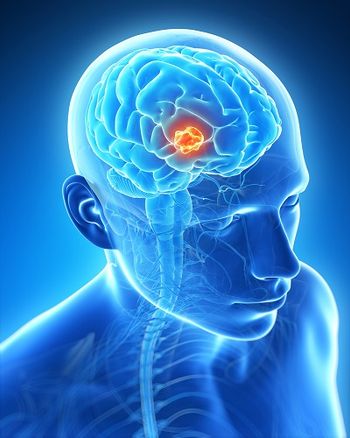
Polio-Rhinovirus Conjugate Shows Promise in Early Recurrent Glioblastoma Trial
A phase I trial of an oncolytic polio/rhinovirus vaccine was safe and showed promising efficacy in patients with recurrent glioblastoma.
A phase I trial of an oncolytic polio/rhinovirus vaccine was safe and showed promising efficacy in patients with recurrent glioblastoma, according to results presented at the Society for Neuro-Oncology (SNO) Annual Scientific Meeting in Miami.
PVS-RIPO is a live attenuated, oral serotype 1 poliovirus vaccine that contains a heterologous internal ribosomal entry site arising from human rhinovirus (cause of the common cold) type 2. The vaccine recognizes nectin-like molecule-5, a tumor antigen that is widely expressed in malignancies. “To allow safe targeting of cancer cells with poliovirus, we need the neural competency… to be ablated,” said Annick Desjardins, MD, of Duke Cancer Center in Durham, North Carolina. “That’s where the rhinovirus comes in.” The internal ribosomal entry site is essentially replaced by that of the rhinovirus, she said.
Desjardins and her co-authors are co-owners of the intellectual property and a pending patent on this therapy; she said that all data were reviewed by an external data safety and monitoring board.
In this phase I trial, the vaccine was delivered intratumorally via convection-enhanced delivery; this involves stereotactically placed catheters directly into the malignancy. The trial included 15 patients, all of whom had recurrent supratentorial glioblastoma, a solitary tumor between 1 and 5 cm in diameter, with at least 4 weeks passed since chemotherapy or other medical therapy. Dose escalation through five levels eventually revealed one dose-limiting toxicity at level 5, and an additional six patients were then treated at dose level 2.
Adverse events that were considered potentially related to the study included hemiparesis (five patients with grade 3), intracranial hemorrhage at catheter removal (one patient at level 4, considered a dose-limiting toxicity), lymphopenia (four patients with grade 3), seizure (one patient with grade 3), and hyperglycemia (three patients with grade 3), as well as lethargy, headache, diarrhea, paresthesia, and hyperbilirubinemia. Grade 1 fever, cough, nasal congestion, memory impairment, and others were also observed.
The median survival was 15.2 months, and the 12-month survival rate was 70%; 18- and 24-month survival rates were 43.8% and 29.2%, respectively.
“Intratumoral infusion of PVS-RIPO via convection-enhanced delivery is safe,” Desjardins concluded. “Initial MRI worsening seems to improve over time at lower dose levels.” At higher dose levels, prolonged corticosteroid use was required. She said that the phase I dose escalation study is now completed, and her group is proceeding with a dose expansion cohort, including investigation of a lower dose level.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.