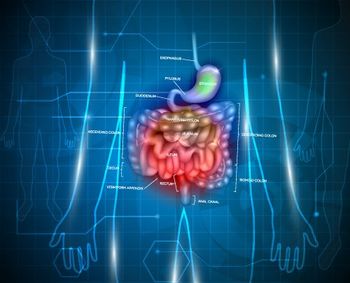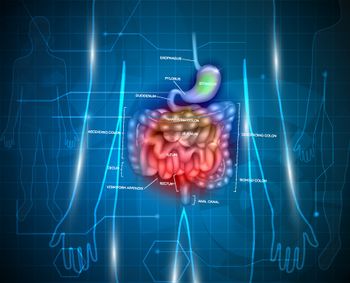
How Does Prognosis of NETs Differ Based on Site of Origin?
An analysis of more than 70,000 patients revealed significant differences with regard to survival between different sites of origin for neuroendocrine tumors.
An analysis of more than 70,000 patients revealed significant differences with regard to survival between different sites of origin for neuroendocrine tumors (NETs). These differences could help guide therapy in these malignancies.
“Despite 100 years of clinical studies, NETs remain poorly understood because of their rarity, tumor heterogeneity, nonspecific presentation, unique indolent biology, and a lack of awareness,” wrote study authors led by Da Man, MD, of Hangzhou Hospital in China. Recent research has found increasing incidence of these tumors, but the clinical characteristics and prognosis remain poorly understood.
Researchers used the Surveillance, Epidemiology, and End Results (SEER) database to examine prognostic factors for survival among NETs patients. They included a total of 73,782 patients diagnosed between 1973 and 2014, and the results were
Patients ranged in age from 18 to 100 years, and the median age in the cohort was 61.6 years. Slightly more than half the cohort was female (52.7%), and the bulk of those included were diagnosed between 2001 and 2014 (76.7%).
The median survival for the entire group was 41 months. The 1-year survival rate was 72.8%; at 3, 5, and 10 years, these rates were 52.7%, 39.4%, and 18.1%, respectively.
Survival rates were significantly different depending on primary tumor site (P < .001). For example, the median survival of those with colon NETs was 41 months, compared with 25 months for those originating in the lung and bronchus, 51 months for small intestine NETs, 41 months for stomach NETs, and 70 months for those originating in the rectum. The shortest median survival, at 22 months, was seen in pancreatic NETs.
The highest 1-year survival rate was seen in rectal NETs (86.5%), while the lowest was in lung and bronchus tumors (63.9%). At 5 years, rectal NETs remained highest, at 55.7%, while pancreatic NETs fared poorest, at 22.7%. Only 7.3% of patients with pancreatic NETs were alive at 10 years, compared with 20.5% of those with colon NETs and 27.1% of those with rectal NETs.
A multivariate analysis confirmed the importance of primary site on survival. After adjustments for several prognostic factors, NETs in the rectum had the best prognosis; using those tumors as a reference, the hazard ratio (HR) for overall survival for colon NETs was 1.896 (95% CI, 1.799–1.999; P < .001). For small intestine NETs, that HR was 1.660 (95% CI, 1.579–1.744; P < .001), while for pancreatic NETs the HR was 2.034 (95% CI, 1.925–2.148; P < .001).
A further analysis showed that women had higher mortality risk than men for all origin sites other than lung/bronchus, and that American Indians/Alaskan natives and Asian/Pacific Islands had significantly worse prognosis for all origin sites other than the colon. “Primary tumor sites might be one of the most useful predictors of outcome in patients with NETs,” the authors concluded.
Andrew E. Hendifar, MD, MPH, an expert on NETs at Cedars-Sinai Medical Center in Los Angeles, who was not involved with the new research, pointed out that other factors should still be considered when attempting to determine prognosis. “NETs need to be understood by grade and differentiation, as these characteristics can be just as important as site of origin,” he told Cancer Network.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.