Myeloproliferative Neoplasms Increased Overall Mortality
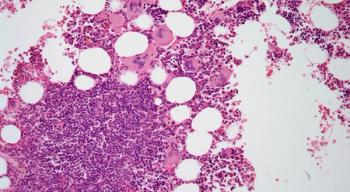
A study found that patients with myeloproliferative neoplasms have a higher overall mortality rate due to death from hematologic malignancies and infections.
Patients with myeloproliferative neoplasms (MPNs) have a higher overall mortality rate than matched control patients, and this risk is driven primarily by death due to hematologic malignancies and infections, according to the results of a study
“Our results underline the demand for disease modifying treatments as well as improved prevention of thromboembolic and infectious complications in patients with MPN, something that it is hoped can be achieved with the emerging tailored treatments,” wrote study author Malin Hultcrantz, MD, of the Karolinska University Hospital in Solna, Sweden, and colleagues.
Using Swedish registries, Hultcrantz and colleagues identified 9,285 patients with MPN and 35,769 matched control patients and compared outcomes between the two groups.
They found that the cause-specific mortality rate for patients with MPN was higher than in the matched controls for most causes of death and in most age groups. This increased risk for mortality was driven primarily by increased death from hematologic malignancies (hazard ratio [HR] = 92.8; 95% confidence interval [CI], 70.0–123.1) and infections (HR = 2.7; 95% CI, 2.4–3.1) for patients with MPNs compared with the control patients.
Looking at outcomes by age groups, the researchers found that patients aged 70 to 79 years with MPNs had increased risk for death from cardiovascular disease (HR = 1.5; 95% CI, 1.4–1.7), cerebrovascular disease (HR = 1.5; 95% CI, 1.3–1.8), solid tumor (HR = 1.2; 95% CI, 1.0–1.3), and other disorders compared with control patients. In younger patients, MPNs conferred higher relative risk for dying from vascular diseases. Specifically, for patients aged 50 to 59 years, the HR for death from cardiovascular disease was 2.2 (95% CI, 1.6–3.1), and 5.1 (95% CI, 2.8–9.4) from cerebrovascular disease, compared with the control patients.
To calculate the cumulative incidence, the researchers used data from the largest patient group: men diagnosed with MPN between age 70 and 79 from 1993 to 2000.
“These patients had an overall 10-year probability of death of 75.0% compared with 49.0% in matched controls,” the researchers wrote. “The 10-year probabilities of death were higher in patients with MPN versus matched controls for infections (4.6% vs 2.3%), hematologic malignancies (13.6% vs 0.2%), and other disorders (24.9% vs 14.8%).”
However, the researchers found that after adjustment for competing risks, there was no large difference between patients and controls in the 10-year probabilities of dying from cardiovascular diseases (16.8% vs 15.2%), cerebrovascular diseases (5.6% vs 5.2%), or solid tumors (9.7% vs 11.4%). Patients aged 50 to 59 years with MPNs had an elevated 10-year probability of death from cardiovascular disease (4.2% vs 2.1%) and cerebrovascular disease (1.9% vs 0.4%).
“Advances in MPN treatment, such as prophylactic low-dose aspirin and more stringent criteria for phlebotomy, has most likely contributed to the improved survival in patients with MPN,” the researchers wrote. “In addition, general improvements-for example, reduced smoking rates, more optimal treatment of hyperlipidemia, and better acute management of vascular events-have contributed to decreased mortality from cardiovascular disease in both patients with MPN and in controls.”
However, the researchers added, “The higher cardiovascular death rate in young patients with MPN compared with controls is an important finding that needs further assessment.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.