HER2+ mBC With CNS Disease: Sequencing Therapy After Progression on Tucatinib
Panelists reflect on sequencing therapy for HER2+ metastatic breast cancer following disease progression on the tucatinib, trastuzumab and capecitabine regimen.
Episodes in this series
Transcript:
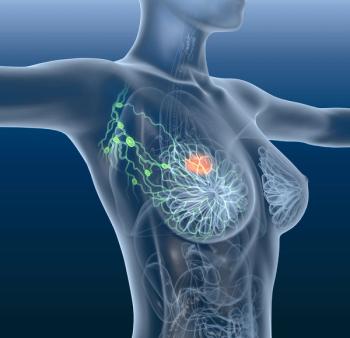
Sara Tolaney, MD:In this case, when the patient presented with the brain metastases and we decided that we wanted to use a systemic approach, we used HER2CLIMB. Sarah, if you were thinking about this and you were trying to decide between the HER2CLIMB regimen or trastuzumab deruxtecan, how would you make a decision? Would you prioritize 1 over the other in a case like this?
Sarah Sammons, MD: That’s a good question. That’s what everybody wants to know. Who are we placing in the second line? For me, in a patient with brain metastases, it’s important to consider if they’re active or stable. Stable means that they’ve undergone local therapy with radiation and resection. We’ve done an interval MRI, and the brain metastases are stable or there are no distant brain metastases. In a stable patient with brain metastases who’s in the second line and progressing extra cranially, I’ll give them T-DXd [trastuzumab deruxtecan]. For a patient with active brain metastases, this means that your patient who had a pretty high number of brain metastases was trying to avoid having the whole brain untreated. Untreated equals active to me, so it’s treated but progressive. They’ve maybe had SRS [stereotactic radiosurgery] or whole-brain treatment, yet their brain metastases continue to grow. You phone a friend, and they don’t think it’s radiation necrosis. They think it’s true progression in the brain, which is active to me. In that patient population, I’d choose HER2CLIMB.
Sara Tolaney, MD:That’s a good way to think about it. As this patient went on to HER2CLIMB, what happens if they progress? What do you think about? Nancy, the challenge is that it depends on where they progressed. Did they progress in the brain, or did they progress in the body? Take us through those scenarios and what you’d do in those cases.
Nancy Lin, MD: If the patient progresses in the body—let’s say the brain is stable and they are on tucatinib but haven’t received trastuzumab deruxtecan—I’d generally sequence to that next because the data are very strong for extracranial disease control with trastuzumab deruxtecan. The emerging data explain the role of trastuzumab deruxtecan in patients with progressive or active brain metastases. There are now some data. The original data came out of the DESTINY-Breast03 and DESTINY-Breast01 studies, which did report out CNS [central nervous system] responses and PFS [progression-free survival] overall in patients with stable, treated brain metastases at study entry. There were responses, but it’s hard to interpret them because there’s no information about when the last CNS-directed radiation was. That could be what’s causing a response. There’s no information about the status of the brain metastases other than just knowing the eligibility. You don’t know what the trajectory was beforehand. There are a lot of issues with interpretation of the data because of the eligibility.
There have been a couple of small prospective experiences. One was presented by Rupert Bartsch, called the TUXEDO-1 trial. It was 15 patients with small experience, but the response rate intracranially was around 73%. It was a very high response rate. The DEBBRAH investigators also had a HER2 [human epidermal growth factor receptor 2]–positive active brain metastases cohort in their series, which has multiple cohorts, but the 1 that’s been reported out so far is HER2+. Their response rates were in the mid-40% range, but it’s a very small number of patients. At Dana-Farber [Cancer Institute], Duke [University], and [The University of Texas] MD Anderson [Cancer Center], we also published a case series with a response rate in excess of 70% intracranially. Collectively, the data suggest that T-DXd [trastuzumab deruxtecan] has intracranial activity. Even though the number of patients who we have data for is relatively small, still it’s hard to believe that through chance alone we’ll see response rates of that magnitude. I think it’s going to be an active drug.
Sara Tolaney, MD:That’s great.
Transcript edited for clarity.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.