- Oncology Vol 31 No 10
- Volume 31
- Issue 10
Pancreatic Neuroendocrine Tumors: State-of-the-Art Diagnosis and Management
In this review, we focus on the treatment of well-differentiated early and metastatic PNETs, emphasizing current controversies, recent advances in therapy, and the multidisciplinary approach required for optimal treatment.
The incidence of pancreatic neuroendocrine tumors (PNETs) has significantly increased in recent years, although this may reflect better detection and improved diagnosis, in addition to a true increase in incidence. The majority of PNETs are nonfunctional; up to half of nonmetastatic PNETs will present incidentally, and 85% will develop metastases over their lifetime. Treatment of PNETs is largely dictated by their heterogeneous nature and usually indolent behavior. Surgery is a mainstay of treatment, both in early PNETs and in metastatic disease. In this review, we focus on the treatment of well-differentiated early and metastatic PNETs, emphasizing current controversies, recent advances in therapy, and the multidisciplinary approach required for optimal treatment.
Introduction
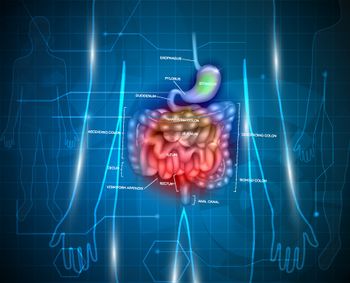
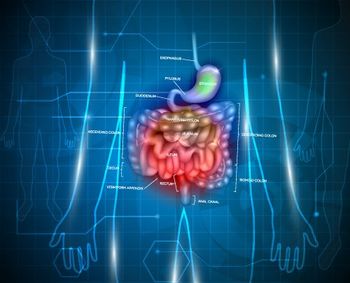
Neuroendocrine tumors (NETs) are widely distributed neoplasms described as epithelial tumors with predominantly neuroendocrine differentiation that share a common phenotype. Regardless of primary site, these tumors have a propensity to metastasize to the liver, albeit at varying rates. Historically, classification of NETs has focused more on the differences between the tumors at different sites, with names often designating the tissue of origin, such as “pancreatic islet cell” and “carcinoid” tumors. More recent classification systems, such as the World Health Organization (WHO) 2010 classification, have emphasized the greater importance of grade and differentiation with regard to prognosis, as compared with tumor location. Although there is no single classification system that includes all the various primary sites, the changes in classification reflect the general consensus that the prognosis of gastroenteropancreatic (GEP) neuroendocrine neoplasms depends more on grade and differentiation than on site. In this review, we will focus on well-differentiated nonfunctional pancreatic neuroendocrine tumors (PNETs), while mentioning the various functional tumors.
Epidemiology
The incidence of all NETs has increased substantially, from an annual rate of 1.1 per 100,000 people in 1973 to 5.8 per 100,000 in 2008.[1,2] In our own analysis, which we performed using Yao’s method and data through 2012, the incidence appears to now approach 7 cases per 100,000 people. This increase likely reflects improved imaging and pathologic techniques as much as a true surge in the incidence of disease.
PNETs have similarly increased-to a rate of nearly 1 per 100,000 (Figure 1). PNETs make up only 7% of GEP NETs and 2% of pancreatic neoplasms.[1,3] However, PNETs account for a disproportionate number of neuroendocrine liver metastases, which are seen on presentation in an estimated 60% of patients with PNETs, compared with 27% of all patients with GEP NETs-and the lifelong incidence of liver metastases in patients with PNETs is as high as 85%.[1,2,4,5]
Several genetic syndromes are associated with NETs, including multiple endocrine neoplasia type 1 (MEN1), von Hippel–Lindau disease, neurofibromatosis type 1, and tuberous sclerosis; however, the majority of PNETs are sporadic. NETs occur in 80% to 100% of patients with MEN1, in up to 20% of patients with von Hippel–Lindau disease, in 10% of patients with neurofibromatosis type 1, and in 1% of patients with tuberous sclerosis.[6] PNETs associated with MEN1 are often functional-for example, insulinomas and gastrinomas. Other than the rare genetic endocrinopathy, no specific recognizable cause of PNETs has been clearly identified. Less common factors associated with these tumors include smoking, diabetes, and a history of chronic pancreatitis.
Presentation
NETs are often asymptomatic and are discovered incidentally. Incidentally discovered pancreatic masses now account for up to half of nonmetastatic PNETs.[7,8] The most common complaints associated with symptomatic nonfunctional PNETs include abdominal pain, weight loss, anorexia, and nausea. Less frequent complaints include jaundice, hemorrhage from tumors, and a palpable mass. Symptoms often do not appear until metastases develop.
PNETs may also present with symptoms from one of the several syndromes with which they may be associated. A synoptic description of the symptoms associated with functional syndromes is presented in Table 1. It is important to note that 70% to 90% of patients will present with nonfunctional PNETs.[9,10]
Workup
The workup of an incidental pancreatic mass or of symptoms consistent with a PNET is focused on arriving at a diagnosis, determining functionality, and delineating extent of disease. These goals are accomplished by means of cross-sectional imaging; functional imaging; invasive imaging, such as endoscopic ultrasound (EUS) or arterial stimulation venous sampling (for functional PNETs); and measurement of tumor markers.
Cross-sectional imaging
In the workup of PNETs, cross-sectional imaging plays a major role in characterizing the primary tumor and determining the extent of disease. The sensitivity of CT and MRI for the detection of PNETs exceeds 80%, and both modalities are more sensitive than an octreotide-based scintigraphic study.[11,12] Radiologic findings suggestive of a PNET include arterial enhancement, calcifications, and occasionally necrosis or cystic degeneration.[13] In general, CT or MRI can be used interchangeably, depending on institutional preferences.
EUS
EUS is an invaluable adjunct to CT or MRI and has superior resolution. The sensitivity of EUS alone may exceed 90%, with tumor resolution as small as 2 mm; its sensitivity approaches 100% when combined with cross-sectional imaging.[11,14] EUS is recommended when a biopsy is needed to proceed with treatment, when cross-sectional imaging does not define the pancreatic mass, or when location of the primary tumor is in question.
Functional imaging
Functional imaging in NETs takes advantage of high levels of somatostatin receptor 2 (SSTR2) expression. It is less useful for insulinomas and poorly differentiated tumors because they often lack SSTR2.[15,16] Functional imaging can often detect primary tumors or metastatic disease not seen on cross-sectional imaging. In addition, uptake can predict response to octreotide analogs.[17] Octreotide-based imaging is most beneficial at diagnosis and is used less frequently in surveillance.
Indium-111 (111In) pentetreotide scan (Octreoscan™) is a readily available nuclear scan that is effective at identifying nonfunctional PNETs, glucagonomas, and gastrinomas.[18] Functional imaging has significantly improved with the recent US Food and Drug Administration (FDA) approval of gallium-68 (68Ga) DOTATATE.[19] High-resolution positron emission tomography (PET) in combination with CT makes this imaging modality superior to 111In pentetreotide at detecting small tumors and identifying occult metastases.[20] 68Ga DOTATATE PET/CT has a sensitivity ranging from 86% to 100% and a specificity of 79% to 100%[21-23]; what it reveals can change treatment in 20% to 55% of cases, leading to either more invasive or less invasive interventions.[23] However, wide adoption is precluded by limited availability and high costs.
Tumor markers
In NETs, tumor markers are useful for diagnosis, but they often play a more important role in prognostication, assessment of response to treatment, and detection of recurrence. Whereas functional PNETs can be followed with their respective secretagogues (see Table 1), as clinically indicated, nonspecific NET tumor markers, such as chromogranin A (CgA), 5-hydroxyindoleacetic acid (5-HIAA), and pancreatic polypeptide (PP), are useful in patients with nonfunctioning NETs. It is our practice to order measurements of functional markers, as well as CgA and PP, at diagnosis and to follow whichever marker is elevated. PP is less sensitive than CgA, and 5-HIAA is more useful in patients with carcinoid syndrome resulting from small bowel NETs.[24] Given the lower utility of PP and 5-HIAA in PNETs, CgA only will be discussed in this review.
CgA is a secretory protein found in NET cells. The sensitivity and specificity of CgA in NETs are 73% and 95%, respectively.[25] CgA is less sensitive in PNETs but still clinically useful. Elevated levels of CgA can be associated with advanced disease and predict shorter survival.[26] CgA may be artificially low when patients are receiving somatostatin analog treatment or artificially elevated when they are receiving proton pump inhibitors or have renal failure.[27] In cases of aberrant CgA levels, testing may be repeated with short-term follow-up.
Surveillance
CT and MRI, in combination with tumor markers, are the preferred modalities for surveillance and monitoring progression. Unfortunately, Response Evaluation Criteria in Solid Tumors (RECIST) may not be reliable in NETs, since tumor shrinkage is not a reliable marker of response in these patients.[28,29] In functional PNETs, the relevant functional marker is followed (see Table 1), whereas CgA or whichever tumor marker is elevated is followed in nonfunctional PNETs. Functional imaging may help to confirm recurrences observed on CT or MRI.
Staging and Classification
Multiple classification and grading systems have been proposed over the last few decades in an effort to better categorize NETs according to their clinical behavior; these have emphasized grade and differentiation. The older systems have been refined into the current grading classifications (Table 2) and TNM staging systems, including those adapted by the European Neuroendocrine Tumor Society (ENETS) in 2006, by the American Joint Committee on Cancer (AJCC) in 2009, and by WHO in 2010.
Although there has been significant progress in refining NET staging, the current systems are not perfect. Several authors have questioned whether poorly differentiated neuroendocrine carcinomas (NECs) and high-grade tumors are equivalent.[30] Using the current staging system, a subset of patients may be classed as grade 2 on the basis of mitotic rate but have a high proliferation rate ( Ki-67 index ≥ 20%), typically associated with grade 3 disease; the behavior of such grade-discordant tumors is not well understood. For the most part, discordant tumors fall into a gray zone for which there are few data regarding treatment, with additional research needed to clarify optimal therapy.[31]
Patients with poorly differentiated tumors (grade 3) may be further stratified on the basis of whether their Ki-67 index is between 20% and 55% or is > 55%. Patients with a Ki-67 index > 55% have a worse prognosis but respond to cisplatin-based chemotherapy for a longer period.[32] Future staging strategies may need to account for heterogeneity in poorly differentiated NECs.
Treatment
The only known cure for functional or nonfunctional PNETs is surgical resection. Unfortunately, most patients present with or develop advanced disease, for which the goal of treatment is often longevity with quality of life. Tumor functionality, grade, and stage are factors that help determine which of the various treatment options may be considered in patients with PNETs (Figure 2). Several treatment options exist for advanced PNETs, although the optimal sequence of therapies has not been well established. At times, observation may be prudent. Treatment of patients with advanced disease is usually multimodal. Details regarding the treatment of poorly differentiated NEC will not be discussed here, except to say that chemotherapy is the mainstay of treatment, and that surgery is rarely indicated in these patients.
Nonmetastatic PNETs
Surgical resection is the gold standard for all locoregional PNETs ≥ 2 cm.[33] Even when major vascular construction is needed, surgical resection may often cure or prolong survival in patients with PNETs.[34] For small tumors (< 2 cm), treatment remains controversial and includes formal oncologic resection, enucleation, or observation, depending on patient factors, location, grade, functionality, and risk of disease dissemination.
Oncologic resection. An oncologic resection is necessary for PNETs ≥ 2 cm and includes pancreaticoduodenectomy or distal pancreatectomy with or without splenectomy. Central pancreatectomy is not an ideal operation for PNETs, since the lymphatic drainage typically favors either the pancreatic head or tail.
For lesions < 2 cm, the risk of positive lymph nodes or disease dissemination remains an argument for an oncologic resection. Patients with positive lymph nodes do worse than those with negative nodes, with some studies suggesting a significant 10-year difference in median survival (4.6 vs 14.6 years, respectively),[35] although this discrepancy remains controversial. While small (< 1.5–2 cm) PNETs may have positive lymph nodes at a rate of 12% to 13%,[35,36] some population-based studies have questioned the prognostic value of lymphadenopathy.[37] Preoperative risk evaluation of lymph nodes is often unreliable and correlates poorly with tumor size[38,39]; therefore, factors associated with lymph node positivity, such as tumor location (head), high Ki-67 index, and lymphovascular invasion, should be considered in surgical planning.[35]
Enucleation. A patient is an ideal candidate for enucleation when the pancreatic duct is not in close proximity to the tumor. In patients with functional PNETs that have low malignant risk, such as insulinomas or gastrinomas, enucleation is a treatment option when deemed surgically appropriate.[33] In properly selected patients with small (< 2 cm) PNETs, risk of recurrence is low and oncologic outcomes are acceptable.[37,40] When possible, lymphadenectomy should be performed in patients undergoing enucleation for nonfunctional PNETs.
Observation. Studies comparing observation with surgical resection are difficult because of the indolent nature of PNETs. Retrospective studies are limited by selection bias and short follow-up. With these limitations in mind, it is fair to say that observation of patients with small PNETs does not lead to more recurrences.[41,42] Observation should be considered in patients with a low risk of disease dissemination who are at higher risk of dying from competing causes or whose risk from surgery outweighs the risk of disease progression.
Metastatic PNETs
PNETs most often spread to the liver, and disease recurs in the majority of patients even with complete resection. Therefore, treatment is often directed at slowing progression and minimizing symptoms. Liver treatment depends on the status of the primary tumor, the presence of extrahepatic disease, and the volume of liver disease. A combination of surgery, radiologic interventions, and systemic therapies can often alleviate symptoms and extend survival for several years (Figure 3).
Primary tumor resection. Primary tumor resection combined with neuroendocrine liver metastasectomy improves survival and symptomatology.[43,44] The role of primary tumor resection in patients with unresectable neuroendocrine liver metastases is less clear, and randomized trials are needed to evaluate the role of primary tumor resection in this setting.
While primary tumor resection for small bowel NETs with unresectable metastases may prevent mesenteric fibrosis, bowel obstruction, and malnutrition,[45] primary tumor resection for PNETs with unresectable metastases is more controversial. Overwhelmingly, retrospective studies support primary tumor resection (Table 3), although there is no way to eliminate selection bias from these studies. The median survival in patients undergoing primary tumor resection ranges from 36 to 111 months compared with 12 to 52 months without primary tumor resection.[46-50] There appears to be a benefit from primary tumor resection whether or not liver disease is treated.[46] It may be hypothesized that even nonfunctional PNETs secrete active agents, and that primary tumor resection decreases local symptoms while preventing further spread of tumor. Primary tumor resection should be considered even in patients with unresectable metastases when surgical morbidity is considered low in experienced hands.
Despite the potential benefits of primary tumor resection in metastatic PNETs, care should be taken when considering this approach in pancreatic head tumors. Hepatic abscesses occur in up to 50% of patients who undergo hepatic artery embolization (HAE) after pancreaticoduodenectomy.[51] Hepatic abscesses in this setting can be difficult to treat and may potentially lead to death. In a recent discussion by a panel of experts, the majority agreed that in patients with neuroendocrine liver metastases, primary tumor resection should not be performed with pancreaticoduodenectomy; however, the majority would pursue primary tumor resection in patients with body/tail lesions.[52]
Cytoreduction of liver metastases. The majority of patients with PNETs present with or later develop metastases.[4] Liver failure is the leading cause of death in patients with liver metastases from PNETs, and treatment is often aimed at reducing tumor burden.[43] It is not uncommon for patients with neuroendocrine liver metastases to have unresectable disease at diagnosis; however, surgery is likely underutilized, as only one in four patients undergoes resection.[53]
Surgical rates have improved as surgical techniques have been refined. A shift toward parenchymal-preserving operations has led to a decrease in morbidity and mortality, with excellent oncologic outcomes even in patients with significant disease burden in the liver (Table 4). Parenchymal-preserving liver surgery is ideal for these well-encapsulated tumors, which are often amenable to enucleation (Figure 4). Nonanatomic resections in combination with ablation offer comparable oncologic results in small tumors.[54]
Many surgeons have advocated for a 70% threshold[43,44] for cytoreductive liver surgery (ie, proceeding to surgery if cytoreduction to at least 70% is deemed possible) instead of the traditional and more stringent 90% threshold,[55] maintaining that there is a survival benefit. Despite more advanced disease and a lower threshold for operating, contemporary surgical series report a 5-year overall survival (OS) rate of 74% to 80% with optimal surgical debulking and in combination with other therapies, in comparison with a historical 5-year OS rate of 40%.[43,56,57] Concomitant primary tumor resection is associated with a longer time to liver progression[58] and improvement in median survival up to 159 months.[58,59] With these excellent data, resection of neuroendocrine liver metastases, with or without primary tumor resection, should be considered in all patients with metastatic PNETs.
Liver transplantation. Liver transplant may be considered for isolated neuroendocrine liver metastases; however, this is still not considered standard of care. While outcomes are promising, disease will recur in most patients.[60,61]
Systemic Therapy
Several systemic options exist for the treatment of advanced PNETs. Typically, treatment is initiated in patients with unresectable high-volume or progressive disease. At times, observation may be the optimal treatment in patients with advanced disease, particularly in those with low-volume disease. Currently, there is no evidence to suggest a role for adjuvant therapy after complete resection.
Octreotide-based therapies
Somatostatin analogs currently approved for clinical use include octreotide (including long-acting octreotide) and lanreotide, which bind both SSTR2 and SSTR5. Functional imaging can predict response to somatostatin analogs, but it does not necessarily dictate therapy.
Three randomized studies have evaluated the role of somatostatin analogs in advanced NETs. The PROMID trial compared long-acting octreotide vs placebo in patients with midgut NETs, excluding PNETs. There was a significant improvement in median progression-free survival (PFS) (14.3 months vs 6 months; P = .000072) but no difference in OS. The CLARINET study compared lanreotide vs placebo in well-/moderately differentiated nonfunctioning NETs (including PNETs) and again showed an improvement in the PFS rate at 2 years (65.1% vs 33.1%; P < .0001) but no improvement in OS. A third phase III randomized trial evaluated the use of pasireotide, a somatostatin analog targeting SSTR5, in octreotide-resistant patients, but there was no difference in the response rate (RR) compared with long-acting octreotide. The trial was stopped prematurely.[62]
The optimal timing for treatment of indolent, nonfunctional PNETs is unclear. Response to somatostatin analogs is diminished in patients with PNETs compared with patients who have small bowel NETs, moderate-grade tumors, extensive liver involvement, or markedly elevated CgA levels.[63] In addition, NETs can potentially become resistant to octreotide therapy.[64] Guidelines suggest somatostatin analog use in patients with advanced PNETs who have asymptomatic high-volume disease or slowly progressive disease.[33,65] Observation in patients with low-volume disease is supported by the fact that some patients initially regressed in the placebo arms of randomized trials.
Targeted therapy
Molecular targeted therapies are suitable for patients with well-differentiated PNETs whose disease progresses on best supportive care or a somatostatin analog, based on randomized studies that have shown an improvement in PFS but not OS. Currently, sunitinib and everolimus are approved for use in PNETs.
Sunitinib is a multi–tyrosine kinase inhibitor that targets the vascular endothelial growth factor receptor (subtypes 1, 2, and 3), among other receptors. Its efficacy in well-differentiated PNETs was demonstrated in a phase III randomized controlled trial that showed an improved median PFS in the sunitinib group compared with placebo (11.5 months vs 5.5 months; P < .001), with an overall response rate (ORR) of 9.3%. Final analysis showed a trend toward improved OS (38.6 months vs 29.1 months; P = .094).[66] However, premature termination and a high crossover rate (69.3%) may have skewed the results.
Everolimus is an inhibitor of mammalian target of rapamycin (mTOR). In phase II trials (including RADIANT-2) in metastatic PNETs, everolimus showed an RR of 4% to 27% and a median PFS between 9.3 and 17.1 months.[67-69] The RADIANT-3 trial compared everolimus vs placebo in patients with progressive low-/intermediate-grade PNETs, and again showed an improved median PFS with everolimus (11 months vs 4.6 months; hazard ratio [HR], 0.35; 95% CI, 0.27–0.45) but no difference in median OS (44 months vs 37.7 months). These findings were further validated in the RADIANT-4 trial, which included patients with tumors in lung and at other gastrointestinal sites.[70]
Combination regimens are currently being investigated. The Cancer and Leukemia Group B 80701/Alliance trial is a phase II randomized controlled trial comparing everolimus ± bevacizumab together with octreotide.[71] Preliminary results show an improved RR in the combination arm (31% vs 12%; P = .005) and a trend toward improvement in median PFS (16.7 months vs 14 months; HR, 0.8; 95% CI, 0.55–1.17; P = .12), but not in median OS. The role of combination therapies is yet to be determined.
Recent interest in additional targets has led to the identification of mutations in MEN1, DAXX/ATRX, and mTOR genes in well-differentiated PNETs (Table 5). Initial studies suggest a prognostic role for these mutations; however, their clinical utility is still unknown.[72] Currently, targeted therapy is not predicated on the presence or absence of mutations, and routine testing is not recommended.[65] However, targeted therapies show promise and remain an active area of research in PNETs.
Cytotoxic chemotherapies
Cytotoxic chemotherapies are reserved for patients who are highly symptomatic from unresectable advanced disease; patients with rapid tumor growth; and those whose disease has progressed on other treatments, such as somatostatin analogs or targeted therapies. Historically, streptozotocin and dacarbazine were the chemotherapeutic agents of choice, with RRs of 30% to 70%; however, both agents are limited by toxicity.[73,74] Currently, the preferred cytotoxic regimens consist of temozolomide in combination with other chemotherapeutic agents (Table 6). Temozolomide-based regimens have ORRs of 24% to 45%.[75-77] PNETs are more likely than other gastrointestinal NETs to respond to temozolomide.[78]
The role of capecitabine in combination with temozolomide (CAPTEM regimen) shows promise, with an RR between 17% and 70% and a partial RR of 65% to 97% for a median duration of 8 to 20 months.[79] Preliminary data from a phase II nonrandomized clinical trial evaluating CAPTEM in PNETs (ClinicalTrials.gov identifier: NCT01824875) show an ORR of 45% in 30 patients, a stable disease rate of 54%, and an overall clinical benefit rate of 97%. CAPTEM is the current cytotoxic regimen of choice at our institution for the treatment of PNETs.
Cytotoxic chemotherapy is effective in high-grade, poorly differentiated NEC. Platinum-based chemotherapy-usually with etoposide-is the mainstay of treatment for both early- and advanced-stage NEC, given its tendency to metastasize.[80] The best treatment for patients with grade-discordant, high-grade NETs is unclear. These patients do not typically respond as well to platinum-based chemotherapy and should be discussed in detail in a multidisciplinary setting to optimize treatment.[32] Details of chemotherapy for NEC will not be discussed in this review.
Other Therapeutic Modalities
HAE
HAE is indicated in patients with high-volume, progressive, or symptomatic liver-predominant disease. HAE is often given sequentially or concurrently with hormonal or systemic treatment, although studies have yet to establish the optimal order of therapy. Bland embolization (gel foam), chemoembolization (gel foam in conjunction with doxorubicin, streptozotocin, cisplatin, or drug-eluting beads), and radioembolization (with yttrium-90 [90Y]) are effective because liver metastases derive their blood supply from the hepatic arterial system. All three techniques are usually well tolerated, with very few serious adverse events occurring. No comparison of these techniques has been completed, and such an assessment would be difficult. The preferred treatment modality is often institutionally dependent.
In a meta-analysis of 18 trials, ORRs among the various intra-arterial techniques ranged from 39% to 95% within 1 to 18 months of treatment.[81] Symptomatic relief occurs in 80% to 90% of patients, whereas the radiologic RR ranges from 30% to 50% and median OS from 22 to 70 months. The range in survival likely reflects the variable timing of treatment, disparity in adjunctive therapies, and the heterogeneity of NETs.
Hepatic arterial therapies can be repeated as necessary. Extrahepatic disease does not always preclude the use of HAE, since a significant tumor burden or progression in the liver may lead to liver failure and death.
KEY POINTS
- Pancreatic neuroendocrine tumors are on the rise, likely due to an increase in detection resulting from better imaging modalities and specialized scans.
- Surgery is the mainstay of treatment for pancreatic neuroendocrine tumors, and includes surgical debulking of both the primary tumor and liver metastases, when possible.
- The future treatment of unresectable pancreatic neuroendocrine tumors appears promising, with peptide receptor radionuclide therapy a potential option and several newer drugs coming down the pipeline.
The role of HAE in conjunction with other treatment modalities is not well established. In addition, there has been no comparison with the standard of care-surgery. Our series suggests that radioembolization after liver resection is safe.[82] HAE in the neoadjuvant setting may potentially convert borderline resectable disease into resectable disease; however, few data are available to support the safety of this approach. Future studies involving HAE should involve a multimodal approach.
Peptide receptor radionuclide therapy
Radiolabeled somatostatin analogs, currently available in the United States for compassionate use only, pending FDA approval, have shown promise in patients whose disease is refractory to other medical therapies. Peptide receptor radionuclide therapy (PRRT) has been used in Europe since the 1990s, based on retrospective data.[83] The two most common radionuclides are 90Y and lutetium-177 (177Lu), which differ in their particle emission and depth of penetration.
90Y-DOTATOC has mainly been studied in the retrospective setting.[84] The largest study to date included 1,109 patients treated with 1 to 10 cycles of 90Y-DOTATOC.[84] Patients who had a response had a significantly longer median survival (44.7 months vs 18.3 months; P < .001), most pronounced in those with a morphologic response. Furthermore, uptake on octreotide-based imaging (including both 111In pentetreotide and 68Ga DOTATATE scanning) was predictive of survival (HR, 0.45; 95% CI, 0.29–0.69; P < .001).
The efficacy of 177Lu-DOTATATE is currently being evaluated in a phase III clinical trial (NETTER-1), which is comparing it vs octreotide for patients with midgut NETs. Interim analysis in 2016 showed promising results, with median PFS not reached in the 177Lu-DOTATATE group compared with 8.4 months in the octreotide group.[85] RRs were 18.8% vs 3.0%, respectively, and preliminary analysis suggests an OS benefit (P < .019).
Data comparing 90Y and 177Lu are limited but may suggest superiority of 177Lu. One retrospective analysis compared 450 patients treated with 90Y alone (RR, 17%; median PFS, 27 months), 177Lu alone (RR, 54%; median PFS, 40 months), or 177Lu in combination with 90Y (RR, 29%; median PFS, 50 months).[86] It is unclear at this time why one agent might outperform the other.
Multiple phase II clinical trials are currently evaluating 177Lu-DOTATATE in various settings, including in poorly differentiated NECs, in combination with chemotherapy (capecitabine + etoposide) for low- to intermediate-grade NETs (CONTROL NETS), in combination with sunitinib (OCCLURANDOM), and in the neoadjuvant setting prior to liver transplant (NEO-LEBE), among others. The role of PRRT in PNETs and its place in the current treatment paradigm is unknown. It is not yet known whether 177Lu will be approved for use in patients with PNETs. In addition, patients can become unresponsive to somatostatin analogs after prolonged treatment,[64] and it is unclear whether this will alter the efficacy of PRRT. Overall, however, PRRT is a promising treatment modality for NETs.
Immunotherapy
The remarkable success of immunotherapy in melanoma and lung cancer has led to interest in using immunotherapeutic approaches in other malignancies. Although research on immunotherapy for NETs is in the earliest stages, there are some preliminary data to suggest an immune response in NETs.[87-90] Several phase I and phase II studies are actively being pursued. A trial involving PDR001, an anti–programmed death 1 inhibitor, in advanced or metastatic NETs (including PNETs), has recently opened for accrual (ClinicalTrials.gov identifier: NCT02955069). Clarification of the role of immunotherapeutics in NETs is highly anticipated.
Summary
PNETs-and NETs more broadly-are increasing in incidence. NETs encompass a heterogeneous group of tumors whose behavior and treatment often depend on grade. The majority of PNETs will metastasize to the liver, and treatment involves a multidisciplinary approach that includes surgery, even in some of the most advanced tumors. Beyond surgery, treatment consists of a combination of octreotide analogs, targeted therapies, systemic chemotherapy, and HAE. The future looks promising for treatment of PNETs, given the pending approval of PRRT and the potential role of immunotherapy in NETs.
Financial Disclosure:The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
Acknowledgments:The writing of this article was supported by funds from the Leo and Anne Albert Trust. The authors wish to thank Indra M. Mahajan, PhD, for her assistance with proofreading and editing the manuscript.
References:
1. Lawrence B, Gustafsson BI, Chan A, et al. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am. 2011;40:1-18.
2. Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063-72.
3. Fitzgerald TL, Hickner ZJ, Schmitz M, Kort EJ. Changing incidence of pancreatic neoplasms: a 16-year review of statewide tumor registry. Pancreas. 2008;37:134-8.
4. Proye C. Natural history of liver metastasis of gastroenteropancreatic neuroendocrine tumors: place for chemoembolization. World J Surg. 2001;25:685-8.
5. Jutric Z, Lewis A, Raoof M, et al. Is it worth resecting gastrointestinal neuroendocrine tumors in patients above the age of 70?
6. Metz DC, Jensen RT. Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology. 2008;135:1469-92.
7. Vagefi PA, Razo O, Deshpande V, et al. Evolving patterns in the detection and outcomes of pancreatic neuroendocrine neoplasms: the Massachusetts General Hospital experience from 1977 to 2005. Arch Surg. 2007;142:347-54.
8. Cheema A, Weber J, Strosberg JR. Incidental detection of pancreatic neuroendocrine tumors: an analysis of incidence and outcomes. Ann Surg Oncol. 2012;19:2932-6.
9. Zerbi A, Falconi M, Rindi G, et al. Clinicopathological features of pancreatic endocrine tumors: a prospective multicenter study in Italy of 297 sporadic cases. Am J Gastroenterol. 2010;105:1421-9.
10. Halfdanarson TR, Rabe KG, Rubin J, Petersen GM. Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol. 2008;19:1727-33.
11. Khashab MA, Yong E, Lennon AM, et al. EUS is still superior to multidetector computerized tomography for detection of pancreatic neuroendocrine tumors. Gastrointest Endosc. 2011;73:691-6.
12. Reidy-Lagunes DL, Gollub MJ, Saltz LB. Addition of octreotide functional imaging to cross-sectional computed tomography or magnetic resonance imaging for the detection of neuroendocrine tumors: added value or an anachronism? J Clin Oncol. 2011;29:e74-e75.
13. Noone TC, Hosey J, Firat Z, Semelka RC. Imaging and localization of islet-cell tumours of the pancreas on CT and MRI. Best Pract Res Clin Endocrinol Metab. 2005;19:195-211.
14. James PD, Tsolakis AV, Zhang M, et al. Incremental benefit of preoperative EUS for the detection of pancreatic neuroendocrine tumors: a meta-analysis. Gastrointest Endosc. 2015;81:848-56.e1.
15. Zimmer T, Stolzel U, Bader M, et al. Endoscopic ultrasonography and somatostatin receptor scintigraphy in the preoperative localisation of insulinomas and gastrinomas. Gut. 1996;39:562-8.
16. Sharma P, Arora S, Karunanithi S, et al. Somatostatin receptor based PET/CT imaging with 68Ga-DOTA-Nal3-octreotide for localization of clinically and biochemically suspected insulinoma. Q J Nucl Med Mol Imaging. 2016;60:69-76.
17. Janson ET, Westlin JE, Eriksson B, et al. [111In-DTPA-D-Phe1]octreotide scintigraphy in patients with carcinoid tumours: the predictive value for somatostatin analogue treatment. Eur J Endocrinol. 1994;131:577-81.
18. Papotti M, Bongiovanni M, Volante M, et al. Expression of somatostatin receptor types 1-5 in 81 cases of gastrointestinal and pancreatic endocrine tumors. A correlative immunohistochemical and reverse-transcriptase polymerase chain reaction analysis. Virchows Arch. 2002;440:461-75.
19. US Food and Drug Administration. FDA approves new diagnostic imaging agent to detect rare neuroendocrine tumors. June 1, 2016.
20. Sadowski SM, Neychev V, Millo C, et al. Prospective study of 68Ga-DOTATATE positron emission tomography/computed tomography for detecting gastro-entero-pancreatic neuroendocrine tumors and unknown primary sites. J Clin Oncol. 2016;34:588-96.
21. Sharma P, Arora S, Mukherjee A, et al. Predictive value of 68Ga-DOTANOC PET/CT in patients with suspicion of neuroendocrine tumors: is its routine use justified? Clin Nucl Med. 2014;39:37-43.
22. Treglia G, Castaldi P, Rindi G, et al. Diagnostic performance of Gallium-68 somatostatin receptor PET and PET/CT in patients with thoracic and gastroenteropancreatic neuroendocrine tumours: a meta-analysis. Endocrine. 2012;42:80-7.
23. Ilhan H, Fendler WP, Cyran CC, et al. Impact of (68)Ga-DOTATATE PET/CT on the surgical management of primary neuroendocrine tumors of the pancreas or ileum. Ann Surg Oncol. 2015;22:164-71.
24. Eriksson B, Oberg K, Stridsberg M. Tumor markers in neuroendocrine tumors. Digestion. 2000;62(suppl 1):33-8.
25. Yang X, Yang Y, Li Z, et al. Diagnostic value of circulating chromogranin A for neuroendocrine tumors: a systematic review and meta-analysis. PLoS One. 2015;10:e0124884.
26. Tian T, Gao J, Li N, et al. Circulating chromogranin A as a marker for monitoring clinical response in advanced gastroenteropancreatic neuroendocrine tumors. PLoS One. 2016;11:e0154679.
27. Oberg K. Management of neuroendocrine tumours. Ann Oncol. 2004;15(suppl 4):iv293-iv298.
28. Sowa-Staszczak A, Chrzan R, Pach D, et al. Are RECIST criteria sufficient to assess response to therapy in neuroendocrine tumors? Clin Imaging. 2012;36:360-4.
29. de Mestier L, Dromain C, d’Assignies G, et al. Evaluating digestive neuroendocrine tumor progression and therapeutic responses in the era of targeted therapies: state of the art. Endocr Relat Cancer. 2014;21:R105-R120.
30. Basturk O, Yang Z, Tang LH, et al. The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol. 2015;39:683-90.
31. Yang Z, Tang LH, Klimstra DS. Effect of tumor heterogeneity on the assessment of Ki67 labeling index in well-differentiated neuroendocrine tumors metastatic to the liver: implications for prognostic stratification. Am J Surg Pathol. 2011;35:853-60.
32. Sorbye H, Welin S, Langer SW, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24:152-60.
33. Kulke MH, Anthony LB, Bushnell DL, et al. NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010;39:735-52.
34. Norton JA, Harris EJ, Chen Y, et al. Pancreatic endocrine tumors with major vascular abutment, involvement, or encasement and indication for resection. Arch Surg. 2011;146:724-32.
35. Hashim YM, Trinkaus KM, Linehan DC, et al. Regional lymphadenectomy is indicated in the surgical treatment of pancreatic neuroendocrine tumors (PNETs). Ann Surg. 2014;259:197-203.
36. Fischer L, Bergmann F, Schimmack S, et al. Outcome of surgery for pancreatic neuroendocrine neoplasms. Br J Surg. 2014;101:1405-12.
37. Gratian L, Pura J, Dinan M, et al. Impact of extent of surgery on survival in patients with small nonfunctional pancreatic neuroendocrine tumors in the United States. Ann Surg Oncol. 2014;21:3515-21.
38. Wong J, Fulp WJ, Strosberg JR, et al. Predictors of lymph node metastases and impact on survival in resected pancreatic neuroendocrine tumors: a single-center experience. Am J Surg. 2014;208:775-80.
39. Kloppel G. Classification and pathology of gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2011;18(suppl 1):S1-S16.
40. Cauley CE, Pitt HA, Ziegler KM, et al. Pancreatic enucleation: improved outcomes compared to resection. J Gastrointest Surg. 2012;16:1347-53.
41. Sadot E, Reidy-Lagunes DL, Tang LH, et al. Observation versus resection for small asymptomatic pancreatic neuroendocrine tumors: a matched case-control study. Ann Surg Oncol. 2016;23:1361-70.
42. Lee LC, Grant CS, Salomao DR, et al. Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): role for nonoperative management. Surgery. 2012;152:965-74.
43. Maxwell JE, Sherman SK, O’Dorisio TM, et al. Liver-directed surgery of neuroendocrine metastases: what is the optimal strategy? Surgery. 2016;159:320-33.
44. Graff-Baker AN, Sauer DA, Pommier SJ, Pommier RF. Expanded criteria for carcinoid liver debulking: maintaining survival and increasing the number of eligible patients. Surgery. 2014;156:1369-76; discussion 76-7.
45. Capurso G, Rinzivillo M, Bettini R, et al. Systematic review of resection of primary midgut carcinoid tumour in patients with unresectable liver metastases. Br J Surg. 2012;99:1480-6.
46. Lewis A, White M, Raoof M, et al. Resection of primary gastrointestinal neuroendocrine tumor improves overall survival with or without treatment of liver metastases. Presented at the Society of Surgical Oncology Annual Cancer Symposium; March 2–5, 2016; Boston, MA. Abstr P158.
47. Bertani E, Fazio N, Radice D, et al. Resection of the primary tumor followed by peptide receptor radionuclide therapy as upfront strategy for the treatment of G1-G2 pancreatic neuroendocrine tumors with unresectable liver metastases. Ann Surg Oncol. 2016;23:981-9.
48. Bettini R, Mantovani W, Boninsegna L, et al. Primary tumour resection in metastatic nonfunctioning pancreatic endocrine carcinomas. Dig Liver Dis. 2009;41:49-55.
49. Nguyen SQ, Angel LP, Divino CM, et al. Surgery in malignant pancreatic neuroendocrine tumors. J Surg Oncol. 2007;96:397-403.
50. Solorzano CC, Lee JE, Pisters PW, et al. Nonfunctioning islet cell carcinoma of the pancreas: survival results in a contemporary series of 163 patients. Surgery. 2001;130:1078-85.
51. Woo S, Chung JW, Hur S, et al. Liver abscess after transarterial chemoembolization in patients with bilioenteric anastomosis: frequency and risk factors. AJR Am J Roentgenol. 2013;200:1370-7.
52. Frilling A, Modlin IM, Kidd M, et al. Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol. 2014;15:e8-e21.
53. Lewis A, White M, Ituarte P, et al. Are we maximizing liver treatment for metastases in neuroendocrine tumors? Presented at the Society of Surgical Oncology Annual Cancer Symposium; March 2–5, 2016; Boston, MA. Abstr P216.
54. Leung U, Kuk D, D’Angelica MI, et al. Long-term outcomes following microwave ablation for liver malignancies. Br J Surg. 2015;102:85-91.
55. Sarmiento JM, Heywood G, Rubin J, et al. Surgical treatment of neuroendocrine metastases to the liver: a plea for resection to increase survival. J Am Coll Surg. 2003;197:29-37.
56. Mayo SC, de Jong MC, Pulitano C, et al. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Ann Surg Oncol. 2010;17:3129-36.
57. Taner T, Atwell TD, Zhang L, et al. Adjunctive radiofrequency ablation of metastatic neuroendocrine cancer to the liver complements surgical resection. HPB (Oxford). 2013;15:190-5.
58. Givi B, Pommier SJ, Thompson AK, et al. Operative resection of primary carcinoid neoplasms in patients with liver metastases yields significantly better survival. Surgery. 2006;140:891-7; discussion 7-8.
59. Norlen O, Stalberg P, Oberg K, et al. Long-term results of surgery for small intestinal neuroendocrine tumors at a tertiary referral center. World J Surg. 2012;36:1419-31.
60. Le Treut YP, Gregoire E, Klempnauer J, et al. Liver transplantation for neuroendocrine tumors in Europe-results and trends in patient selection: a 213-case European liver transplant registry study. Ann Surg. 2013;257:807-15.
61. Gedaly R, Daily MF, Davenport D, et al. Liver transplantation for the treatment of liver metastases from neuroendocrine tumors: an analysis of the UNOS database. Arch Surg. 2011;146:953-8.
62. Wolin EM, Jarzab B, Eriksson B, et al. Phase III study of pasireotide long-acting release in patients with metastatic neuroendocrine tumors and carcinoid symptoms refractory to available somatostatin analogues. Drug Des Devel Ther. 2015;9:5075-86.
63. Laskaratos FM, Walker M, Naik K, et al. Predictive factors of antiproliferative activity of octreotide LAR as first-line therapy for advanced neuroendocrine tumours. Br J Cancer. 2016;115:1321-7.
64. Strosberg JR, Yao JC, Bajetta E, et al. Efficacy of octreotide long-acting repeatable in neuroendocrine tumors: RADIANT-2 placebo arm post hoc analysis. Endocr Relat Cancer. 2015;22:933-40.
65. Falconi M, Eriksson B, Kaltsas G, et al. ENETS consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016;103:153-71.
66. Faivre S, Niccoli P, Castellano D, et al. Sunitinib in pancreatic neuroendocrine tumors: updated progression-free survival and final overall survival from a phase III randomized study. Ann Oncol. 2016 Nov 10. [Epub ahead of print]
67. Yao JC, Lombard-Bohas C, Baudin E, et al. Daily oral everolimus activity in patients with metastatic pancreatic neuroendocrine tumors after failure of cytotoxic chemotherapy: a phase II trial. J Clin Oncol. 2010;28:69-76.
68. Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:514-23.
69. Oh DY, Kim TW, Park YS, et al. Phase 2 study of everolimus monotherapy in patients with nonfunctioning neuroendocrine tumors or pheochromocytomas/paragangliomas. Cancer. 2012;118:6162-70.
70. Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387:968-77.
71. Kulke MH, Niedzwiecki D, Foster NR, et al. Randomized phase II study of everolimus versus everolimus plus bevacizumab in patients with locally advanced or metastatic pancreatic neuroendocrine tumors (pNET), CALGB 80701 (Alliance). J Clin Oncol. 2015;33(suppl):abstr 4005.
72. Jiao Y, Shi C, Edil BH, et al. DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science. 2011;331:1199-203.
73. Moertel CG, Lefkopoulo M, Lipsitz S, et al. Streptozocin-doxorubicin, streptozocin-fluorouracil or chlorozotocin in the treatment of advanced islet-cell carcinoma. N Engl J Med. 1992;326:519-23.
74. Ramanathan RK, Cnaan A, Hahn RG, et al. Phase II trial of dacarbazine (DTIC) in advanced pancreatic islet cell carcinoma: study of the Eastern Cooperative Oncology Group-E6282. Ann Oncol. 2001;12:1139-43.
75. Kulke MH, Stuart K, Enzinger PC, et al. Phase II study of temozolomide and thalidomide in patients with metastatic neuroendocrine tumors. J Clin Oncol. 2006;24:401-6.
76. Chan JA, Stuart K, Earle CC, et al. Prospective study of bevacizumab plus temozolomide in patients with advanced neuroendocrine tumors. J Clin Oncol. 2012;30:2963-8.
77. Chan JA, Blaszkowsky L, Stuart K, et al. A prospective, phase 1/2 study of everolimus and temozolomide in patients with advanced pancreatic neuroendocrine tumor. Cancer. 2013;119:3212-8.
78. Kulke MH, Hornick JL, Frauenhoffer C, et al. O6-methylguanine DNA methyltransferase deficiency and response to temozolomide-based therapy in patients with neuroendocrine tumors. Clin Cancer Res. 2009;15:338-45.
79. Saif MW, Kaley K, Brennan M, et al. A retrospective study of capecitabine/temozolomide (CAPTEM) regimen in the treatment of metastatic pancreatic neuroendocrine tumors (pNETs) after failing previous therapy. J Oncol Pract. 2013;14:498-501.
80. Sorbye H, Strosberg J, Baudin E, et al. Gastroenteropancreatic high-grade neuroendocrine carcinoma. Cancer. 2014;120:2814-23.
81. Kennedy A, Bester L, Salem R, et al. Role of hepatic intra-arterial therapies in metastatic neuroendocrine tumours (NET): guidelines from the NET-Liver-Metastases Consensus Conference. HPB (Oxford). 2015;17:29-37.
82. Kessler J, Lewis A, Gagandeep S, et al. Radioembolization following liver resection: safety and dosing considerations. J Vasc Interv Radiol. 2016;27:46-51.
83. Carollo A, Papi S, Chinol M. Lutetium-177 labeled peptides: the European Institute of Oncology experience. Curr Radiopharm. 2016;9:19-32.
84. Imhof A, Brunner P, Marincek N, et al. Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol. 2011;29:2416-23.
85. Strosberg J, Wolin E, Chasen B, et al. NETTER-1 phase III in patients with midgut neuroendocrine tumors treated with 177Lu-DOTATATE: efficacy and safety results. Clin Adv Hematol Oncol. 2016;14(suppl 7):8-9.
86. Horsch D, Ezziddin S, Haug A, et al. Effectiveness and side-effects of peptide receptor radionuclide therapy for neuroendocrine neoplasms in Germany: a multi-institutional registry study with prospective follow-up. Eur J Cancer. 2016;58:41-51.
87. Vikman S, Giandomenico V, Sommaggio R, et al. CD8+ T cells against multiple tumor-associated antigens in peripheral blood of midgut carcinoid patients. Cancer Immunol Immunother. 2008;57:399-409.
88. Vikman S, Sommaggio R, De La Torre M, et al. Midgut carcinoid patients display increased numbers of regulatory T cells in peripheral blood with infiltration into tumor tissue. Acta Oncol. 2009;48:391-400.
89. Kosaloglu Z, Zornig I, Halama N, et al. Identification of immunotherapeutic targets by genomic profiling of rectal NET metastases. Oncoimmunology. 2016;5:e1213931.
90. Alonso-Gordoa T, Capdevila J, Grande E. GEP-NETs update: biotherapy for neuroendocrine tumours. Eur J Endocrinol. 2015;172:R31-R46.
91. Glazer ES, Tseng JF, Al-Refaie W, et al. Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB (Oxford). 2010;12:427-33.
92. Boudreaux JP, Putty B, Frey DJ, et al. Surgical treatment of advanced-stage carcinoid tumors: lessons learned. Ann Surg. 2005;241:839-45; discussion 45-6.
93. Jones S, Zhang X, Parsons DW, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321:1801-6.
94. Ekeblad S, Sundin A, Janson ET, et al. Temozolomide as monotherapy is effective in treatment of advanced malignant neuroendocrine tumors. Clin Cancer Res. 2007;13:2986-91.
95. Strosberg JR, Fine RL, Choi J, et al. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer. 2011;117:268-75.
Articles in this issue
over 8 years ago
Management of Breast Cancer Therapy–Related Sexual DysfunctionNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.