Oncology NEWS International
- Oncology NEWS International Vol 10 No 1
- Volume 10
- Issue 1
Letrozole Superior to Tamoxifen in 2 Studies
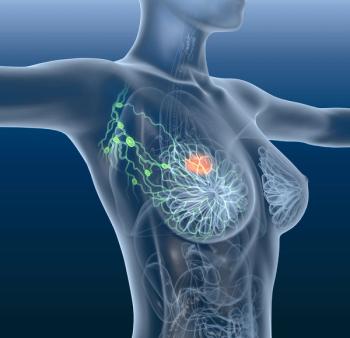
NEW YORK-Letrozole (Femara) was found to be superior to tamoxifen (Nolvadex) in the largest study ever conducted of endocrine therapy in advanced breast cancer, Matthew J. Ellis, MD, PhD, clinical director of the Duke University Breast Cancer Program, said at the XVIII Chemotherapy Foundation Symposium. Median time to progression was 41 weeks for letrozole vs 26 weeks for tamoxifen (P = .0001), he said.
NEW YORKLetrozole (Femara) was found to be superior to tamoxifen (Nolvadex) in the largest study ever conducted of endocrine therapy in advanced breast cancer, Matthew J. Ellis, MD, PhD, clinical director of the Duke University Breast Cancer Program, said at the XVIII Chemotherapy Foundation Symposium. Median time to progression was 41 weeks for letrozole vs 26 weeks for tamoxifen (P = .0001), he said.
The study was the basis for the FDA’s Oncologic Drugs Advisory Committee’s recommendation that the agency approve the supplemental new drug application for letrozole’s use as first-line therapy in postmenopausal women with advanced breast cancer (see article above for details of the study).
The study addressed a number of points that have been at issue in endocrine therapy studies, Dr. Ellis said. Among them is the question of the best way to treat women who relapse after receiving tamoxifen in the adjuvant setting. Is it better to reintroduce tamoxifen in those patients or to use letrozole?
Patients in the study who had received prior adjuvant tam-oxifen and then received letrozole had a response rate of 30%, very similar to those who had never received tamoxifen, whereas those in whom tamoxifen was reintroduced after a relapse showed an extremely low response rate of about 8%.
"For me, this solves the mystery. Should you reintroduce tamoxifen after prior adjuvant use? The answer is: No, you should use an aromatase inhibitor," he said.
Dr. Ellis explained the rationale behind the trial. "We have known for a very long time that reducing estrogen levels in women with premenopausal breast cancer results in gains in survival," he said. After menopause, however, extra-ovarian synthesis of estrogen still takes place, driven by the enzyme aromatase, in the skin and adipose tissue, the breast itself, the brain, and other parts of body.
Tamoxifen targets postmenopausal estrogen by attempting to block it at the tumor receptor, but that does not always work, Dr. Ellis said.
Many breast cancers are unresponsive to tamoxifen’s action, despite tumor estrogen-receptor (ER) expression, he said. In addition, tamoxifen paradoxically stimulates estrogen receptors in the endometrium and circulation, increasing the risk of endometrial cancer and venous thrombosis.
Selective aromatase inhibitors (SAIs) such as letrozole, he said, block estrogen synthesis throughout the body by interfering with the P450 enzyme pathway and thus preventing peripheral conversion of adrenal androgens to estrogens.
"Every indication for tamoxifen will be challenged by letrozole," Dr. Ellis said. He noted that this line of inquiry has "huge" implications. "For years we had only one drug that workedtamoxifen." he said. "This trial shows that letrozole is superior to tamoxifen for first-line therapy of advanced disease in postmenopausal breast cancer. Now, we really have a chance to learn the best way to treat this disease in other settings as well."
In a 1-year multicenter trial comparing letrozole and tamoxifen as preoperative treatment in postmenopausal women with untreated primary breast cancer, letrozole showed a superior clinical response and increased the odds by more than 70% that breast-conserving surgery could be performed, compared with tamoxifen, Dr. Ellis reported.
This study, he said "supports the idea that letrozole is significantly more active than tamoxifen in this completely treatment-naïve population."
In the phase IIb/III trial, 337 women were randomized to either 2.5 mg letrozole or 20 mg tamoxifen daily for 4 months prior to surgery. According to study criteria, all subjects were postmenopausal with ER-positive and/or proges-terone-receptor-positive primary invasive tumors.
All tumors were unilateral and ineligible at baseline for breast-conserving surgery, with stages ranging from T2 to T4A, B, or C, but excluding inflammatory carcinoma. Nodes were 0, 1, or 2, and there were no distant metastases. There could be no prior endocrine therapy for the disease.
Significantly more women in the letrozole arm had a clinical response than women in the tamoxifen arm: 55% vs 36% (P < .001). Particularly intriguing, Dr. Ellis said, was the finding that 45% of subjects were eligible for breast-conserving surgery after 4 months on letrozole, compared with only 35% of those in the tamoxifen arm (P = .02).
Women with T2 tumors treated with letrozole had the highest rate of breast-conserving surgery: 61%. "It is really quite remarkable and bears further confirmation," he said.
Articles in this issue
about 25 years ago
ODAC Recommends Campath for FDA Approval for Refractory CLLabout 25 years ago
‘IrinoGem’ Active and Well Tolerated in Pancreatic Cancerabout 25 years ago
STI571 Studies Help Validate Molecular Targeting in CMLabout 25 years ago
Outpatient Mylotarg Therapy Cuts Costs in Relapsed AMLabout 25 years ago
STI571 Proves Effective in Patients With Interferon-Failure CMLabout 25 years ago
Prostate Cancer Patients Tolerate Higher 3D Conformal RT Dosesabout 25 years ago
IP6 (Phytic Acid) Inhibits Breast Cancer in Animalsabout 25 years ago
Adjuvant Therapy Beneficial in Early, Node-Negative Breast Cancerabout 25 years ago
Medicare Increases Payment Rates for Most Physiciansabout 25 years ago
Update on High-Dose Consolidation Therapy in Breast CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.