
FDA Approves Cilta-Cel for Relapsed/Refractory Multiple Myeloma
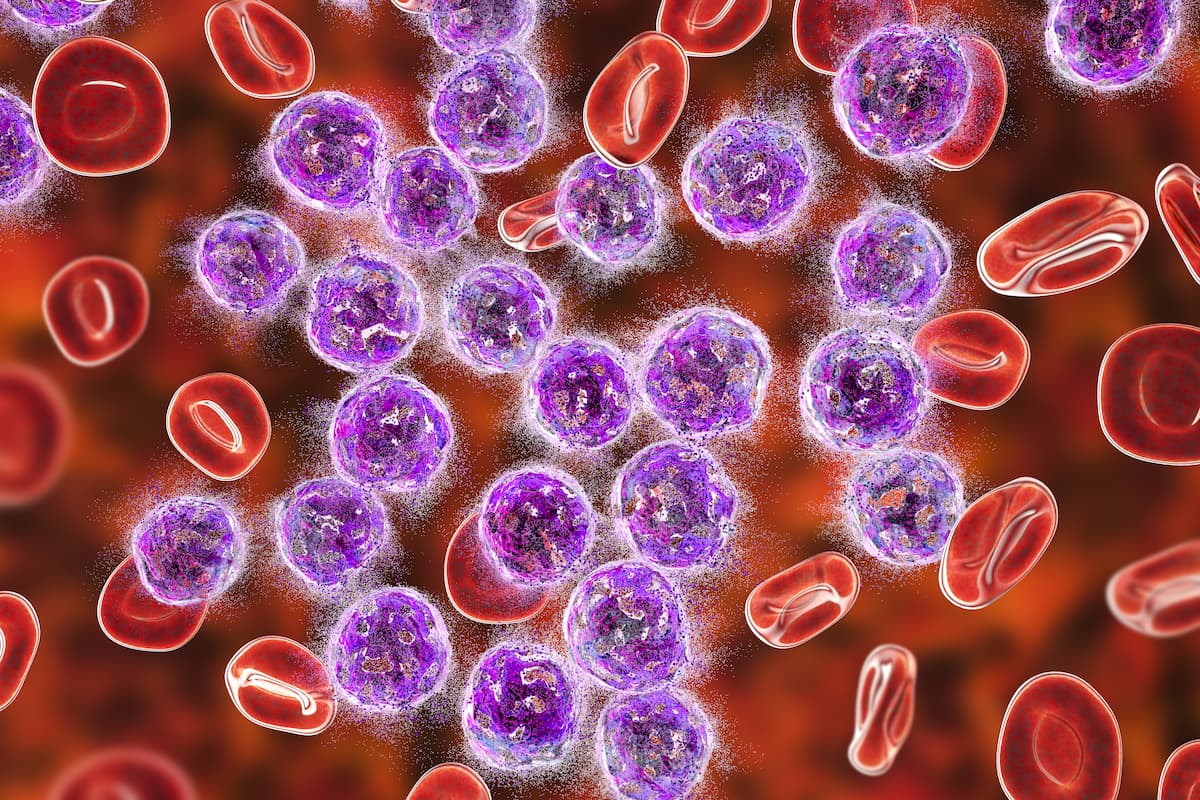
Patients with heavily pretreated relapsed/refractory multiple myeloma may now receive treatment with ciltacabtagene autoleucel following its approval by the FDA.
The FDA has approved the use of ciltacabtagene autoleucel (Carvykti; cilta-cel) for the treatment of patients with relapsed/refractory multiple myeloma after 4 or more lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody, according to press release from The Janssen Pharmaceutical Companies of Johnson & Johnson.1
The approval was based on findings from the phase 1b/2 CARTITUDE-1 trial (NCT03548207) during which one-time treatment with cilta-cel resulted in an overall response rate of 98% (95% CI, 92.7%-99.7%). Additionally, investigators reported a stringent complete response rate of 78% (95% CI, 68.8%-86.1%). The median duration of response was 21.8 months after a median follow-up of 18 months.
“We are committed to harnessing our science, deep disease understanding and capabilities to bring forward cell therapies like CARVYKTI as we continue to focus on our ultimate goal of delivering a cure for multiple myeloma,” Peter Lebowitz, MD, PhD, global therapeutic area head, of oncology at Janssen Research & Development, LLC. “We extend our sincere gratitude to the patients, their families and the teams of researchers and study centers who have participated in the clinical study of CARVYKTI and enabled today's approval.”
Updated results were previously presented at the
BCMA-positive patients who were treated with CAR T-cell therapy experienced an overall response rate of 97.9% with a stringent complete response (sCR) rate of 80.4% and a very good partial response of 14.4%. The median time to first response was 1 month, and the median time to best response and CR or greater was 2.6 months. Moreover, the median duration of response was 21.8 months. Investigators estimated that 73% of responders had not progressed or died at 12 months.
A total of 61 patients were minimal residual disease (MRD) evaluable, 91.8% of whom were MRD negative, with a median time to MRD 10-5 negativity of 1 month. Investigators also reported that 57.7% of those in the overall patient population were MRD negative. Additionally, the overall patient population had an 18-month progression-free survival (PFS) rate of 66.0% (95% CI, 54.9%-75.0%), and those who achieved a sCR had an 18-month PFS rate of 75.9% (95% CI, 63.6%-84.5%). The 18-month overall survival rate was 80.9% (95% CI, 71.4%-87.6%).
Investigators did not observe any new safety signals with this follow-up. The most common grade 3/4 hematologic adverse effects (AEs) that occurred in 25% or more of patients included neutropenia (94.8%), anemia (68.0), thrombocytopenia (59.8%), and leukopenia (60.8%). The most common grade 3/4 nonhematologic AEs included hypophosphatemia (7.2%) and hypocalcemia (3.1%), with other AEs including fatigue (5.2%) and aspartate aminotransferase increase (5.2%).
Within the overall patient population, 94.8% (n = 92) of patients experienced cytokine release syndrome (CRS), with the time to median onset of 7 days and a median duration of 4 days. The majority of cases were grade 1/2, and 98.9% of patients had their CRS resolve within 14 days of onset.
“Cilta-cel has a manageable safety profile consistent with its mechanism of action; no new safety signals were observed with longer follow-up,” the investigators concluded.
References
- U.S. FDA Approves CARVYKTI (ciltacabtagene autoleucel), Janssen's first cell therapy, a BCMA-directed CAR-T immunotherapy for the treatment of patients with relapsed or refractory multiple myeloma. News release. Janssen. February 28, 2022. Accessed February 28, 2022. https://prn.to/3vskiZu
- Martin T, Usmani S, Berdeja J, et al. Updated Results from CARTITUDE-1: Phase 1b/2 study of ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T cell therapy, in patients with relapsed/refractory multiple myeloma. Blood. 2021; 138(suppl_1): 549. doi:10.1182/blood-2021-146060
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.





































