FDA Approves Iobenguane I 131 for Rare Adrenal Gland Tumors
Intravenous Iobenguane I 131 has been approved to treat unresectable, locally advanced, or metastatic pheochromocytoma.
Oncologists now have a new treatment to offer patients with unresectable rare adrenal tumors. On July 30, the US Food and Drug Administration (FDA) approved iobenguane I 131 (Azedra) 555 MBq/mL intravenous injection for the treatment of unresectable, locally advanced, or metastatic pheochromocytoma or paraganglioma in adults and adolescents age 12 years and older.
Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research in Bethesda, Maryland, said many patients with these types of ultra-rare cancers can be treated with surgery or local therapies. However, there are no effective systemic treatments for patients who experience tumor-related symptoms.
“Patients will now have an approved therapy that has been shown to decrease the need for blood pressure medication and reduce tumor size in some patients,” Pazdur said in a
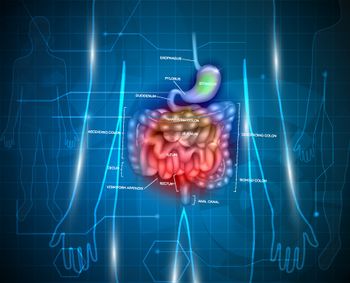
Pheochromocytomas are rare tumors of the adrenal glands. When these tumors occur outside the adrenal gland they are called paragangliomas. Patients with metastatic pheochromocytoma and paraganglioma have a poor prognosis, with an estimated 5-year survival rate of approximately 12%.
The FDA approval of iobenguane I 131 was based on data from a pivotal phase II, open-label, multicenter trial that was conducted under a Special Protocol Assessment (SPA) with the FDA. The final results showed that 17 of 68 evaluable patients (25%) experienced a 50% or greater reduction of all antihypertensive medication for at least 6 months, achieving the primary endpoint specified in the SPA.
The study showed favorable results from a key secondary endpoint evaluating the proportion of patients with overall tumor response as measured by Response Evaluation Criteria in Solid Tumors (RECIST). Overall tumor response was achieved in 15 patients (22%). Among these 15 patients, 53% experienced durable tumor responses lasting 6 months or longer.
The most common adverse events reported by patients receiving iobenguane I 131 included lymphopenia, neutropenia, thrombocytopenia, fatigue, anemia, increased international normalized ratio, nausea, dizziness, hypertension, and vomiting.
Iobenguane I 131, from Progenics Pharmaceuticals, Inc, is a radiolabeled molecule similar to noradrenaline. The company said this approval is welcome news to patients with pheochromocytoma and paraganglioma, since there is currently an extremely limited number of treatment options available to them.
Iobenguane I 131 comes with a warning about radiation exposure to patients and family members. Contact should be minimized while the patient is receiving treatment. The risk of radiation exposure is greater in pediatric patients, according to the FDA. Other warnings and precautions include a risk of myelosuppression, underactive thyroid, elevations in blood pressure, renal failure or renal injury, and pneumonitis. Myelodysplastic syndrome and acute leukemias were observed in patients who received iobenguane I 131, and the magnitude of this risk will continue to be studied.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.