- ONCOLOGY Vol 10 No 7
- Volume 10
- Issue 7
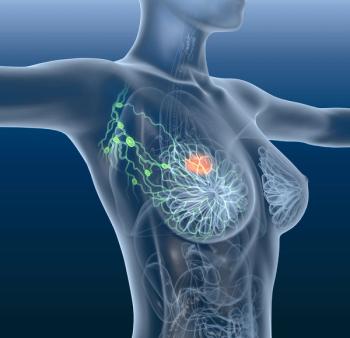
Defining the Role of Post-Mastectomy Radiotherapy: The New Evidence
It is ironic that the issue of aggressive local therapy for breast cancer has re-emerged as a controversial issue in the early 1990s, almost 100 years after Halsted proposed this theory in the early 1890s [1]. Since that time, both survival and quality of life seemed to have improved for patients with breast cancer, due to more sophisticated and effective treatments. Nonetheless, as Drs. Pierce and Lichter point out in their article, the precise balance between the benefits and risks of aggressive local therapy still remains to be defined.
It is ironic that the issue of aggressive local therapy for breastcancer has re-emerged as a controversial issue in the early 1990s,almost 100 years after Halsted proposed this theory in the early1890s [1]. Since that time, both survival and quality of lifeseemed to have improved for patients with breast cancer, due tomore sophisticated and effective treatments. Nonetheless, as Drs.Pierce and Lichter point out in their article, the precise balancebetween the benefits and risks of aggressive local therapy stillremains to be defined.
Does More Aggressive Local Therapy Make a Difference?
The resolution of this issue initially lies in the definitionof "benefit." As Pierce and Lichter discuss, one mustseparate issues of local vs systemic recurrence. Most investigatorsagree that more intense local therapy results in a decreased riskof local recurrence when compared to less intense local therapy.
However, is a reduction in local recurrence, by itself, an acceptableindication for prophylactic therapy? There are at leastthree potential reasons for routinely treating all patients withprophylactic local therapy:
1) to avoid the emotional distress of a local recurrence;
2) to avoid uncontrollable symptomatic local disease (so-calledlocal "shambles"); and/or
3) to reduce the chances of future mortality.
Unfortunately, it has not been established that prevention oflocal recurrence reduces any of these end points. Few, if any,studies have specifically addressed the issue of quality of lifeand patient perceptions in groups of women who have or have notreceived prophylactic chest wall radiotherapy after mastectomy.Likewise, results from a few retrospective series and only a singleprospective study suggest that the use of prophylactic radiationtherapy decreases the incidence of "uncontrolled" localdisease [2].
Such data are very difficult to glean from most clinical studies.Rather, most authors report on only the incidence of any localrecurrences (controllable or not) that occur before theonset of systemic disease. Local recurrences that develop subsequentto distant metastases are often ignored, and whether or not theycan be adequately controlled is often not stated. Thus, the incidenceof absolute control during a patient's lifetime is usually notreported accurately [3].
Pierce and Lichter argue appropriately that systemic recurrenceand survival may be more meaningful end points for assessing theeffects of local therapy. Does any local therapy reduce mortality?The answer to this question is, of course, yes. Between 60% to80% of all patients with primary breast cancer can be cured withlocal therapy alone. Furthermore, results from the randomizedstudies of mammography screening indicate that early detectionand local treatment improve survival relative to delayed localtreatment.
Does More Aggressive Local Therapy Reduce the Risk of DistantMetastasis?
If we conclude that local therapy alone cures a substantial fractionof patients and that early local therapy improves survival relativeto delayed local treatment, we might reasonably infer that improvementsin local therapy may make a difference in overall survival. Pierceand Lichter provide an elegant review of the current data on whethermore aggressive local therapy (in this case, post-mastectomy radiotherapy)improves overall survival while decreasing local recurrence. Theymake the cogent point that the earliest trials focusing on thisissue consistently demonstrated a decrease in local recurrencebut failed to show any evidence of an improvement in overall survival.
It has been argued that these early studies were performed inan era of out-dated radiotherapy techniques and in the absenceof effective systemic therapy. Results from more modern studies,especially those conducted by the Danish Breast Cancer CooperativeGroup and the Vancouver Group, suggest that the issue of post-mastectomyradiotherapy needs to be readdressed [4,5]. We applaud the suggestionby Pierce and Lichter that a new randomized trial should be consideredin the United States. It is less certain whether we should nowrecommend the routine delivery of post-mastectomy radiotherapyto patients at high risk of local recurrence.
What Are the Risks and Costs of Radiation Therapy?
With currently available techniques, post-mastectomy radiationtherapy appears to pose a substantially lower risks than wereobserved with the techniques used in the 1940s and '50s [6,7].Nonetheless, these risks still include pulmonary, cardiac, andneuromuscular damage and the potential for a second malignancy.None of these appears to occur in more than 5% of all patients[6,7].
Of these complications, perhaps the most feared is late cardiacdysfunction. The precise risk of this complication is not established.Studies from our center and elsewhere have suggested the possibilityof enhanced subacute cardiac damage in patients treated with highcumulative doses of adjuvant doxorubicin and left-sided irradiation[8]. However, we have reviewed our experience with patients whoreceived doxorubicin at cumulative doses of less than 200 mg/m²in a recently reported randomized trial, and we have seen no increasein subacute mortality, regardless of the side treated [9]. Furthermore,a comparison of patients who received chest-wall radiation therapyto either the right or left side at the Joint Center for RadiationTherapy suggested no difference in non-breast cancer mortalityin patients who did not receive chemotherapy [10].
Post-mastectomy radiation therapy results in a substantial increasein the cost of care, both in terms of direct and indirect expenses.A course of chest wall radiotherapy requires approximately 4 to6 weeks of daily treatment and, on average, costs between $10,000and $15,000. Furthermore, it results in lost time from work, increasedtransportation costs, and, possibly, additional elder- and child-carecosts. Thus, recommendations for routine post-mastectomy chestwall radiation therapy require a careful assessment of both localand systemic benefits and results. Such an analysis is best performedin the context of a randomized clinical trial.
Do Biologic Changes Lead to Local Recurrence?
The issue of prevention of local recurrence raises several interestingbiologic questions. Why is the chest wall, especially the mastectomyscar, the most frequent site of breast cancer recurrence? Localrecurrence may simply be secondary to insufficient surgical resectionand/or surgical contamination of fields during the resection itself.Alternatively, microenvironmental changes in the area of a healingscar, such as local production of various growth factors and othercytokines, may induce anchorage and growth of hematologic metastases[11].
Insufficient data exist to fully resolve any of these theories.However, new trials of chest wall therapy will provide an excellentopportunity to incorporate correlative studies on the biologyof local recurrence.
Summary
In summary, the issue of more aggressive local therapy for patientswith newly diagnosed primary cancers remains controversial. Theauthors are to be praised for their recommendation that a prospectiverandomized trial be mounted to address this issue. We stronglysupport this recommendation.
References:
1. Halsted WS: The results of operations for the cure of cancerof the breast performed at the Johns Hopkins Hospital from June,1889, to January, 1894. Johns Hopkins Hosp Rep 4:297-350,1894-1895.
2. Rutqvist L: Adjuvant radiation therapy versus surgery alonein operable breast cancer: Long-term follow-up of a randomizedclinical trial. Radiother Oncol 26:104-110, 1993.
3. Gelman R, Gelber R, Henderson IC, et al: Improved methodologyfor analyzing local and distant recurrence. J Clin Oncol8:548-555, 1990.
4. Overgaard M, Christensen J, Johansen H, et al: Evaluation ofradiotherapy in high-risk breast cancer patients: Report fromthe Danish Breast Cancer Cooperative Group (DBCG 82) trial. IntJ Radiat Oncol Biol Phys 19:1121-1124, 1990.
5. Ragaz J, Jackson S, Le N, et al: Can adjuvant locoregionalradiotherapy (XRT) reduce systemic recurrences in stage 1-11 breastcancer patients? Recurrence analysis of the British Columbia randomizedtrial. Proc Am Soc Clin Oncol 15:121, 1996.
6. Lingos TI, Recht A, Vicini F, et al: Radiation pneumonitisin breast cancer patients treated with conservative surgery andradiation therapy. Int J Radiat Oncol Biol Phys 21:355-360,1991.
7. Pierce SM, Recht A, Lingos TI: Long-term radiation complicationsfollowing conservative surgery (CS) and radiation therapy (RT)in patients with early stage breast cancer. Int J Radiat OncolBiol Phys 23:915-923, 1992.
8. Harrigan P, Otis D, Recht A, et al: The effect of adjuvantradiation therapy on cardiac events in breast cancer patientstreated with doxorubicin. Proc Am Soc Clin Oncol 14:102a,1995.
9. Harrigan P, Recht A, Payne S, et al: Treatment-related cardiactoxicity from doxorubicin (DOX) and radiation therapy (RT) inpatients treated with breast-conserving therapy. Proc ASTRO(in press).
10. Nixon A, Gelman R, Bornstein B, et al: Non-breast cancer mortalityafter conservative surgery and radiation therapy (RT) to the leftbreast. Proc ASTRO (in press).
11. Fisher B, Saffer E, Rudock C, et al: Effect of local or systemictreatment prior to primary tumor removal on the production andresponse to a serum growth-stimulating factor in mice. CancerRes 49:2002-2004, 1989.
Articles in this issue
over 29 years ago
The Role of PSA in the Radiotherapy of Prostate Cancerover 29 years ago
The Role of PSA in the Radiotherapy of Prostate Cancerover 29 years ago
The Role of PSA in the Radiotherapy of Prostate Cancerover 29 years ago
State of the Art in Umbilical Cord Transplantationover 29 years ago
Viatical Bill of Rightsover 29 years ago
Hospice and Palliative Care: Program Needs and Academic Issuesover 29 years ago
Long-Term Consequences of the Breast Implant DebateNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.