave provided an excellentoverview of the current uses ofMohs micrographic surgery. The procedurehas certainly come a long waysince the days of Frederic Mohs andthe application of zinc chloride paste(chemosurgery). Despite the fact that ithas indeed become the “gold standard”for the removal of basal cell carcinoma(BCC) and squamous cell carcinoma(SCC), there remain areas of controversyfor its use in melanoma and otherless common cutaneous neoplasms. Asmore dermatologists (and even a fewnondermatologists) have becometrained and gain experience in this specializedprocedure, and as more communitiesand university teaching centershave established growing Mohs practices,the procedure has become recognizedand embraced by health-careprofessionals and patients alike.
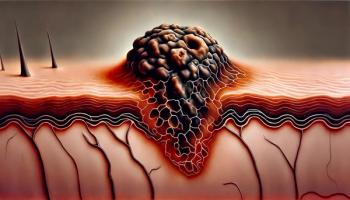
Drs. Pennington and Leffell have provided an excellent overview of the current uses of Mohs micrographic surgery. The procedure has certainly come a long way since the days of Frederic Mohs and the application of zinc chloride paste (chemosurgery). Despite the fact that it has indeed become the "gold standard" for the removal of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), there remain areas of controversy for its use in melanoma and other less common cutaneous neoplasms. As more dermatologists (and even a few nondermatologists) have become trained and gain experience in this specialized procedure, and as more communities and university teaching centers have established growing Mohs practices, the procedure has become recognized and embraced by health-care professionals and patients alike. Treatment Options
Dermatologists have several excellent methods for treating common skin cancers, including both surgical and nonsurgical techniques. The nonsurgical approaches include topical treatment such as imiquimod (Aldara) and fluorouracil for superficial BCCs, photodynamic therapy, cryosurgery, and radiation. Surgical approaches include curettage, excision with permanent sections, and excision with frozen sections. There is no "best" treatment, and all available procedures have distinct advantages and disadvantages. For example, curettage is quick, easy to learn, requires minimal equipment, and is associated with a cure rate of 90% or better for select low-risk skin cancers. With this strategy, however, there is no margin control, and healing and cosmesis can be variable; moreover, it is not a very effective treatment for high-risk tumors. The pluses and minuses of all procedures should be discussed with the patient so that an informed decision can be made. Most skin cancers do not require Mohs surgery, and there are clear indications and guidelines for its use. I will strongly disagree with any Mohs surgeon who states that all BCCs and SCCs should be treated with Mohs surgery simply because Mohs has the highest cure rate; that may be true, but it does not justify the overuse (and potential abuse) of the Mohs procedure. Risk Criteria
Which brings us to the concept of low-risk and high-risk skin cancers. Mohs surgery is typically utilized for high-risk BCC, and guidelines have been established over the years. A highrisk BCC includes recurrent tumor, incomplete excision (positive margin on standard excision), location in the "mask" of the face (forehead, periocular, perinasal, perioral, periauricular), aggressive histologic growth pattern (morpheaform, basosquamous, infiltrative, micronodular), perineural invasion, and larger size (> 6 mm on the central face, > 1 cm on the head and neck, > 2 cm on the trunk and extremities). Squamous cell carcinomas are potentially more aggressive than BCCs, with a small but very real risk for metastatic spread. With the exception of in situ disease (Bowen's), most SCCs should be excised with margin control, including Mohs surgery. Although the overall cure rate for SCC utilizing Mohs is not as high as it is for BCC, the technique is nevertheless superior to standard excision, again due to meticulous mapping and frozen-section control. Advantages of Mohs Surgery
So with all the modalities available, why Mohs? Clearly there are advantages, including: (1) High success rate-The literature certainly supports the fact that Mohs micrographic surgery has the highest cure rates compared to other available procedures.
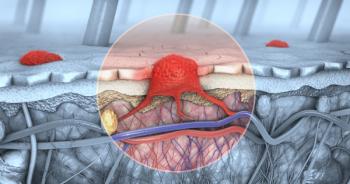
(2) Potential for tissue conservation because smaller margins can be taken- This is feasible because, within an hour, frozen sections can be examined and more tissue taken if needed. Basically, it removes some of the guesswork of taking an arbitrary margin of 4 to 6 mm. This is extremely helpful when trying to save an eyelid, alar rim, or lip. It can also mean the difference between a simple primary closure and a more complex flap or graft. Some persons are under the misconception that Mohs surgery makes "big holes." Partly, Mohs surgeons are to blame for this misconception, because when lecturing, we often show defects out of proportion to the clinical tumor in order to point out how aggressive the subclinical spread of BCC can be. At the same time, however, the point should be made that very often tumor clearance is achieved with the first stage and there is minimal tissue loss and therefore smaller defects than what might have been expected..
(3) The surgeon can feel confident that clear margins have been achieved, and therefore immediate reconstruction, even complex flaps, can be undertaken. Performing an extensive flap procedure without established clear margins is risky and makes subsequent tumor extirpation very difficult.
(4) The procedure is well tolerated in an outpatient setting. It is a rare case that needs to go to the operating room. Because the procedure is performed under local anesthesia, it is safe even for elderly patients with multiple medical problems. Disadvantages of Mohs Surgery
Are there disadvantages to Mohs surgery? Indeed. First, the cure rate is not 100%. Despite the meticulous mapping and compulsive examination of all tissue margins, recurrences still occur; the strategy is not perfect. Second, the procedure takes longer. Patients need to wait for the frozen sections and the average two-stage procedure and subsequent reconstruction may require half a day in the office. (That said, few patients ever find this difficult.) Third, Mohs is more expensive than standard treatments but less expensive than if the patient were to be taken to an ambulatory surgery center. Fourth, a Mohs surgeon is only as good as the technician and lab. The preparation of high-quality frozen sections is a skilled procedure that takes months to learn well. Horizontal sectioning with a full epidermal margin and complete deep-tissue visualization is a technical challenge. Lousy slides make for a suboptimal Mohs procedure. Also, no matter how excellent the frozen sections, permanent sections are usually better. For this reason, when dealing with a highly aggressive or unusual tumor (eg, a deeply invasive, poorly differentiated SCC), a final permanent section is sometimes sent for histologic confirmation. Other Considerations and Controversies
What makes Mohs surgery unique? Is it not simply an excision with frozen sections? As pointed out, the horizontal sectioning is truly different from standard vertical sectioning with 100% of excised tissue examined. The mapping technique is detailed and meticulous, so exact tumor location can be identified. However, the most unique aspect of the Mohs procedure is the fact that the physician serves as both the surgeon and the pathologist. The doctor excises, maps, and reads the slides. There is no misunderstanding as to where the residual tumor is located. Mohs surgery is primarily used for BCC and SCC. Its use in melanoma is controversial and the subject of an ongoing debate. Although there are established articles showing the success of Mohs for melanoma, it is far from being embraced as a standard of care by Mohs surgeons. There are many Mohs surgeons, myself included, who do not believe frozen sections are reliable enough to track out melanomas. Most melanomas that are not limited to the head and neck area can be easily excised with standard wide local excision margins. The challenge is for melanomas on the face, usually of the lentigo maligna type. These are ill-defined, often large, and in important cosmetic areas. Many surgeons will use a "modified" Mohs technique involving the same detailed peripheral mapping but with rapid-turnaround permanent sections (usually within 24 hours). These permanent sections are typically interpreted by a dermatopathologist. At the University of Rochester, we have used this modified technique for the past 10 years with a high cure rate (98%). The disadvantage is that only one stage can be performed per day. Certainly, there is more work involved for both the physician and the patient. There may be Mohs surgeons whose labs can produce very thin, artifact-free frozen sections, but I dare say that this is the exception and not the rule. As to other unusual cutaneous tumors, Mohs has been described for almost every rare skin cancer as long as the tumor is contiguous, not multifocal, and can be easily visualized on frozen sections. The biggest challenge in determining the overall success rate of Mohs for these cancers is that the number of cases is usually small, and the studies are usually retrospective in nature and not well-controlled. Certainly, the cure rates for these challenging, unusual cutaneous tumors will not be as high as they are for BCCs, but nonetheless are usually excellent when compared to standard wide local excisions. Again, the idea is that of meticulous mapping to try to look at the entire specimen that has been excised. It is very important that the Mohs surgeon removing these unusual tumors has appropriate experience and training. Often, expert dermatopathology back-up will be needed and I do not hesitate sending final sections for permanents to confirm negative margins. Conclusions
Mohs has become a highly appreciated surgical modality for the treatment of cutaneous neoplasms, especially BCCs and SCCs. Its role in other cancers, including melanoma, will likely continue to stir debate. Mohs surgery is indicated for select, high-risk tumors, and caution must be taken not to overutilize the procedure for all skin cancers. It is best (but not solely) performed by fellowship-trained dermatologists with full and active cutaneous oncology practices.
Disclosures:
Dr. Brown is a speaker and consultant for 3M.
Articles in this issue
over 20 years ago
Biphasic Tumors of the Female Genital Tractover 20 years ago
Commentary (Czito/Willett): Neoadjuvant Therapy for Gastric Cancerover 20 years ago
Mohs Micrographic Surgery: Established Uses and Emerging Trendsover 20 years ago
Metastatic Colorectal Cancer: Is There One Standard Approach?over 20 years ago
Cancer Management in Patients With End-Stage Renal Diseaseover 20 years ago
Commentary (Goldberg/O'Neil): Neoadjuvant Therapy for Gastric CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.