Fedratinib Reduced Spleen Volume in Ruxolitinib-Resistant Myelofibrosis
Patients with myelofibrosis resistant or intolerant to ruxolitinib may have an alternative treatment option with the JAK2-selective inhibitor fedratinib, according to the results of a phase II study.
Patients with myelofibrosis resistant or intolerant to ruxolitinib may have an alternative treatment option with the JAK2-selective inhibitor fedratinib, according to the results of a phase II study
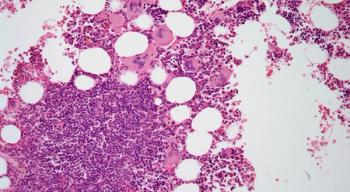
About one-half of patients with myelofibrosis have mutations in JAK2. There is currently one JAK2 inhibitor approved for these patients, ruxolitinib; however, a large percentage of patients treated with ruxolitinib in clinical trials do not achieve a 35% reduction in spleen volume and about one-half will discontinue treatment after 3 to 5 years.
In this study, Claire N. Harrison, MD, of Guy’s and St. Thomas’ NHS Foundation Trust in London, and colleagues, investigated the efficacy and safety of fedratinib in 97 patients with intermediate- or high-risk primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocytopenia myelofibrosis that was ruxolitinib resistant or intolerant.
“Overall, the results show that fedratinib was effective in reducing splenomegaly and symptom burden in patients who had previously discontinued ruxolitinib therapy due to either intolerance or resistance, as determined by the study investigators,” wrote Harrison and colleagues. “Most patients achieved a reduction in spleen volume, with more than half (55%) of patients reaching the primary endpoint at end of cycle 6 of a 35% or greater reduction in spleen volume from baseline.”
Patients received oral fedratinib at a dose of 400 mg once per day for 6 consecutive 28-day cycles. The primary endpoint was spleen response, defined as the proportion of patient with a 35% or greater reduction in spleen volume. The primary analysis was done in the per protocol population.
All enrolled patients received at least one dose of fedratinib with a median of 6 cycles of therapy given. Thirty-nine percent of patient required at least one dose reduction; the most common reason for reduction was gastrointestinal disorders.
With a median follow-up of 6 months, 55% of patients achieved a spleen response as defined by the primary endpoint. Fifty-three percent of the ruxolitinib resistant and 63% of the ruxolitinib intolerant patients achieved a response at the end of cycle 6. Overall, the median percentage change in spleen volume at the end of cycle 6 was –34%.
“Although the primary endpoint was met, early termination of the trial precluded assessment of the duration of spleen response,” the researchers wrote.
About one-quarter (26%) of patients achieved a 50% or greater reduction in total symptom score compared with baseline.
All patients in the study had at least one adverse event. The most common hematologic events were anemia and thrombocytopenia. The most common non-hematologic events were gastrointestinal symptoms such as diarrhea, nausea, and vomiting. About one-third of patients had a serious adverse event, including cardiac disorders, pneumonia, and pleural effusion. None of the deaths that occurred during the study were related to the study drug.
“The importance of the responses to fedratinib in this study are further underscored by data suggesting that patients who develop progressive disease, even after initial response to ruxolitinib, might fare badly with other salvage therapies such as transplantation and have a poor overall survival after stopping ruxolitinib, which is currently the only approved JAK inhibitor for myelofibrosis therapy,” the researchers wrote.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.