- ONCOLOGY Vol 12 No 8
- Volume 12
- Issue 8
Gastrointestinal Toxicity of Irinotecan
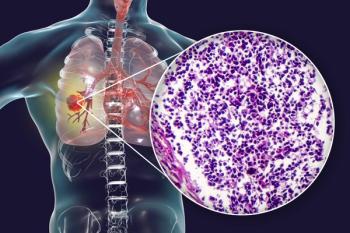
Irinotecan (CPT-11 [Camptosar]) is an important new chemotherapeutic drug that demonstrates activity against a broad spectrum of malignancies, including carcinomas of the colon, stomach, and lung. Unfortunately, frequent and
ABSTRACT: Irinotecan (CPT-11 [Camptosar]) is an important new chemotherapeutic drug that demonstrates activity against a broad spectrum of malignancies, including carcinomas of the colon, stomach, and lung. Unfortunately, frequent and often severe gastrointestinal toxicities, particularly diarrhea, have limited its more widespread use. A cholinergic syndrome resulting from the inhibition of acetylcholinesterase activity by irinotecan is frequently seen within the first 24 hours after irinotecan administration but is easily controlled with atropine. Late diarrhea occurs in the majority of patients, however, and is National Cancer Institute (NCI) grade 3 or 4 in up to 40%. The late syndrome appears to be related to the effects on the bowel of SN-38, the active metabolite of irinotecan, which undergoes biliary excretion and inactivation. Early recognition and treatment of late diarrhea with high-dose loperamide have reduced, although not entirely eliminated, patient morbidity. Further study is needed to identify the mechanism of irinotecan-induced late diarrhea and to evaluate potential new therapies. [ONCOLOGY 12(Suppl 6):73-78, 1998]
Irinotecan (CPT-11 [Camptosar]) is an important new drug in the chemotherapeutic armamentarium. Irinotecan is active against a broad spectrum of malignancies, including carcinomas of the colon, stomach, and lung. Unfortunately, frequent and often severe gastrointestinal toxicities, particularly diarrhea, have limited its more widespread use.
Clinical observations, preclinical models, and pharmacokinetic studies have yielded some critical insights into the pathophysiology of these side effects. Early recognition and treatment of these toxicities have resulted in a reduction in patient morbidity. Despite these new pathophysiologic insights and advances in treatment, gastrointestinal toxicities remain a major problem with the clinical use of irinotecan. The gastrointestinal side effects of irinotecan administration can be divided into two distinct syndromes: early and late.
Early toxicity occurs within the first 24 hours of irinotecan administration and is characterized by diarrhea, emesis, diaphoresis, abdominal cramping, and, less commonly, hyperlacrimation and rhinorrhea.[1] Various components of the syndrome have been reported in up to 80% of patients receiving the drug.[2,3]
The spectrum of symptoms appears to be dose-related. Patients who receive lower doses experience abdominal cramping, diarrhea, and diaphoresis, while those given over 300 mg/m2 also complain of salivation, hyperlacrimation, and visual changes.[4] In a study of patients treated with 250 mg/m2 of irinotecan every 2 weeks, Petit et al found that most symptoms occurred within the first 2 hours, and median duration was approximately 30 minutes.[5]
The constellation of early symptoms is consistent with cholinergic hyperstimulation. Irinotecan has been shown to mimic the effects of acetylcholine in various in vitro preparations.[6] This action is mediated by inhibition of acetylcholinesterase and, perhaps less importantly, by direct binding to and stimulation of muscarinic receptors (Figure 1).[7]
In both animal models and humans, symptoms are inhibited by administration of the anticholinergic drug atropine.[8] Atropine as needed is now routinely used in patients treated with irinotecan, and the incidence of cholinergic symptoms severe enough to interfere with treatment is quite low. In the series of Petit et al, the use of atropine was required in 34% of patients, and only one case of grade 3 early diarrhea occurred despite the use of a relatively high dose of irinotecan.[5]
In contrast to early diarrhea, late diarrhea, defined as that occurring more than 24 hours after irinotecan administration, is a common and often serious and dose-limiting side effect. Although usually controllable with nonspecific and supportive measures, late diarrhea can be particularly dangerous in elderly or debilitated patients who experience other toxicities, such as neutropenia.[1]
Incidence
The overall incidence of late diarrhea in most US and European phase I and II trials of irinotecan ranges from 60% to 87% and appears to be dose-dependent.[1,9-11] The incidence of severe (National Cancer Institute [NCI] grade 3 or 4) diarrhea in these studies varies from 20% to 40%.[1,9-12] The incidence in Japanese studies is somewhat lower; however, most of these studies used less intensive dosing regimens.[13]
Timing
The onset and duration of late diarrhea may vary with the dosing schedule. In European studies in which patients received 350 mg/m2 every 3 weeks, the median time to onset was 5 days and the median duration was 5 days.[11] In the pivotal American trials, in which patients received 125 mg/m2/wk for 4 out of 6 weeks, the median time to onset was 11 days, and the median duration was 2 days (Figure 2).[14]
Predisposing Factors
Identification of patient characteristics that predispose to diarrhea may allow for the identification of patients who require close monitoring and early treatment. Unfortunately, this approach has not proven to be clinically useful.
In European studies, age older than 65 years, prior pelvic irradiation, and low performance status were significantly associated with an increased incidence of severe diarrhea.[1,3,11] In American studies, however, the results are conflicting. Von Hoff reported that ³ 65 years was a risk factor for grade 3/4 diarrhea,[14] whereas Pazdur found no significant increase in these patients.[12] Schaaf et al uncovered no differences in irinotecan pharmacokinetics between patients older and younger than 65 years of age.[15]
Etiology
In normal states, intestinal fluids remain in homeostasis, maintaining a finely regulated balance between fluid secretion and absorption. The intestines receive 8 to 9 L of ingested and secreted fluids each day and absorb all but 100 to 200 mL.[16] Alteration of this balance by increased secretion or reduced absorption may result in the clinical symptom of diarrhea.
One potential mechanism by which drugs may induce diarrhea is direct damage to the intestinal epithelium. The resulting denuded mucosa is leaky and unable to absorb fluid. This is the probable mechanism of fluorouracil-induced diarrhea, which results from diffuse mucosal injury.[17,18] Alternatively, compounds may increase secretion or decrease absorption of fluid by intestinal epithelial cells.[16]
Irinotecan Pharmacology and Metabolism--Clues to the etiology of irinotecan-induced late diarrhea may be found in the complex pharmacology and metabolism of the drug (Figure 3). Irinotecan is a prodrug that is converted to an active form, SN-38, by carboxyl-esterases, which in humans are found predominantly in the liver.[19-21] The SN-38 metabolite is 250 to 1,000 times as potent an inhibitor of topoisomerase I as irinotecan.[22]
Inhibition of topoisomerase I, which correlates with antitumor activity, results in the formation of cleavable complexes in DNA, which induce strand breaks.[23] This DNA damage is thought to lead to cell death by apoptosis,[24] which may be mediated through the interleukin-1 beta-converting enzyme (ICE) pathway.[25] Both irinotecan and SN-38 require an intact lactone ring for topoisomerase I inhibition. They are inactivated by pH-dependent hydrolysis of the ring to the hydroxy acid.[22,26]
SN-38 is further metabolized by glucuronidation to SN-38 glucuronide (SN-38G), which is inactive.[27,28]. Glucuronidation is specifically performed by the UGT*1.1 isoform of hepatic uridine diphosphate glucuronosyltransferase,[29] which also glucur- onidates bilirubin and is deficient in Gilberts syndrome.[30] The SN-38G metabolite can also be deconjugated back to SN-38 in the gut by bacterial glucuronidases, which may result in increased exposure of the intestinal epithelium to toxic products. Takasuna et al found a correlation between intestinal bacterial beta-glucuronidase activity and the site of epithelial damage in rats exposed to irinotecan.[31]
Biliary excretion is an important mechanism in the elimination of irinotecan and its metabolites, with 25%, 2%, and 1% of a dose excreted in the bile as irinotecan, SN-38G, and SN-38, respectively.[32] Levels of irinotecan and SN-38 in the bile are up to 113- and 40-fold higher than levels in plasma.[33] Normal excretion of these compounds into the bile is via the canalicular multispecific organic anion transporter (cMOAT), as well as other less-well characterized transporters.[34,35] Treatment with cyclosporine (Neoral, Sandimmune), which decreases biliary flow and inhibits MOAT, increases the areas under the curve (AUCs) of irinotecan, SN-38, and SN-38G severalfold.[36]
The relationship between the pharmacokinetics of irinotecan and its metabolites and diarrhea is also quite complex. Both the parent compound and metabolites undergo enterohepatic circulation, and the concentration of SN-38 has been correlated with diarrhea in mice[37] and in humans.[10,38,39] Ratains group found that a calculated biliary index [AUCCPT-11 × (AUCSN-38/AUCSN-38G)] was predictive of diarrhea.[40,41] However, Conti et al did not find the biliary index or other pharmacokinetic parameters to correlate with diarrhea in patients dosed with irinotecan weekly.[10] The clinical usefulness of any of these measures is limited by the large overlap between putative high- and low-risk groups. Wasserman et al reported severe irinotecan toxicity in two patients with Gilberts syndrome, in which glucuronida- tion is deficient.[42] This finding indicates the importance of glucuronidation in the detoxification of irinotecan and its metabolites. Patients with Gilberts syndrome, which may be found in up to 6% of the general population,[43-45] may constitute a group at high risk for late diarrhea.
In rats, treatment with valproic acid, which competes for glucuronidation with SN-38, reduced SN-38G by 99% and increased the AUC of SN-38 by 270%.[46] Phenobarbital, an inducer of glucuronidation, increased the AUC of SN-38G while decreasing the AUCs of irinotecan and SN-38.[46]
Unresolved Questions--Several questions remain, however: Why is the gastrointestinal tract preferentially affected by irinotecan or its metabolites, and by what mechanism do they induce diarrhea? The excretion of biliary irinotecan and SN-38 may expose the intestinal mucosa to high levels of the compound responsible for late diarrhea.
Further investigation of late diarrhea has been hampered by the lack of a pathologic correlation with symptoms. There have been several animal studies revealing bowel injury,[31,47] but no comparable human reports, though human studies are under way. Ikuno et al reported that mice treated with irinotecan exhibited intestinal wall thinning with epithelial vacuolation, vascular dilatation, and an inflammatory cell infiltrate. There was evidence of apoptosis in the ileum, as well as epithelial cell hyperplasia with goblet cell metaplasia in the cecum.[47]
Interspecies variation may exist with respect to susceptibility to irinotecan toxicity. Guffroy and Hodge observed villous atrophy in the small intestine but not cecal lesions in their mouse studies.[48] Takasuna et al found characteristic intestinal changes that appeared in a time-dependent fashion in rats treated with irinotecan. Gross thinning of both the intestines and cecum was seen. Histologically, there was cell death and apoptosis with crypt dropout, followed by the development of severe submucosal edema and an inflammatory infiltrate.[31]
These results indicate that, at least in these models, diarrhea may result from a direct toxic action of irinotecan on the intestinal mucosa. One small human study of irinotecan-induced late diarrhea, reported in abstract form only, found normal d-xylose absorption, indicating a relatively intact intestinal mucosa[49] but increased clearance of alpha-1-antitrypsin, which is associated with protein-losing enteropathy.[50]
Other Effects of Irinotecan and Its Metabolites on the Intestinal Mucosa--Irinotecan and its metabolites may have additional effects on the intestinal mucosa that may induce diarrhea. In the normal intestine, secretion of fluid is driven by active secretion of chloride.[51] Chloride is actively transported into the cell across the basolateral membrane by the Na+:K+:2Cl- cotransporter and then exits the cell via chloride channels along an electrochemical gradient.
In the rat, Sakai et al demonstrated that colonic chloride secretion, as measured with Ussing chambers as a short-circuit current, is stimulated by irinotecan.[52] This stimulation is mimicked by stable analogs of the unstable thromboxane A2 and is blocked by inhibitors of cyclooxygenase, thromboxane synthase, and thromboxane A2 receptors.[53] Our unpublished data show that SN-38 stimulates the short-circuit current in human colonic mucosa, indicating that a metabolite of irinotecan can induce chloride secretion. This effect is abrogated by cyclooxygenase inhibition.
Irinotecan may induce inflammation and intestinal secretion by paracrine mechanisms as well. Exposure of both mouse and human mononuclear cells to irinotecan induces secretion of tumor necrosis factor (TNF).[54] Expression of TNF is associated with AIDS-related diarrhea and induces chloride secretion in colonocytes.[55] Tumor necrosis factor also induces inflammation and may be important in the pathogenesis of inflammatory conditions, such as Crohns disease.[56]
Therapy
Nonspecific Measures--Nonspecific measures have proven partially effective in the treatment of irinotecan-induced late diarrhea. Abigereges et al showed that loperamide, an opiate analog, reduces the incidence of severe diarrhea when given in an intensive fashion.[57] This entails the administration of 2 mg of loperamide every 2 hours until the patient is free of diarrhea for 12 hours.
A modification of this regimen using a 4-mg initial dose and then 4 mg every 4 hours at night has become the standard for clinical studies and is recommended in the US clinical labeling for irinotecan.[58] Although no randomized studies of this loperamide regimen have been performed, the incidence of grade 3 and 4 diarrhea fell from 24% to 9% in patients so treated in American studies.[2] At these doses, loperamide probably reduces diarrhea by delaying intestinal transit, allowing increased time for fluid absorption.[16]
Opioids may also reduce fluid secretion by activating opioid receptors. Acetorphan, an enkephalinase inhibitor available in Europe, has also been used with some success in irinotecan-induced diarrhea in several small studies.[1,16,49,59]
Octreotide (Sandostatin), a synthetic, longer-acting analog of somatostatin available for the treatment of the symptoms of neuroendocrine tumors, reduces intestinal secretion and motility.[60] It may be useful in the treatment of severe fluorouracil-induced diarrhea.[61,62] Although octreotide has been used anecdotally in the treatment of irinotecan-induced late diarrhea, it has not been studied rigorously.
Rustum et al recently showed that treatment with the cytokine IL-15 significantly reduced the incidence of diarrhea and death without affecting antitumor activity in a rat model of irinotecan administration. The mechanism of this protective effect remains unclear.[63]
Other potential therapies are in various stages of development and study. Some have been used in other types of diarrhea, while others are specific to irinotecan. For example, the use of intestinal growth factors, such as keratinocyte growth factor (KGF), stem-cell factor, and glucagon-like peptide 2, is being explored to reduce the side effects caused by radiation and various types of chemotherapy.[64-66] Direct stimulation of intestinal stem cells by growth factors may reduce the extent and duration of mucosal damage and diarrhea. Multicenter trials assessing the efficacy of KGF in the prevention of fluorouracil-induced mucositis currently are under way (L. Rosen, personal communication, October, 1997).
Alteration of Irinotecan Metabolism--Another potential strategy to reduce irinotecan-induced late diarrhea is to alter the metabolism of the parent drug and its metabolites to reduce intestinal exposure to toxic compounds. The complex metabolism and pharmacokinetics of irinotecan offer a number of potential targets for manipulation.
Since SN-38G, the glucuronide of SN-38, appears to be an inactive metabolite, attempts have been made to alter glucuronidation. Gupta et al showed that phenobarbital administration increases glucuronidation of SN-38 in rats and lowers plasma SN-38 concentrations.[46] Reductions in gastrointestinal toxicity have been noted in patients with neurologic malignancies treated with irinotecan. In one recent series of 60 glioma patients, most of whom were receiving antiseizure medications, no patient had severe diarrhea.[67] Certain antiepileptic drugs may induce UGT activity, while valproic acid decreases SN-38 glucuronidation in animal models.[46] Only one patient in this study was receiving valproate alone, and pharmacokinetic studies are currently under way.
In our experience treating 32 patients with brain malignancies with irinotecan at the University of California, Los Angeles, we found only two cases of grade 3 or 4 diarrhea. One of these patients was taking valproic acid alone, while the other was not receiving any antiepileptics (T. Cloughesy, personal communication, October, 1997). Most other drugs tested so far, however, have had little effect on glucuronidation of SN-38.[20]
Glucuronidation of SN-38 may also be reduced by inhibiting bacterial glucuronidase activity in the gut. Treatment of rats with orally administered penicillin and streptomycin eliminated bacterial deconjugation of SN-38G in the stool and ameliorated mucosal damage and diarrhea.[31]
Another method of reducing glucuronidase has been the use of traditional Japanese herbal (Kampo) medications. These medications contain various natural glucuronides, such as baicalin, which can inhibit bacterial glucuronidases[68,69] and reduce diarrhea in animal studies. Although increasing glucuronidation of SN-38 in the intestinal lumen may improve diarrhea, it is unclear what effects this may have on plasma SN-38 levels and therapeutic efficacy.
Reducing the excretion of toxic metabolites into the gastrointestinal tract may also affect late diarrhea. As previously mentioned, drugs such as cyclosporine may inhibit biliary excretion of irinotecan and its metabolites.[36] Human trials are under way to determine the pharmacokinetic and side effect profile of the coadministration of cyclosporine and irinotecan.[70]
Chronobiologic modulation may offer a means of reducing irinotecan-induced toxicity. In animal studies, Ohdo et al showed that bone marrow toxicity and pharmacokinetics of irinotecan were circadian-rhythm-dependent in mice. [69] Gallbladder emptying, which occurs in a daily pattern, is stimulated by eating via release of cholecystokinin from and activation of neural pathways in the small intestine.[72] Proper timing of irinotecan dosing could possibly alter the drugs metabolism and reduce intestinal exposure to toxic metabolites, although this has not been studied.
Another theoretical method to ameliorate irinotecan-induced diarrhea would be to alter the proportion of active irinotecan and SN-38 in the lumen by reducing the proportion in the lactone form. This conversion is pH-dependent,[26] and altering stool pH may be another pathway for the effects of antibiotics on late diarrhea.
Finally, the cytoprotectant amifostine (Ethyol) specifically reduces DNA damage by preferentially scavenging free radicals in nonmalignant cells. Amifostine has been shown to reduce the toxicities of radiation, cisplatin (Platinol), and alkylating agents in normal tissues.[73] Although the effects of irinotecan do not appear to be mediated by the generation of free radicals, a phase II trial of the combination of irinotecan and amifostine is currently under way (D. Prager: personal communication, October, 1997).
Blockade of Irinotecan-Induced Fluid Secretion--If irinotecan-induced secretion is responsible for at least part of the pathophysiology of late diarrhea, specific inhibitors may be useful therapeutically. In animal models, thromboxane A2 appears to be important in the induction of increased chloride excretion. One method of reducing thromboxane A2 would be to block cyclooxygenase-mediated metabolism of arachidonic acid to prostaglandin H2, which is required for thromboxane synthesis.[74] Although indomethacin blocks irinotecan-induced colonic chloride secretion in vitro,[53] nonspecific cyclooxygenase inhibitors have a high incidence of gastrointestinal and hematologic side effects.[75] The use of specific cyclooxygenase 2 inhibitors, which will soon be available, may avoid the gastrointestinal toxicities of nonspecific inhibitors.[76] Another option would be to use specific thromboxane synthase inhibitors, some of which are already approved for the treatment of asthma in Japan.[77]
The activity of irinotecan against a broad spectrum of malignancies heralds the widespread use of this important new chemotherapeutic drug. With increasing experience, the gastrointestinal toxicities of irinotecan have become better defined and at least partially managed.
Despite the advent of high-dose loperamide therapy, late diarrhea remains a major dose-limiting toxicity, resulting in significant patient morbidity and occasional mortality. The work of Japanese, American, and European investigators has hinted at potential mech- anisms of and possible therapies for late diarrhea. Additional animal and human studies are required to specifically identify underlying causes and potential therapies.
References:
1. Bleiberg H, Cvitkovic E: Characterization and clinical management of CPT-11 (irinotecan)-induced adverse events: The European perspective. Eur J Cancer 32A (suppl 3):S18-23, 1996.
2. Rothenberg ML: Topoisomerase I inhibitors: Review and update. Ann Oncol 8:837-855, 1997.
3. Rougier P, Bugat R, Douillard JY, et al: Phase II study of irinotecan in the treatment of advanced colorectal cancer in chemotherapy-naive patients and patients pretreated with fluorouracil-based chemotherapy. J Clin Oncol 15:251-260, 1997.
4. Abigerges D, Chabot GG, Armand JP, et al: Phase I and pharmacologic studies of the camptothecin analog irinotecan administered every 3 weeks in cancer patients. J Clin Oncol 13:210-221, 1995.
5. Petit RG, Rothenberg ML, Mitchell EP, et al: Cholinergic symptoms following CPT-11 infusion in a phase II multicenter trial of 250 mg/m2 irinotecan (CPT-11) given every 2 weeks (abstract). Proc Am Soc Clin Oncol 16:268a, 1997.
6. Takayanagi I, Koike K, Tagawa M, et al: Some pharmacological properties of a new antitumor drug, CPT-11, in isolated muscle preparations. Gen Pharmacol 20:763-766, 1989.
7. Kawato Y, Sekiguchi M, Akahane K, et al: Inhibitory activity of camptothecin derivatives against acetylcholinesterase in dogs and their binding activity to acetylcholine receptors in rats. J Pharm Pharmacol 45:444-448, 1993.
8. Gandia D, Abigerges D, Armand JP, et al: CPT-11-induced cholinergic effects in cancer patients (letter). J Clin Oncol 11:196-197, 1993.
9. Rothenberg ML, Eckardt JR, Kuhn JG, et al: Phase II trial of irinotecan in patients with progressive or rapidly recurrent colorectal cancer. J Clin Oncol 14:1128-1135, 1996.
10. Conti JA, Kemeny NE, Saltz LB, et al: Irinotecan is an active agent in untreated patients with metastatic colorectal cancer. J Clin Oncol 14:709-715, 1996.
11. Rougier P, Bugat R: CPT-11 in the treatment of colorectal cancer: Clinical efficacy and safety profile. Semin Oncol 23:34-41, 1996.
12. Pazdur R, Zinner R, Rothenberg ML, et al: Age as a risk factor in irinotecan (CPT-11) treatment of 5-FU-refractory colorectal cancer (abstract). Proc Am Soc Clin Oncol 16:260a, 1997.
13. Shimada Y, Yoshino M, Wakui A, et al: Phase II study of CPT-11, a new camptothecin derivative, in metastatic colorectal cancer: CPT-11 Gastrointestinal Cancer Study Group. J Clin Oncol 11:909-913, 1993.
14. Von Hoff DD, Rothenberg ML, Pitot HC, et al: Irinotecan (CPT-11) therapy for patients with previously treated metastatic colorectal cancer (CRC): Overall results of FDA-reviewed pivotal US clinical trials (abstract). Proc Am Soc Clin Oncol 16:228a, 1997.
15. Schaaf L, Ichhpurani N, Elfring G, et al: Influence of age on the pharmacokinetics of irinotecan (CPT-11) and its metabolites, SN-38 and SN-38 glucuronide (SN-38G), in patients with previously treated colorectal cancer (abstract). Proc Am Soc Clin Oncol 16:202a, 1997.
16. Sellin JH: Intestinal electrolyte absorption and secretion, in Feldman M, Scharschmidt BF, Sleisenger M (eds): Sleisenger and Fordtrans Gastrointestinal and Liver Disease, pp 1451-1471. Philadelphia, WB Saunders, 1998.
17. Grem JL, Shoemaker DD, Petrelli NJ, et al: Severe and fatal toxic effects observed in treatment with high- and low-dose leucovorin plus 5-fluorouracil for colorectal carcinoma. Cancer Treat Rep 71:1122, 1987.
18. Lewis JH: Gastrointestinal injury due to medicinal agents. Am J Gastroenterol 81:819-834, 1986.
19. Satoh T, Hosokawa M, Atsumi R, et al: Metabolic activation of CPT-11, 7-ethyl-10-[4-(1-piperidino)-1- piperidino] carbonyloxycamptothecin, a novel antitumor agent, by carboxylesterase. Biol Pharm Bull 17:662-664, 1994.
20. Haaz MC, Rivory LP, Riche C, et al: The transformation of irinotecan (CPT-11) to its active metabolite SN-38 by human liver microsomes: Differential hydrolysis for the lactone and carboxylate forms. Naunyn Schmiedebergs Arch Pharmacol 356:257-262, 1997.
21. Slatter JG, Su P, Sams JP, et al: Bioactivation of the anticancer agent CPT-11 to SN-38 by human hepatic microsomal carboxylesterases and the in vitro assessment of potential drug interactions. Drug Metab Dispos 25:1157-1164, 1997.
22. Kawato Y, Aonuma M, Hirota Y, et al: Intracellular roles of SN-38, a metabolite of the camptothecin derivative CPT-11, in the antitumor effect of CPT-11. Cancer Res 51:4187-4191, 1991.
23. Pommier Y: Eukaryotic DNA topoisomerase I: Genome gatekeeper and its intruders, camptothecins. Semin Oncol 23:3-10, 1996.
24. Suzuki A, Kato M: Chemotherapeutic agent CPT-11 induces the new expression of the apoptosis initiator to the cytoplasm. Exp Cell Res 227:154-159, 1996.
25. Suzuki A, Iwasaki M, Kato M, et al: Sequential operation of ceramide synthesis and ICE cascade in CPT-11-initiated apoptotic death signaling. Exp Cell Res 233:41-47, 1997.
26. Sasaki Y, Yoshida Y, Sudoh K, et al: Pharmacological correlation between total drug concentration and lactones of CPT-11 and SN-38 in patients treated with CPT-11. Jpn J Cancer Res 86:111-116, 1995.
27. Atsumi R, Suzuki W, Hakusui H: Identification of the metabolites of irinotecan, a new derivative of camptothecin, in rat bile and its biliary excretion. Xenobiotica 21:1159-1169, 1991.
28. Rivory LP, Robert J: Identification and kinetics of a beta-glucuronide metabolite of SN-38 in human plasma after administration of the camptothecin derivative irinotecan. Cancer Chemother Pharmacol 36:176-179, 1995.
29. Iyer L, King C, Tephly T, et al: UGT isoform 1.1 (UGT*1.1) glucuronidates SN-38, the active metabolite of irinotecan (abstract). Proc Am Soc Clin Oncol 16:201a, 1997.
30. Bosma PJ, Chowdhury JR, Bakker C, et al: The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilberts syndrome. N Engl J Med 333:1171-1175, 1995.
31. Takasuna K, Hagiwara T, Hirohashi M, et al: Involvement of beta-glucuronidase in intestinal microflora in the intestinal toxicity of the antitumor camptothecin derivative irinotecan hydrochloride (CPT-11) in rats. Cancer Res 56:3752-3757, 1996.
32. Chabot GG: Clinical pharmacokinetics of irinotecan. Clin Pharmacokinet 33:245-259, 1997.
33. Wiseman LR, Markham A: Irinotecan: A review of its pharmacological properties and clinical efficacy in the management of advanced colorectal cancer. Drugs 52:606-623, 1996.
34. Chu XY, Kato Y, Sugiyama Y: Multiplicity of biliary excretion mechanisms for irinotecan, CPT-11, and its metabolites in rats. Cancer Res 57:1934-1938, 1997.
35. Chu XY, Kato Y, Niinuma K, et al: Multispecific organic anion transporter is responsible for the biliary excretion of the camptothecin derivative irinotecan and its metabolites in rats. J Pharmacol Exp Ther 281:304-314, 1997.
36. Gupta E, Safa AR, Wang X, et al: Pharmacokinetic modulation of irinotecan and metabolites by cyclosporin A. Cancer Res 56:1309-1314, 1996.
37. Araki E, Ishikawa M, Iigo M, et al: Relationship between development of diarrhea and the concentration of SN-38, an active metabolite of CPT-11, in the intestine and the blood plasma of athymic mice following intraperitoneal administration of CPT-11. Jpn J Cancer Res 84:697-702, 1993.
38. Kudoh S, Fukuoka M, Masuda N, et al: Relationship between the pharmacokinetics of irinotecan and diarrhea during combination chemotherapy with cisplatin. Jpn J Cancer Res 86:406-413, 1995.
39. Sasaki Y, Hakusui H, Mizuno S, et al: A pharmacokinetic and pharmacodynamic analysis of CPT-11 and its active metabolite SN-38. Jpn J Cancer Res 86:101-110, 1995.
40. Mick R, Gupta E, Vokes EE, et al: Limited-sampling models for irinotecan pharmacokinetics-pharmacodynamics: Prediction of biliary index and intestinal toxicity. J Clin Oncol 14:2012-2019, 1996.
41. Gupta E, Lestingi TM, Mick R, et al: Metabolic fate of irinotecan in humans: Correlation of glucuronidation with diarrhea. Cancer Res 54:3723-3725, 1994.
42. Wasserman E, Myara A, Lokiec F, et al: Severe CPT-11 toxicity in patients with Gilberts syndrome: Two case reports. Ann Oncol 8:1049-1051, 1997.
43. Gwee KA, Koay ES, Kang JY: The prevalence of isolated unconjugated hyperbilirubinaemia (Gilberts syndrome) in subjects attending a health screening programme in Singapore. Singapore Med J 33:588-589, 1992.
44. Chowdury JR, Chowdury NR: Unveiling the mysteries of inherited disorders of bilirubin glucuronidation. Gastroenterology 105:288-293, 1993.
45. Owens D, Evans J: Population studies on Gilberts syndrome. J Med Genet 12:152-156, 1975.
46. Gupta E, Wang X, Ramirez J, et al: Modulation of glucuronidation of SN-38, the active metabolite of irinotecan, by valproic acid and phenobarbital. Cancer Chemother Pharmacol 39:440-444, 1997.
47. Ikuno N, Soda H, Watanabe M, et al: Irinotecan (CPT-11) and characteristic mucosal changes in the mouse ileum and cecum. J Natl Cancer Inst 87:1876-1883, 1995.
48. Guffroy M, Hodge T: Re: Irinotecan (CPT-11) and characteristic mucosal changes in the mouse ileum and cecum (letter; comment). J Natl Cancer Inst 88:1240-1241, 1996.
49. Hagipantelli R, Saliba F, Misset JL, et al: Pathophysiology and therapy of irinotecan (CPT-11) induced delayed onset diarrhea (abstract). Proc Am Soc Clin Oncol 14:464, 1995.
50. Florent C, LHirondel C, Desmazures C, et al: Intestinal clearance of alpha 1-antitrypsin. A sensitive method for the detection of protein-losing enteropathy. Gastroenterology 81:777-780, 1981.
51. Field M, Rao MC, Chang EB: Intestinal electrolyte transport and diarrheal disease (1). N Engl J Med 321:800-806, 1989.
52. Sakai H, Diener M, Gartmann V, et al: Eicosanoid-mediated Cl-secretion induced by the antitumor drug, irinotecan (CPT-11), in the rat colon. Naunyn Schmiedebergs Arch Pharmacol 351:309-314, 1995.
53. Sakai H, Sato T, Hamada N, et al: Thromboxane A2, released by the anti-tumour drug irinotecan, is a novel stimulator of Cl- secretion in isolated rat colon. J Physiol (Lond) 505:133-144, 1997.
54. Goto S, Okutomi T, Suma Y, et al: Induction of tumor necrosis factor by a camptothecin derivative, irinotecan, in mice and human mononuclear cells. Anticancer Res 16:2507-2511, 1996.
55. Schmitz H, Fromm M, Bode H, et al: Tumor necrosis factor-alpha induces Cl- and K+ secretion in human distal colon driven by prostaglandin E2. Am J Physiol 271:G669-674, 1996.
56. Targan SR, Hanauer SB, van Deventer SJ, et al: A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohns disease: Crohns Disease cA2 Study Group. N Engl J Med 337:1029-1035, 1997.
57. Abigerges D, Armand JP, Chabot GG, et al: Irinotecan (CPT-11) high-dose escalation using intensive high-dose loperamide to control diarrhea. J Natl Cancer Inst 86:446-449, 1994.
58. Pharmacia & Upjohn: Irinotecan Package Insert.
59. Goncalves E, de Costa L, Abigerges D, et al: A new enkephalinase inhibitor as an alternative to loperamide in the prevention of diarrhea induced by CPT-11. J Clin Oncol 13:2144-216, 1995.
60. Lamberts SW, van der Lely AJ, de Herder WW, et al: Octreotide. N Engl J Med 334:246-254, 1996.
61. Wadler S, Haynes H, Wiernik PH: Phase I trial of the somatostatin analog octreotide acetate in the treatment of fluoropyrimidine-induced diarrhea. J Clin Oncol 13:222-226, 1995.
62. Cascinu S, Fedeli A, Fedeli SL, et al: Octreotide versus loperamide in the treatment of fluorouracil-induced diarrhea: A randomized trial. J Clin Oncol 11:148-151, 1993.
63. Rustum YM, Cao S, Black JD, et al: Interleukin-15 offers selective protection from CPT-11 induced in vivo toxicity in rats bearing advanced colorectal cancer. Proc Am Soc Clin Oncol 17:196a, 1998.
64. Khan WB, Shui C, Ning S, et al: Enhancement of murine intestinal stem cell survival after irradiation by keratinocyte growth factor. Radiat Res 148:248-253, 1997.
65. Leigh BR, Khan W, Hancock SL, et al: Stem-cell factor enhances the survival of murine intestinal stem cells after photon irradiation. Radiat Res 142:12-15, 1995.
66. Drucker DJ, Erlich P, Asa SL, et al: Induction of intestinal epithelial proliferation by glucagon-like peptide 2. Proc Natl Acad Sci USA 93:7911-7916, 1996.
67. Colvin OM, Cokgor I, Ashley DM, et al: Irinotecan treatment of adults with recurrent or progressive malignant glioma. Proc Am Soc Clin Oncol 17:387a, 1998.
68. Narita M, Nagai E, Hagiwara H, et al: Inhibition of beta-glucuronidase by natural glucuronides of kampo medicines using glucuronide of SN-38 (7-ethyl-10-hydroxycamptothecin) as a substrate. Xenobiotica 23:5-10, 1993.
69. Takasuna K, Kasai Y, Kitano Y, et al: Protective effects of kampo medicines and baicalin against intestinal toxicity of a new anticancer camptothecin derivative, irinotecan hydrochloride (CPT-11), in rats. Jpn J Cancer Res 86:978-84, 1995.
70. Fagbemi S, Iyer L, Mani S, et al: Phase I and pharmacokinetic study of irinotecan (CPT-11) administered with cyclosporin A (CSA) (abstract). Proc Am Soc Clin Oncol 16:219a, 1997.
71. Ohdo S, Makinosumi T, Ishizaki T, et al: Cell cycle-dependent chronotoxicity of irinotecan hydrochloride in mice. J Pharmacol Exp Ther 283:1383-8, 1997.
72. Everson GT: Gallbladder function in gallstone disease. Gastroenterol Clin North Am 20:85-110, 1991.
73. Tannehill SP, Mehta MP: Amifostine and radiation therapy: Past, present, and future. Semin Oncol 23:69-77, 1996.
74. Sigal E: The molecular biology of mammalian arachidonic acid metabolism. Am J Physiol 260:L13-28, 1991.
75. Cryer B: Nonsteroidal anti-inflammatory drugs and gastrointestinal disease, in Feldman M, Scharschmidt BF, Sleisenger M, (eds): Sleisenger and Fordtrans Gastrointestinal and Liver Disease, pp 343-357 Philadelphia, W.B. Saunders, 1998.
76. Futaki N, Takahashi S, Yokoyama M, et al: NS-398, a new anti-inflammatory agent, selectively inhibits prostaglandin G/H synthase/cyclooxygenase (COX-2) activity in vitro. Prostaglandins 47:55-59, 1994.
77. Samara E, Cao G, Locke C, et al: Population analysis of the pharmacokinetics and pharmacodynamics of seratrodast in patients with mild to moderate asthma. Clin Pharmacol Ther 62:426-435, 1997.
Articles in this issue
over 27 years ago
CD-ROM Helps Cancer Patients Ease the Painover 27 years ago
UT Southwestern and Komen Foundation Offer Breast Care Fellowshipover 27 years ago
Controversies in the Management of Stage I Seminomaover 27 years ago
Genetic Switch May Yield Map of Prostate Cancer Machineryover 27 years ago
Personalized Approach Increases Breast Cancer Screening RatesNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.