Oncology NEWS International
- Oncology NEWS International Vol 15 No 10
- Volume 15
- Issue 10
Noxafil Approved for Prevention of Aspergillus Infection
The US Food and Drug Administration (FDA) has approved Schering-Plough Corporation's Noxafil (posaconazole) Oral Suspension for the prevention of invasive Aspergillus and Candida infections in patients age 13 years and older at high risk of developing these infections.
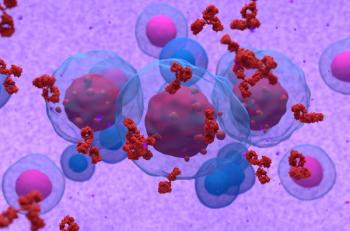
ROCKVILLE, MarylandThe US Food and Drug Administration (FDA) has approved Schering-Plough Corporation's Noxafil (posaconazole) Oral Suspension for the prevention of invasive Aspergillus and Candida infections in patients age 13 years and older at high risk of developing these infections. High-risk patients include hematopoietic stem cell transplant recipients with graft-versus-host disease (GVHD) or those with hematologic malignancies with prolonged neutropenia from chemotherapy.
Noxafil, a novel triazole antifungal agent discovered and developed at Schering-Plough Research Institute, is the first and only antifungal agent approved by FDA for prevention of invasive fungal infections (IFIs) caused by Aspergillus species, the company said.
Invasive fungal infections are the leading cause of death among hematopoietic stem cell transplant recipients. In the United States, each year more than 1.3 million hospital patients are affected by IFIs. Currently, if these populations develop such an infection, the mortality rate varies between 60% and 90%.
"Noxafil can help prevent patients from developing life-threatening invasive fungal infections while being treated for serious conditions such as acute leukemia or GVHD," said John Perfect, MD, professor of medicine, Division of Infectious Diseases, Duke University, and director, Duke University Mycology Research Unit. "With this FDA approval, Noxafil offers physicians an important new therapeutic option for preventing invasive fungal infections in patients at high risk," he said.
Clinical Trials
The safety and efficacy of Noxafil were evaluated in clinical trials consisting of 1,844 patients between 13 and 82 years of age, according to the FDA. In two randomized controlled studies of patients who had compromised immunity and were at high risk for invasive fungal infections, those patients who received Noxafil had comparable or lower rates of invasive Aspergillus and Candida infections than those patients who received other antifungal medications.
Open-Label Study
An open-label study compared Noxafil oral suspension 200 mg three times daily (n = 304) to pooled standard azole therapies (fluconazole oral suspension 400 mg once daily or itraconazole oral solution 200 mg twice daily) (n = 298), as prophylaxis against IFIs in neutropenic patients who were receiving cytotoxic chemotherapy for acute myelogenous leukemia (AML) or myelodysplastic syndrome (MDS). The study assessed all patients while on therapy plus 7 days and at 100 days postrandomization. Efficacy of prophylaxis was evaluated using a composite endpoint of proven/probable IFIs, death, or treatment with systemic antifungal therapy. Patients may have met more than one of these criteria.
In this study, Noxafil reduced treatment failure (as defined by breakthrough IFIs, death, and use of systemic antifungal therapy), compared with the comparator group (27% vs 42%); reduced proven and probable IFIs vs fluconazole/itraconazole (2% vs 8%); reduced breakthrough Aspergillus infections vs fluconazole/itraconazole (1% vs 7%) (aspergillosis was the most common breakthrough infection seen in the study); decreased all-cause mortality at 100 days postrandomization (14% vs 21%); and had safety and tolerability comparable to that of fluconazole.
Double-Blind Study
A double-blind study compared Noxafil oral suspension 200 mg three times daily (n = 301) to fluconazole capsules 400 mg once daily (n = 299) as prophylaxis against IFIs in allogeneic hematopoietic stem cell transplant recipients with GVHD. The study assessed all patients while on therapy plus 7 days and at 16 weeks postrandomization. Efficacy of prophylaxis was evaluated using a composite endpoint of proven/probable IFIs, death, or treatment with systemic antifungal therapy. Patients may have met more than one of these criteria.
In this study, Noxafil demonstrated a reduction in proven/probable IFIs at 16 weeks, compared to fluconazole (5% vs 9%); a reduction in breakthrough Aspergillus infections at 16 weeks, compared to fluconazole (2% vs 7%); decreased IFI-related mortality at 16 weeks (3% vs 5%); and safety and tolerability comparable to that of fluconazole.
Safety Profile
Clinical studies have demonstrated that Noxafil is generally safe and well tolerated, the company said. The most common side effects in patients receiving Noxafil were nausea, vomiting, diarrhea, rash, a decrease in potassium blood levels and platelet counts, and abnormalities in liver function tests. Rare adverse events possibly related to the drug include QTc prolongation and liver function impairment. Liver function tests should be monitored at the start of and during the course of therapy.
Noxafil must be taken with a full meal or nutritional supplement to allow adequate absorption into the body, according to the FDA.
Noxafil has been shown to interact with several medications, including drugs that suppress the immune system, and these reactions may be serious. The product label should be consulted when other drugs are being prescribed along with Noxafil.
Articles in this issue
over 19 years ago
Recombinant MAGE-A3 Cancer Immunotherapy Promisingover 19 years ago
WHI Calcium/Vit D Trial:over 19 years ago
Negative Lymph Nodes Predict Survival in Stage III Colon Caover 19 years ago
Oophorectomy Value Varies by BRCA Typeover 19 years ago
FDA Approves Vectibix for Metastatic Colon Caover 19 years ago
Brain Cancer Cells Attract Stem Cells for Angiogenesisover 19 years ago
NCCN Presents Hematologic Ca Congressover 19 years ago
Interim Results for MediGene's Oncolytic Virus NV1020over 19 years ago
GSK Files NDA for Tykerb for Advanced Breast Cancer RxNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.