Hematopoietic growth factors
For years, chemotherapy-associated myelosuppression has represented a major limitation to a patient’s tolerance of anticancer therapy. In addition, the clinical consequences of chemotherapy-induced myelosuppression (such as febrile neutropenia, dose reductions, or lengthy dose delays) may have had significant negative effects on quality of life or even response to treatment.
For years, chemotherapy-associated myelosuppression has represented a major limitation to a patient’s tolerance of anticancer therapy. In addition, the clinical consequences of chemotherapy-induced myelosuppression (such as febrile neutropenia, dose reductions, or lengthy dose delays) may have had significant negative effects on quality of life or even response to treatment.
Before the widespread availability of agents to stimulate host hematopoiesis, administration of antibiotics, transfusion of blood products, and reductions or delays in chemotherapy dose have been the major means of combating the myelotoxicity of chemotherapy. It is now possible to stimulate clinically relevant production of several formed elements of the blood: neutrophils, erythrocytes, and platelets.
This chapter summarizes data supporting the clinical activity of several hematopoietic growth factors. A thorough knowledge of these data will help clinicians to make judicious, informed decisions about how to use these agents most responsibly.
Hematopoietic growth factors
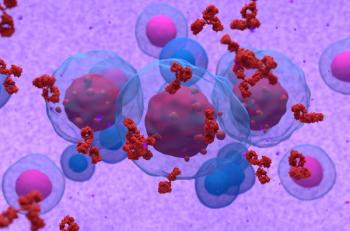
Over the past several years, a great deal of progress has been made in understanding the process of hematopoiesis by which mature cellular elements of blood are formed. Hematopoietic growth factors are a family of regulatory molecules that play important roles in the growth, survival, and differentiation of blood progenitor cells, as well as in the functional activation of mature cells.
Table 1 lists the recombinant human hematopoietic growth factors (also known as hematopoietic cytokines) that have been approved by the US Food and Drug Administration (FDA) for clinical use: granulocyte colony-stimulating factor (G-CSF, filgrastim [Neupogen]); pegfilgrastim [Neulasta]; yeast-derived granulocyte-macrophage colony-stimulating factor (GM-CSF, sargramostim [Leukine, Prokine]); recombinant human erythropoietin (epoetin alfa, EPO [Epogen, Procrit]); darbepoetin alfa (Aranesp); and interleukin-11 (IL-11, oprelvekin [Neumega]). In addition, several other hematopoietic cytokines are under clinical development.
The commercial availability of these recombinant human hematopoietic growth factors has led to their wide clinical application in oncology practice. However, the substantial costs of colony-stimulating factor utilization as supportive care for patients receiving myelosuppressive chemotherapy make it imperative to identify the optimal settings in which their use can make a significant difference in patient outcomes.
This chapter discusses the appropriate uses of only the FDA-approved hematopoietic growth factors/cytokines: G-CSF, GM-CSF, EPO, darbepoetin alfa, and IL-11. For a more detailed review of recommendations for the use of myeloid CSFs, readers are referred to the evidence-based, clinical practice guidelines developed in 1994 (last updated in 2007) by the American Society of Clinical Oncology (ASCO). The ASCO guidelines were formulated to encour-age reasonable use of CSFs when their efficacy has been well documented but to discourage excess use when marginal benefit is anticipated. These clinical practice guidelines have been published and are most easily accessed at the official web site of ASCO (
Myeloid growth factors
Three myeloid growth factors are currently licensed for clinical use in the United States: G-CSF, pegfilgrastim, and GM-CSF.
G-CSF (filgrastim) is lineage-specific for the production of functionally active neutrophils. G-CSF has been extensively evaluated in several clinical scenarios. G-CSF was first approved in 1991 for clinical use to reduce the incidence of febrile neutropenia in cancer patients receiving myelosuppressive chemotherapy.
This broad initial indication has since been expanded even further to include many other areas of oncologic practice, such as stimulation of neutrophil recovery following high-dose chemotherapy with stem-cell support. In addition, G-CSF is indicated to increase neutrophil production in endogenous myeloid disorders, such as congenital neutropenic states.
Pegylated G-CSF (pegfilgrastim) When polyethylene glycol was attached to the protein backbone of filgrastim, a new molecule (pegfilgrastim) with a longer half-life than the standard human G-CSF was created. Pegfilgrastim was approved in 2002 to reduce febrile neutropenia. It has been studied and shown to be equally efficacious as filgrastim, with the advantage of once-per-cycle dosing and self-regulating features of clearance of the drug during neutrophil recovery. Findings have suggested that pegfilgrastim is more effective than G-CSF in preventing febrile neutropenia, but further study is required. The use of pegfilgrastim in cycles < 3 weeks has not been approved; however, it has been studied in 2-week regimens and appears to be safe and effective. In addition, pegfilgrastim is not currently approved in bone marrow transplantation (BMT) or in pediatrics, but studies are under way.
GM-CSF (sargramostim), primarily a myeloid lineage-specific growth factor, stimulates the production of neutrophils, monocytes, and eosinophils. It has been extensively evaluated and received a more narrow FDA approval in 1991 for clinical use in patients with nonmyeloid malignancies undergoing autologous BMT. Since that initial indication, GM-CSF has also been approved for an expanded range of conditions, such as mitigation of myelotoxicity in patients with leukemia who are undergoing induction chemotherapy.
To date, no large-scale randomized trials have directly compared the efficacy of sargramostim with that of either filgrastim or pegfilgrastim in the same clinical setting. Future comparative trials may help to determine the optimal clinical utility of these CSFs in different clinical situations.
INDICATIONS
Uses to support chemotherapy
CSFs have been used to support both conventional and intensified doses of chemotherapy. The use of CSFs in this setting can be defined as prophylactic or therapeutic.
Prophylactic use is defined as the administration of a growth factor to prevent febrile neutropenia. “Primary prophylaxis” denotes the use of CSFs following the first cycle of multicourse chemotherapy prior to any occurrence of febrile neutropenia. The term “secondary prophylaxis” is reserved for the use of CSFs to prevent a subsequent episode of febrile neutropenia in a patient who has already experienced infectious complications in a previous chemotherapy cycle.
Primary prophylaxis G-CSF has been evaluated in at least three major randomized clinical trials in cancer patients receiving chemotherapy. The use of G-CSF as primary prophylaxis reduced the incidence of febrile neutropenia by approximately 50% in these trials, in which the incidence of febrile neutropenia in the control group was high (≥ 40%). More recently studies have evaluated the value of CSFs in patients receiving less myelosuppressive (~20%) regimens.
Vogel and colleagues evaluated a single dose of pegfilgrastim versus placebo 24 hours after chemotherapy in 950 patients with breast cancer receiving docetaxel (Taxotere; 100 mg/m2). This regimen was specifically chosen to try to assess the potential benefit of growth factor in a setting associated with approximately a 20% risk of febrile neutropenia. The placebo group experienced a 17% incidence of febrile neutropenia, compared with a 1% incidence in the pegfilgrastim group. The results from this study and other abstracts presented over the past several years suggest a benefit to pegfilgrastim at least as great or greater than that seen in the previous clinical trials that evaluated filgrastim in treatment settings where the risk of febrile neutropenia was higher. The results of this study were pivotal in the new labeling of pegfilgrastim and recommendations for prophylactic use with regimens associated with a 17% risk of febrile neutropenia. Furthermore, pharmacoeconomic sensitivity analyses have suggested that CSF use may be cost-effective if the anticipated risk of febrile neutropenia is > 20%.
A recent update of the ASCO guidelines established the threshold for use of prophylactic growth factor at 20%. In addition, the NCCN guidelines have recommended CSFs be used in regimens with a 20% risk of neutropenic fever (Table 2). In addition, certain patient risk factors for neutropenia have been identified and should be considered in conjunction with the chemotherapy regimen (Table 3).
Secondary prophylaxis Available data indicate that the use of CSFs as secondary prophylaxis in patients who have had a prior episode of febrile neutropenia can decrease the likelihood of febrile neutropenia in subsequent cycles of chemotherapy. It is important to recognize that this conclusion has never been specifically proven in any randomized clinical trial. Rather, it has been derived from analyses of subsets of patients who crossed over from the placebo arms of the initial randomized clinical trials, as well as large clinical experience.
Thus, in clinical settings where maintenance of chemotherapy dose appears to be important, secondary prophylaxis with CSFs to prevent new episodes of neutropenic fever is appropriate. CSF support can also be considered to maintain standard-dose delivery of chemotherapy when the maintenance of dose may impact outcome.
Therapeutic use is defined as the administration of a growth factor at the time when neutropenia or neutropenic fever is documented in a patient who had not been receiving CSFs previously.
Clinical trials do not support the routine use of CSFs as an adjunct to antibiotics in the treatment of all patients with uncomplicated febrile neutropenia. However, in certain high-risk patients who have features predictive of poor outcome (eg, sepsis syndrome, pneumonia, fungal infection), use of a CSF with antibiotics may be justified. To conduct appropriate clinical trials to test the hypothesis that CSF support may improve the outcomes of subsets of patients, selection of patients based on risk-stratification criteria that have been validated to predict poor outcomes or delayed recovery from neutropenia will be critical. Certain trials performed with more selective entry criteria (such as absolute neutrophil count [ANC] < 100 cells/µL) have, in fact, shown statistically significant benefits from the use of CSFs as an adjunct to antibiotics in these high-risk patients with febrile neutropenia. Continued analyses of these data and the performance of larger scale, confirmatory studies are needed to further assess the therapeutic use of CSFs.
There are no indications for CSF use to treat uncomplicated neutropenia without fever. A large-scale randomized clinical trial noted no difference in patients who had CSF support in whom afebrile neutropenia was detected versus those patients whose hematologic status was allowed to recover spontaneously without CSF support. Thus, low neutrophil counts alone do not represent a reason to prescribe CSF support. One effective way to use CSFs is prophylactically, 24 hours after chemotherapy is completed.
Use to increase dose intensity of chemotherapy
The available evidence indicates that CSF use can permit chemotherapy dose maintenance or allow modest increases in dose intensity in clinical scenarios where the main toxicity is neutropenia. Recently, delivery of dose-dense chemotherapy every 2 weeks with G-CSF support has improved survival compared with standard every-3-week dosing in women with breast cancer receiving adjuvant cyclophosphamide and doxorubicin, followed by paclitaxel. This promising dose-dense approach warrants study in other settings. Outside this setting of dose-dense adjuvant chemotherapy, the study of dose density/intensity should be limited to clinical trials.
Meanwhile, in patients with potentially curable disease for which chemotherapy dose delivery may be critical, the use of CSF support to maintain dose intensity may be appropriate. In settings where dose is not a critical determinant of outcomes, modification of chemotherapy dose and implementation of reasonable supportive care measures remain sound alternatives.
Use following stem-cell transplantation
Autologous stem-cell and/or BMT High-dose chemotherapy with autologous hematopoietic stem-cell support has been used in the treatment of several malignancies, based on the notion that dose intensity may be an important determinant of response in chemosensitive malignancies. The prolonged period of myelosuppression following such cell-supported high-dose therapy, with its attendant increased risk of infectious and bleeding complications, has been deemed justifiable in such diseases as Hodgkin lymphoma, other lymphomas, multiple myeloma, high-risk or relapsed germ-cell cancers, and sarcomas, for which other less toxic therapeutic options yield suboptimal outcomes.
Several randomized trials have documented that CSFs can effectively reduce the duration of neutropenia, infectious complications, and hospitalization in patients who are receiving high-dose cytotoxic treatment with autologous BMT. GM-CSF was the first hematopoietic growth factor evaluated and approved for clinical use in this setting. G-CSF has subsequently been approved for this indication as well. Pegfilgrastim is under study.
Allogeneic BMT Similar beneficial effects of CSFs have been seen following allogeneic BMT, and the routine use of hematopoietic growth factors is appropriate in this setting. There has been no evidence of any increase in graft-versus-host disease, graft rejection, or relapse with the use of CSFs.
Delayed or inadequate neutrophil engraftment CSFs can also be useful in patients who have delayed or inadequate neutrophil engraftment following progenitor cell transplantation.
Mobilization of peripheral blood progenitor cells
CSFs have been used successfully to enhance mobilization of peripheral blood progenitor cells (PBPCs) into the peripheral blood. Available data suggest that mobilization of PBPCs may decrease the costs of harvesting cells and post-transplantation supportive care. Reinfusion of mobilized PBPCs following high-dose chemotherapy results in more rapid hematopoietic recovery than does autologous BMT. CSFs have also been utilized to mobilize donor PBPCs for allogeneic transplantation.
Administration of CSFs can enhance hematopoietic recovery following PBPC transplantation.
Use in myeloid malignancies
Acute myelogenous leukemia Since myeloid leukemia cells express receptors for CSFs, there has been a concern that leukemia cells might be stimulated after chemotherapy. However, given the high incidence of infectious complications following induction therapy for acute myelogenous leukemia (AML), especially in older patients, studies have evaluated CSFs in this setting. Data from several such studies demonstrate that CSFs, when given after the completion of induction chemotherapy, can shorten the duration of neutropenia and may reduce infectious complications. There does not appear to be any detrimental effect, on either response rate or regrowth of leukemia, by CSF administration following induction therapy.
GM-CSF has been approved for use in patients with AML (≥ 55 years old) following induction therapy to shorten the time to neutrophil recovery and to reduce severe, life-threatening infections. Clinical data on the use of CSFs in younger patients (< 55 years old) are currently limited. G-CSF has also proved to be effective in mitigating the myelotoxicity of leukemia therapy without increasing the risk of leukemic relapse or impairing response rates.
Myelodysplastic syndrome Patients with myelodysplastic syndrome (MDS) are prone to infections related to neutropenia and functional abnormalities of mature neutrophils. Although no data supporting the safety of long-term CSF use are available, short-term use of CSFs may be appropriate in severely neutropenic patients who experience recurrent infections. CSFs have not been shown to have a significant impact on clinical outcomes in patients with MDS or other marrow dysfunction states overall, perhaps reflecting abnormalities in the underlying stem-cell pool, which is unable to respond optimally to pharmacologic doses of CSFs.
Severe chronic neutropenia (ie, an ANC < 500 cells/µL) resulting from congenital, cyclic, or idiopathic neutropenia is often associated with recurrent infections. G-CSF is effective in normalizing neutrophil levels and significantly reducing the incidence of infections in > 90% of patients with these conditions.
TOXICITY
G-CSF (filgrastim and pegfilgrastim)
G-CSF has been a remarkably well-tolerated growth factor overall, based on extensive clinical experience with this cytokine over the past decade.
Bone pain The predominant side effect observed with the use of filgrastim and pegfilgrastim is mild to moderate bone pain, which typically occurs in the lower back, pelvis, or sternum in about one-third of patients. Bone pain is usually seen at the initiation of G-CSF therapy or at the very beginning of neutrophil recovery. In randomized studies, no difference in the incidence, severity, or duration of bone pain was noted between filgrastim and pegfilgrastim.
Uncommon side effects Other uncommon side effects include exacerbation of preexisting psoriasis, Sweet’s syndrome (neutrophilic dermatitis), and cutaneous vasculitis. Chronic administration of G-CSF to patients with congenital or idiopathic neutropenia has been associated with splenomegaly.
Laboratory abnormalities observed with the rise in WBC count that occurs during G-CSF administration include elevations in serum lactic dehydrogenase (LDH), uric acid, and alkaline phosphatase levels. Finally, a modest decrease in platelet count without significant clinical sequelae has been reported occasionally with G-CSF use. Antibody formation to either preparation with resultant neutropenia has not been seen in large clinical trials.
GM-CSF
Yeast-derived GM-CSF is generally well tolerated at recommended doses. In the transplant setting, no excessive toxicity is seen in patients treated with this form of GM-CSF, as compared with controls.
Constitutional symptoms In phase I/II trials in other settings, the most commonly reported side effects of GM-CSF have included constitutional symptoms, such as fever, bone pain, myalgia, headaches, and chills. These side effects have been dose- and schedule-dependent and are seen more frequently when GM-CSF is administered at higher doses and by continuous IV infusion than when given at recommended doses by the SC route.
Uncommon side effects Other less frequently observed side effects of GM-CSF include diarrhea, anorexia, facial flushing, dyspnea, and edema. Other side effects that have been reported with Escherichia coli-derived GM-CSF, such as the first-dose phenomenon and capillary leak syndrome, have rarely been observed with sargramostim.
Laboratory abnormalities, such as elevation of LDH, uric acid, and alkaline phosphatase levels; decreases in serum cholesterol and albumin; and occasional thrombocytopenia, have been reported with GM-CSF.
DOSE, ROUTE, AND SCHEDULE OF ADMINISTRATION
Recommended doses The recommended dose of filgrastim (recombinant human G-CSF) is 5 µg/kg/d. This dose is clinically well tolerated and is effective in reducing the duration of neutropenia. The dose should begin 24 hours after chemotherapy and continue until the ANC is > 10,000 cells/µL. However, in clinical practice, dosing is commonly stopped when adequate neutrophil recovery has occurred.
G-CSF is used at a higher dose (10 µg/kg/d) for mobilization of progenitor cells and following BMT. Outside the context of stem-cell mobilization and transplantation, however, there are no data indicating that doses in excess of
5 µg/kg/d are indicated.
Pegfilgrastim is given as a fixed 6-mg dose. This dose has been shown to be effective regardless of age and weight in adults. It is given only once per cycle 24 hours after chemotherapy. For patients who develop febrile neutropenia after administration of pegfilgrastim, further dosing with daily filgrastim is not beneficial and is not recommended.
The recommended dose of sargramostim (yeast-derived GM-CSF) following autologous BMT is 250 µg/m2/d given by a 2-hour IV infusion. In phase I/II studies in the chemotherapy setting, activity has been observed at doses ranging from 250 to 750 µg/m2/d. In patients with MDS, neutrophil responses have been seen at much lower doses (30 to ‰¤ 250 µg/m2/d).
Although recommended doses in patients receiving chemotherapy are 5 µg/kg/d for G-CSF and 250 µg/m2/d for GM-CSF, rounding these doses to the nearest vial size is appropriate for cost savings and convenience. In patients with MDS, the dose can be titrated to the smallest effective level to avoid untoward side effects.
Route of administration The SC route is the preferred route of administering filgrastim, pegfilgrastim, and sargramostim, for convenience. However, IV infusion is an acceptable route for filgrastim and sargramostim, if clinically indicated.
Timing of administration To obtain the greatest benefit from CSFs, the appropriate timing of administration is 24 to 48 hours following the completion of chemotherapy. CSF therapy should be continued until neutrophil recovery is adequate. The discontinuation of CSF therapy after neutrophil recovery is sometimes followed by a decline in ANC, especially in patients with compromised bone marrow reserve. This fall in neutrophil count can be precipitous with G-CSF and appears to be somewhat less pronounced following discontinuation of GM-CSF. Therefore, blood counts should be checked before initiating the next cycle of chemotherapy.
Initiation of the next cycle of chemotherapy is not recommended for at least 24 hours after the completion of CSF therapy because of the potential concern that progenitor cells, which are rapidly dividing following CSF administration, may be sensitized to chemotherapy. Future trials should help to determine the optimal interval that should be allowed between CSF discontinuation and initiation of the next chemotherapy cycle. There remains some theoretic concern that serial exposure of cycling progenitor cells to chemotherapy may accelerate cumulative marrow damage.
Because of the same concern, concurrent administration of CSFs with chemotherapy or radiotherapy is not recommended outside the context of clinical trials. Same-day dosing of pegfilgrastim with chemotherapy has been studied in a variety of tumor types and regimens. To date, these trials have shown that pegfilgrastim is not as effective when administered concurrently with chemotherapy. Therefore, this dosing strategy is not recommended. Trials using GM-CSF concurrently with radiotherapy to the chest area have shown excessive hematologic toxicity, especially thrombocytopenia. It has been speculated that CSF-mobilized progenitor cells in the great vessels may be sensitized to radiation delivered to the chest.
EPO
EPO, an RBC lineage-specific glycoprotein hormone, was the first hematopoietic growth factor to become commercially available for clinical use in the United States. Recombinant human EPO has been approved for the treatment of anemia of chronic renal failure in predialysis or dialysis patients; anemia associated with zidovudine (Retrovir) therapy in patients infected with human immunodeficiency virus (HIV); anemia in cancer patients receiving chemotherapy in nonmyeloid malignancies; and anemia in patients scheduled for elective, noncardiac, nonvascular surgery. (See new safety information box earlier in chapter).
In 2001, darbepoetin alfa was approved by the FDA to allow a new option of treatment of anemia associated with chronic renal failure. Darbepoetin alfa is approved by the FDA for the treatment of chemotherapy-induced anemia in patients with nonmyeloid malignancies. Darbepoetin alfa is a hyperglycosylated molecule based on the protein backbone structure of human EPO. The increased level of glycosylation allows a longer duration of the drug in the circulation after administration (with an up to three times longer half-life than EPO).
CHEMOTHERAPY-INDUCED ANEMIA
The anemia caused by chemotherapy is due mainly to drug effects on bone marrow precursor cells and is proportional to chemotherapy dose intensity. In addition, with platinum agents, anemia may be related to renal effects of these drugs on the production of EPO. Based on these observations, multicenter trials in the United States and Europe have examined the efficacy of recombinant human EPO in correcting the anemia of cancer caused by chemotherapy.
DOSE AND SCHEDULE OF ADMINISTRATION
The original FDA-approved recommended initial dose of EPO in cancer patients is 150 units/kg SC 3 times a week. This dose can be increased to 300 units/kg 3 times weekly if an adequate response (ie, a decrease in transfusion requirements or a rise in hemoglobin value [≥ 1 g/dL]) does not occur after 4 weeks of therapy. However, very few oncologists use the thrice-weekly regimen of EPO dosing anymore. A more common practice, based on data from several clinical trials and the recently FDA-approved dose, is to administer EPO at a dose of 40,000 units SC once weekly, with an increase to 60,000 units once weekly if there is no adequate response after 4 weeks. This dose is well tolerated and appears to be equivalent in clinical effectiveness to three-times-weekly dosing while increasing patient convenience. EPO is approved by the FDA for once-weekly administration in the surgical population. A recent pharmacokinetic/pharmacodynamic study in healthy volunteers demonstrated that once-weekly EPO doses of 600 units/kg resulted in similar increases in hemoglobin value as did 150 units/kg 3 times weekly.
Darbepoetin alfa has a longer half-life than EPO and requires less frequent dosing. The current FDA-approved recommended initial dose of darbepoetin alfa in cancer patients is 2.25 µg/kg SC once a week or 500 µg once every 3 weeks. The weekly dose can be increased to 4.5 µg/kg once a week at 6 weeks if hemoglobin values increase less than 1 g/dL. No dose increase is recommended for the 500-µg-every-3-weeks regimen. Other commonly used dosing regimens of darbepoetin alfa are 200 µg every 2 weeks or 300 µg every 3 weeks, with an increase to 300 µg every 2 weeks at 6 weeks or 500 µg every 3 weeks, respectively, if hemoglobin values increase less than 1 g/dL. Additional dosing schedules have been studied (ie., loading doses, etc.) with both agents.
A patient who does not respond after 8 weeks of therapy (despite a dose increase) is unlikely to respond to higher doses, and erythropoietic therapy should be stopped. The dose of EPO/darbepoetin alfa should be reduced appropriately (25%–40%) if there is a rapid rise in hemoglobin value (ie, > 1 g/dL after 2 weeks) or if hemoglobin values are 12 g/dL or higher and should be titrated to maintain the desired hemogloblin value (10–12 g/dL). In patients treated with 500 µg every 3 weeks, once hemoglobin levels reach 11 g/dL, the dose should be reduced to 300 µg every 3 weeks. If response is suboptimal, the clinician should consider rechecking levels of nutritional cofactors (eg, iron, total iron-binding capacity, ferritin) or evaluate other reasons for lack of response (eg, underlying infection, inflammatory process, occult blood loss, other vitamin deficiencies). Patients (especially premenopausal women) may require supplemental iron to avoid depletion of marginal iron stores and to adequately support erythropoiesis stimulated by EPO. Recent data support the use of intravenous iron products for supplementation, as oral agents are relatively ineffective and often poorly tolerated.
EMERGING SAFETY ISSUES
Recent reports of four new studies in patients with cancer found a higher chance of serious and life-threatening side effects and/or death with the use of erythropoiesis-stimulating agents (ESAs). These research studies evaluated unapproved dosing regimens; a patient population for which ESAs are not approved (patients not receiving concurrent chemotherapy); had target hemoglobin levels up to 15.5 g/dL; or focused on a new, unapproved ESA. Based on these data, the FDA issued a black box warning and updated the package labeling on all ESA products. Further, the prescribing information has been revised to clarify the FDA-approved conditions for use of erythropoiesis-stimulating agents (ESAs) in patients with cancer and revised directions for dosing to state the hemoglobin level (≥ 10 g/dL) at which treatment with an ESA should not be initiated. The new label states that ESAs are not indicated for patients receiving myelosuppressive therapy when the anticipated outcome is cure. In addition, the Center for Medicare Services (CMS) issued further restrictions on the use of these agents in oncology patients with Medicare. For more information and the most up-to-date announcements regarding use of ESAs in patients with cancer, see the box on safety earlier in this chapter and go to
Cytokines with thrombopoietic activity
Although G-CSF and GM-CSF have significantly reduced neutropenia in patients receiving chemotherapy, thrombocytopenia still remains a frequent dose-limiting toxicity of several chemotherapeutic regimens. Several hematopoietic cytokines with thrombopoietic activity have been evaluated in clinical trials. They include IL-1, IL-3, IL-6, IL-11, thrombopoietin (TPO), megakaryocyte growth and development factor (MGDF), and hybrid/synthetic cytokines, such as PIXY321 (a GM-CSF/IL-3 fusion protein) or SC71858 (promegapoietin, a synthetic cytokine comprising mutated versions of IL-3 and TPO).
Most of these cytokines have shown modest thrombopoietic activity and have the potential to induce nonspecific biologic activities, including some undesirable effects. To date, IL-11 is the only thrombopoietic cytokine that has received FDA approval for clinical use.
IL-11
IL-11 is a pleiotropic cytokine with thrombopoietic activity. In vitro, IL-11 acts synergistically with other hematopoietic growth factors, such as TPO, IL-3, and stem-cell factor (c-kit ligand), to promote the proliferation of hematopoietic progenitor cells and to induce maturation of megakaryocytes.
IL-11 was approved by the FDA to prevent severe thrombocytopenia and to reduce the need for platelet transfusions following myelosuppressive chemotherapy in patients with nonmyeloid malignancies who are at risk of severe thrombocytopenia based on the results of a randomized clinical trial of IL-11 in cancer patients who required at least one platelet transfusion after a chemotherapy cycle. In this trial, the use of IL-11 as secondary prophylaxis reduced the need for platelet transfusions in a subsequent cycle of chemotherapy.
However, it should be recognized that severe thrombocytopenia requiring platelet transfusions is an uncommon, acute problem with initiation of standard-dose chemotherapy. Nonetheless, thrombocytopenia can represent a cumulative problem with the many chemotherapeutic regimens often used to treat solid tumors, especially in patients with more heavily pretreated marrows.
Major bleeding is a rare complication related to chemotherapy-induced thrombocytopenia. Therefore, the appropriate use of thrombopoietic agents will require careful attention to several endpoints, including the need for platelet transfusions, ability to deliver chemotherapy without treatment-limiting thrombocytopenia, the safety profile of the thrombopoietic agent, and the associated health care costs.
Dose and schedule of administration The recommended dose of IL-11 for prophylaxis in adults is 50 µg/kg SC once daily. Therapy is started from 6 to 24 hours after the completion of chemotherapy and is continued until the postnadir platelet count is ≥ 50,000 cells/µL. Dosing beyond 21 days per treatment cycle is not recommended.
Adverse reactions Patients treated with IL-11 commonly experience mild to moderate fluid retention, as manifested by peripheral edema and/or dyspnea. In some patients, preexisting pleural effusions have increased during IL-11 administration. Therefore, patients with a history of pleural or pericardial effusions or ascites should be carefully monitored during IL-11 therapy. In addition, fluids and electrolytes should be monitored carefully in patients requiring the use of a diuretic.
Moderate decreases in hemoglobin values (thought to be related to dilutional anemia) have also been observed in patients receiving IL-11. The fluid retention and anemia are reversible within several days after IL-11 is discontinued.
IL-11 should be used with caution in patients with a history of cardiac arrhythmia, since palpitations, tachycardia, and atrial arrhythmia (atrial fibrillation or flutter) have been reported in some patients receiving this agent.
TPO
TPO is a lineage-dominant hematopoietic cytokine that regulates proliferation and maturation of cells of the megakaryocyte/platelet lineage. Preclinical studies have clearly shown that TPO cells are the key regulators of megakaryocyte mass and platelet production. Mice with induced genetic defects in TPO or its receptor, c-mpl, have > 90% loss of platelet production capacity.
The results of initial clinical trials of TPO are encouraging and suggest an important role for this agent in the treatment of cancer patients undergoing myelosuppressive treatment. No recombinant version of TPO has yet been approved by the FDA, showing the difficulty in developing thrombopoietic growth factors.
Development of TPO and related molecules has been complicated by the development of antibodies directed against some-but not all-of the recombinant human versions of this molecule. Clinical development of MGDF, a highly truncated recombinant version of TPO, was halted due to the occurrence of neutralizing antibodies directed against TPO. These potentially dangerous antibodies could prolong thrombocytopenia. However, similar antibodies have not been detected with the full-length version of recombinant human TPO. For that reason, further clinical trials of TPO continue. This promising agent does not produce the edema or other nonspecific side effects that occur with IL-11, and, thus, further data from larger trials of TPO are awaited.
SUGGESTED READING
Auerbach M, Ballard H, Trout JR, et al: Intravenous iron optimizes the response to recombinant human erythropoietin in cancer patients with chemotherapy-related anemia: A multicenter, open-label, randomized trial. J Clin Oncol 22:1301€”1307, 2005.
Bennett CL, Luminari S, Nissenson AR, et al: Pure red-cell aplasia and epoetin therapy. N Engl J Med 351:1403€”1408, 2004.
Citron ML, Berry DA, Cirrincione C, et al: Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: First report of Intergroup Trial C9741/Cancer and Leukemia Group B trial 9741. J Clin Oncol 21:1431–1439, 2003.
Crawford J, Cella D, Cleeland CS, et al: Relationship between changes in hemoglobin level and quality of life during chemotherapy in anemic cancer patients receiving epoetin alfa therapy. Cancer 95:888–895, 2002.
Holmes FA, O’Shaughnessy JA, Vukelja S, et al: Blinded, randomized, multicenter study to evaluate single administration pegfilgrastim once per cycle versus daily filgrastim as an adjunct to chemotherapy in patients with high-risk stage II or stage III/IV breast cancer. J Clin Oncol 20:727–731, 2002.
Kuderer NM, Dale DC, Crawford J, et al: Impact of primary prophylaxis with granulocyte colony-stimulating factor on febrile neutropenia and mortality in adult cancer patients receiving chemotherapy: A systematic review. J Clin Oncol 25:3158–3167, 2007.
Rossert J, Casadevall N, Eckardt KU: Anti-erythropoietin antibodies and pure red cell aplasia. J Am Soc Nephrol 15:398€”406, 2004.
Smith TJ, Khatcheressian J, Lyman GH, et al: 2006 update of recommendations for the use of white blood cell growth factors: An evidence-based clinical practice guideline. J Clin Oncol 24:3187–3205, 2006.
Vogel CL, Wojtukiewicz MZ, Carroll RR, et al: First and subsequent cycle use of pegfilgrastim prevents febrile neutropenia in patients with breast cancer: A multicenter, double-blind, placebo-controlled phase III study. J Clin Oncol 23:1178–1184, 2005.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.