- ONCOLOGY Vol 20 No 5
- Volume 20
- Issue 5
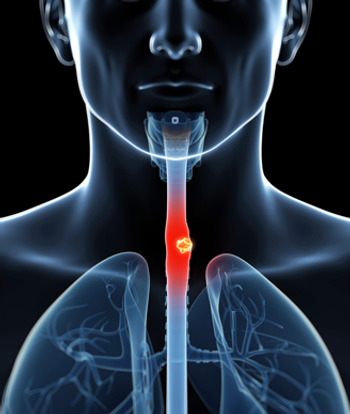
Primary Combined-Modality Therapy for Esophageal Cancer
Based on positive results from the Radiation Therapy Oncology Group (RTOG) 85-01 trial, the conventional nonsurgical treatment of esophageal carcinoma is combined-modality therapy. Dose intensification of the RTOG 85-01 regimen, examined in the Intergroup (INT)-0123/RTOG 94-05 trial, did not improve local control or survival. Areas of clinical investigation include the development of combined-modality therapy regimens with newer systemic agents, the use of 18F-fluorodeoxyglucose positron-emission tomography to assist in the development of innovative radiation treatment planning techniques, and the identification of prognostic molecular markers. The addition of surgery following primary combined-modality therapy apparently does not improve survival, but this finding is controversial.
Based on positive results from the Radiation Therapy Oncology Group (RTOG) 85-01 trial, the conventional nonsurgical treatment of esophageal carcinoma is combined-modality therapy. Dose intensification of the RTOG 85-01 regimen, examined in the Intergroup (INT)-0123/RTOG 94-05 trial, did not improve local control or survival. Areas of clinical investigation include the development of combined-modality therapy regimens with newer systemic agents, the use of 18F-fluorodeoxyglucose positron-emission tomography to assist in the development of innovative radiation treatment planning techniques, and the identification of prognostic molecular markers. The addition of surgery following primary combined-modality therapy apparently does not improve survival, but this finding is controversial.
Combined-modality therapy has been used for preoperative, postoperative, and primary nonoperative treatment in patients diagnosed with esophageal cancer. Most contemporary trials of combined-modality therapy have included both patients with squamous cell cancers and those diagnosd with adenocarcinomas. This trend will continue as the incidence of adenocarcinoma increases relative to that of squamous cell cancers.[1]
However, the impact of histology on outcome in this patient population is unclear. Presently, the data are conflicting; some series have reported different results by histology, whereas others have reported no difference. Fortunately, the US Intergroup randomized trials are stratified by histology. Until these data are available, the impact of histology cannot be assessed adequately, and it is reasonable to treat patients with squamous cell cancer and those with adenocarcinoma similarly.
Radiation Therapy Alone
Many historical series have reported the results of external-beam radiation therapy alone. Most have included patients with unfavorable features (eg, unresectable T4 disease). In the series by De-Ren, 184 of 678 patients had stage IV disease.[2] Overall, the 5-year survival rate for patients treated with radiation therapy alone is 0% to 10%.[2-4] Even in the radiation therapy-alone arm of the Radiation Therapy Oncology Group (RTOG) 85-01 trial, in which patients received 64 Gy with modern techniques, all patients succumbed to their disease within 3 years.[5,6]
There have been limited reports of radiation therapy given to patients with clinically early-stage disease. The trial by Sykes et al was limited to 101 patients (90% with squamous cell carcinoma) with tumors smaller than 5 cm who received 45 to 52.5 Gy in 15 to 16 fractions; the 5-year survival of that cohort was 20%.[7] Sai et al reported more favorable results in 34 patients with clinical stage I squamous cell cancers who were treated with external-beam radiation alone (median dose: 64 Gy) or external beam (median dose: 52 Gy) plus brachytherapy; the 5-year survival in that series was 59%.[8]
In summary, radiation therapy alone should be reserved for palliation or for patients who are medically unable to receive chemotherapy. In contrast, combined-modality therapy-the standard of care-has produced more favorable results.
Standard Approaches to Combined-Modality Therapy
Six randomized trials have compared radiation therapy alone with combined-modality therapy, but the only trial designed to deliver adequate doses of systemic chemotherapy with concurrent radiation therapy was the RTOG 85-01 trial.[5,9,10] In this Intergroup trial, which primarily included patients with squamous cell carcinoma, patients received four cycles of fluorouracil (5-FU)/cisplatin and 50 Gy of radiation therapy concurrently, beginning on day 1 of chemotherapy. The control arm received radiation therapy alone, although at a higher dose (64 Gy) than that received by the combined-modality therapy arm.
Compared with those given radiation therapy alone, patients receiving combined-modality therapy exhibited a significant improvement in median survival (14 vs 9 months) and 5-year survival rate (27% vs 0%; P < .0001).[9] The 8-year survival rate was 22%.[10] Histology did not significantly influence the results, with 21% of 107 squamous cell carcinoma patients surviving at 5 years, compared with 13% of 23 adenocarcinoma patients. African-Americans had larger primary tumors, all of which were squamous cell cancers. However, no difference in survival was noted between African-American and white patients.[11] The incidence of local failure as the first site of failure (defined as local persistence or recurrence) was also lower in the combined-modality arm (47% vs 65%). These positive results led to an early closing of the protocol. Thereafter, an additional 69 eligible patients were treated with the same combined-modality regimen; in this nonrandomized group, the 5-year survival rate was 14%, and the local failure rate was 52%.
Combined-modality therapy is associated with a higher incidence of toxicity. According to the 1997 report of the RTOG 85-01 trial, patients given combined-modality therapy had a higher incidence of acute grade 3 (44% vs 25%) and grade 4 toxicity (20% vs 3%) than did patients given radiation therapy alone. Including one treatment-related death (2%), the incidence of total acute grade 3+ toxicity was 66% in the combined-modality therapy group.[9] Results from the 1999 report of the same trial showed the incidence of late grade 3+ toxicity to be similar in the combined-modality and radiation-alone arms (29% vs 23%).[10] However, grade 4+ toxicity remained higher among patients receiving combined-modality therapy (10% vs 2%). Interestingly, the nonrandomized combined- modality therapy group experienced a similar incidence of late grade 3+ toxicity (28%), a lower incidence of grade 4 toxicity (4%), and no treatment-related deaths.
Based on the positive results from the RTOG 85-01 trial, the conventional nonsurgical treatment of choice for esophageal carcinoma is combined-modality therapy. This change is reflected in the US Patterns of Care survey (1996-1999), in which only 11% of patients diagnosed with the disease and treated with radiation as a component of their initial therapy received radiation without chemotherapy.[12] In contrast, the Japanese Patterns of Care survey (1995-1997) reported that 60% of esophageal cancer patients received radiation without chemotherapy.[13]
Intensification of Combined-Modality Therapy
After the local failure rate in the RTOG 85-01 combined-modality therapy arm was noted to be 45%, new approaches (eg, intensification of combined-modality therapy and escalation of the radiation dose) were developed in an attempt to improve these results.
Neoadjuvant Chemotherapy
A limited number of phase I/II trials have tested the use of neoadjuvant chemotherapy given before combined-modality therapy using non-5-FU-containing regimens, such as paclitaxel/cisplatin or irinotecan (CPT-11, Camptosar)/cisplatin.[14-16] The majority of patients in these trials had adenocarcinomas, and most underwent surgery, although resection was optional. Bains and associates reported that 92% of 38 patients presenting with dysphagia had relief after completing two cycles (weeks 1 and 4) of neoadjuvant paclitaxel and cisplatin.[14] Ilson et al reported similar results in 19 patients given two cycles of neoadjuvant irinotecan plus cisplatin on weeks 1, 2, 4, and 5 before starting combined-modality therapy.[16] Treatment was well tolerated, with no grade 3+ nonhematologic toxicity reported. Only 5% of patients required a feeding tube. Of 16 patients who presented with dysphagia, 81% experienced relief of this symptom after completing neoadjuvant chemotherapy.
Another potential advantage of neoadjuvant chemotherapy is the early identification of patients who may or may not respond to the regimen being delivered. Ott et al examined 35 patients with adenocarcinoma of the gastroesophageal junction or stomach who first underwent an 18F-fluorodeoxyglucose positron-emission tomography (FDG-PET) scan 2 weeks after cisplatin/5-FU/leucovorin was started and then had surgery. The scan was able to predict patients who would respond to the full course of chemotherapy, as shown by analysis of the surgical specimens.[17] Weider and associates reported similar findings in 38 patients with squamous cell cancers.[18] Although this method is investigational, it may identify nonresponders early, and changing the chemotherapeutic regimen may then be helpful.
In summary, although the results of early trials primarily using 5-FU/cisplatin-based neoadjuvant regimens did not suggest a benefit,[19] more recent trials of paclitaxel- and irinotecan-based regimens revealed more favorable response rates and rapid improvement of dysphagia.
Intensification of Intraluminal Brachytherapy
Another approach to the dose intensification of combined-modality therapy is increasing the radiation dose by using brachytherapy and/or external-beam radiation therapy. Intraluminal brachytherapy allows dose escalation to the primary tumor and protection of surrounding structures, such as the lung, heart, and spinal cord.[20] This technique has been used for primary therapy (usually as a palliative modality)[21]; it also has been used as a boost following external-beam radiation therapy or combined-modality therapy.[22] There are technical and radiobiologic differences between high-dose and low-dose rates but no clear therapeutic advantages to either.
Reports of investigational series in which doses were escalated by combining brachytherapy with either external-beam or combined-modality therapy reported results similar to those of series that did not use brachytherapy. Calais et al reported a local failure rate of 43% and a 5-year actuarial survival of 18% using combined therapy with external radiation, three cycles of concomitant chemotherapy, and then administration of high-dose-rate brachytherapy.[23] Even with the more favorable subset of patients with clinical T1-2 disease, Yorozu et al reported a local failure rate of 44% and a 5-year survival of 26% among 124 patients treated with external irradiation followed by high-dose-rate brachytherapy.[24]
In the RTOG 92-07 trial, 75 patients (92% with squamous cell cancers of the thoracic esophagus) received the combined-modality regimen (5-FU/cisplatin plus 50 Gy of external-beam irradiation) used in RTOG 85-01 followed by a boost during cycle 3 of chemotherapy with either low- or high-dose-rate intraluminal brachytherapy.[25] At a median follow-up of only 11 months, the complete response rate was 73%, and 27% of patients developed local failure as the first sign of failure. Grade 3 acute toxicity occurred in 58% of patients, grade 4 acute toxicity in 26%, and treatment-related deaths in 8%. The cumulative incidence of fistula was 18% per year, and the crude incidence was 14%. Of the six treatment-related fistulas noted, three were fatal. Given the significant toxicity reported, this treatment approach should be used with caution.
Based on this experience, the American Brachytherapy Society has developed guidelines for esophageal brachytherapy.[26] For patients treated in the curative setting, brachytherapy should be limited to tumors 10 cm or less in size with no evidence of distant metastasis. Contraindications include tracheal or bronchial involvement, cervical esophagus location, or stenosis that cannot be bypassed. The applicator should have an external diameter of 6 to 10 cm. If combined-modality therapy (defined as 5-FU-based chemotherapy plus 45-50 Gy) is used, the recommended doses of brachytherapy are 10 Gy given in two weekly fractions of 5 Gy each for the high-dose-rate regimen and 20 Gy in a single fraction at 4 to 10 Gy/h for the low dose rate. The doses should be prescribed to 1 cm from the source. Finally, brachytherapy should be delivered after the completion of external-beam irradiation and not concurrently with chemotherapy.
In patients treated in the curative setting, the addition of brachytherapy does not appear to improve results, compared with radiation therapy or combined-modality therapy alone. Therefore, the further benefit of adding intraluminal brachytherapy to radiation or combined-modality therapy, although reasonable, remains unclear.
Intensification of External-Beam Irradiation
Conventional Fractionation-Some investigators have advocated combined-modality therapy using higher external-beam radiation doses. Data from retrospective series suggest improved locoregional control with higher radiation doses.[27] Calais et al[28] and the Intergroup (INT) 0122 investigators[29] reported that doses of 64.8 to 65 Gy are tolerable. Based on these results, the 64.8-Gy dose was used in the experimental arm of the esophageal cancer trial INT 0123 (RTOG 94-05), which was the follow-up trial to RTOG 85-01.
In INT 0123, patients with either squamous cell (85%) or adenocarcinomas (15%) were selected for a nonsurgical approach and then randomized to receive a slightly modified RTOG 85-01 combined-modality regimen using 50.4 Gy or the same chemotherapy plus 64.8 Gy. Modifications to the original RTOG 85-01 combined-modality therapy arm included (1) using 1.8-Gy fractions to 50.4 Gy rather than 2-Gy fractions to 50 Gy, (2) treating patients with 5-cm proximal and distal margins to 50.4 Gy rather than treating the whole esophagus with the first 30 Gy and then with a cone down with 5-cm margins to 50 Gy, (3) not beginning cycle 3 of 5-FU/cisplatin until 4 weeks, rather than 3 weeks, following the completion of radiation therapy, and (4) delivering chemotherapy cycles 3 and 4 every 4 weeks rather than every 3 weeks.
The INT 0123 was closed to accrual in 1999, when an interim analysis revealed that the high-dose arm was unlikely to achieve a superior survival compared with the standard-dose arm. For the 218 eligible patients in the high-dose and standard-dose arms, there was no significant difference in median survival (13.0 vs 18.1 months, respectively) or 2-year survival (31% vs 40%).[30] Although 11 treatment-related deaths occurred in the high-dose arm compared with 2 in the standard-dose arm, 7 of the 11 occurred in patients who had received 50.4 Gy of radiation therapy or less.
To help determine whether the unexplained increase in treatment-related deaths in the high-dose arm was responsible for the inferior survival rate, the investigators performed a separate survival analysis that included only patients given the assigned radiation dose. Despite this biased analysis, no survival advantage was noted in the high-dose arm.
When data from the high-dose and standard-dose arms were examined, the crude incidence of local failure and/or persistence of local disease (50% vs 55%, respectively) and distant failure (9% vs 16%) were lower in the high-dose arm; however, this did not reach statistical significance. At 2 years, the cumulative incidence of local failure was 56% for the high-dose arm vs 52% for the standard-dose arm (P= .71). Therefore, based on results from the INT 0123 trial, the standard dose of external-beam radiation remains 50.4 Gy.
The modifications to the original RTOG 85-01 combined-modality therapy arm outlined above did not adversely affect the local control or survival rate in the control arm of INT 0123. Thus, the radiation doses and field design used in the control arm of INT 0123 should be used.
Altered Fractionation-Radiation therapy can be intensified by increasing the total dose or by instituting accelerated hyperfractionation. Wang et al randomized 101 patients with squamous cell cancer to continuous accelerated hyperfractionated radiation (66 Gy) or to late-course, accelerated hyperfractionated radiation (68.4 Gy).[31] Compared with patients who received late-course accelerated hyperfractionated radiation, those treated with continuous accelerated hyperfractionated radiation had a significantly higher incidence of grade 3+ esophagitis (61% vs 10%, respectively; P < .001). However, no benefit in local control or survival was noted when this method was used.
Zhao and associates treated 201 patients with squamous cell cancer using 41.4 Gy followed by late-course accelerated hyperfractionation to 68.4 Gy[32]; The results-38% local failure and 26% 5-year survival-were similar to those of RTOG 85-01. In another trial, Choi et al treated 46 patients with 5-FU/cisplatin and twice-daily radiation therapy using a concurrent boost technique and reported a 37% 5-year survival.[33] Although these approaches are reasonable, most series report an increase in acute toxicity without any clear therapeutic benefit. Thus, these regimens remain investigational.
Split-course radiation is inferior to continuous-course schedules. In a randomized trial from France, 95 patients with squamous cell cancers who received continuous-course radiation therapy had a significantly higher local control rate (57% vs 29%) and 2-year event-free survival (33% vs 23%), and a borderline-significant improvement in 2-year survival rate (37% vs 23%), compared with those who receive split-course radiation.[34]
Novel Radiation Approaches-On the basis of the more favorable dose distribution of protons, Sugahara and colleagues treated 46 patients (45 with squamous cell cancer) with a combination of protons or combined protons/photons to a median dose of 82 Gy or 76 Gy, respectively.[35] Although 23 of 46 patients had T1 disease, the rate of local failure was still 35%, and the 5-year survival rate was only 13%.
Nutting and colleagues compared two-phase, conformal radiotherapy with intensity-modulated radiation in five esophageal cancer patients given 55 Gy of radiation therapy plus concurrent chemotherapy.[36] Treatment plans using both techniques were compared using dose-volume histograms and normal tissue complication probabilities. The intensity-modulated radiation field, using nine equispaced fields, provided no improvement over conformal radiation, since the larger number of fields in the intensity-modulated radiation plan distributed a low dose over the entire lung. In contrast, intensity-modulated radiation using four fields-equal to the conformal fields-offered an improvement in lung sparing.
Radiation Field Design and Treatment Techniques-Radiation field design for esophageal cancer requires careful techniques.[37] Depending on the location of the primary tumor, a number of sensitive organs may be in the radiation field. These include, but are not limited to, the skin, spinal cord, lung, heart, intestine, stomach, kidney, and liver. Minimizing the dose to these structures while delivering an adequate dose to the primary tumor and locoregional lymph nodes requires patient immobilization and computed tomography (CT)-based treatment planning for organ identification, lung correction, and development of dose-volume histograms.
Computed tomography can identify adjacent organs and structures, but it may be limited in defining the extent of the primary tumor. To assess the consistency of target volume delineation, Tai and colleagues sent sample cases with CT scans to 48 radiation oncologists throughout Canada, asking them to complete questionnaires regarding treatment techniques and to outline the boost target volumes.[38] The investigators found substantial inconsistency in defining the planning target volume, both in the transverse and longitudinal dimensions. Thus, both a CT scan and a barium swallow should be obtained at the time of radiation therapy simulation.
The integration of other imaging modalities in radiation treatment planning, such as esophageal ultrasound and positron-emission tomography (PET) scan,[39-41] are being investigated actively. In comparing scanning techniques used for treatment planning, Konski and associates reported that PET underestimated the tumor length compared with CT, and ultrasound identified more nodes than either of these technologies.[39]
Recent studies have examined the effectiveness of PET in the staging of esophageal cancer.[40] Flamen et al identified previously undetected metastatic disease using PET in 15% of patients following standard staging that included CT and endoscopy[42]; this increased to 20% in the series by Downey and associates.[43] Given the potential for CT to understage metastatic disease, PET should be part of the standard workup for patients receiving combined-modality therapy.
Tai et al reported the results of 12 Canadian radiation oncologists who drew cervical esophagus target volumes based on the RTOG 94-05 protocol design before and after a one-on-one training session.[44] A pre- and post-training session survey revealed less variability in the longitudinal positions of the target volumes, thereby illustrating the importance of specialized training.
As with surgery, the success of treatment is also related, in part, to patient volume. The 1996-1999 US Patterns of Care study included 414 patients, 49% of whom had squamous cell cancers. These patients were treated with a component of radiation therapy at 59 institutions. Multivariate analysis showed a significant improvement in survival among patients treated at centers where 500 or more new cancer patients were seen annually, compared with patients treated at centers that had fewer than 500 new consultations each year.[12]
New Chemotherapeutic Agents
Since 75% to 80% of patients die of metastatic disease, advances in systemic therapies are needed. The most widely used regimen to be combined with radiation has been 5-FU/cisplatin. New chemotherapeutic regimens are used as preoperative regimens, usually combined with radiation doses of 45 to 50.4 Gy. These regimens include both cytotoxic and targeted small molecules.
Paclitaxel- and docetaxel-based combined-modality regimens have shown encouraging results.[14,15,45,46] The randomized, phase II RTOG E-0113 trial is comparing paclitaxel plus cisplatin, with/or without 5-FU. Other agents such as irinotecan,[16,47,48] trastuzumab (Herceptin),[49] and oxaliplatin (Eloxatin)[50,51] are being used as platforms for new regimens. In addition, ongoing trials are testing the combined use of radiation and irinotecan/cisplatin plus bevacizumab (Avastin) or cetuximab (Erbitux). Whether these investigational approaches offer improved results compared with conventional 5-FU/cisplatin-based combined-modality therapy regimens is not known. The development of the ideal regimens and schedules remains an active area of clinical investigation.
Predictors of Response to Combined-Modality Therapy
Berger et al reported that in patients receiving preoperative combined-modality therapy, a complete response was associated with a significant improvement in survival.[52] Therefore, it would be helpful to predict tumors that have a higher likelihood of responding to combined- modality therapy. Unfortunately, most studies have limited numbers of patients and results are conflicting. Markers such as Bcl-XL,[53] p53,[54] membrane phospholipids,[55] cell division cycle 25B,[56] Ki-67, epidermal growth factor receptor, cyclin D1, vascular endothelial growth factor, microvessel density, thymidylate synthase, dihydropyrimidine dehydrogenase, glutathione s-transferase,[57,58] lymphocytic infiltration,[59]and c-erbB-2[60] have been correlated with response and/or outcome. Molecular markers may help to select treatment in the future.
Studies have produced conflicting data regarding the ability of imaging to predict response or outcome. Kalha and colleagues found that posttreatment endoscopic ultrasound did not accurately predict pathologic response after combined-modality therapy.[61] Lim et al reported that response was the most significant predictive factor for survival.[62] Brink and colleagues reported that the change in standardized uptake value from pretreatment to posttreatment FDG-PET did not correlate with the pathologic response following preoperative combined-modality therapy.[63] However, Wieder et al found that changes in metabolic activity measured by PET 14 days after starting combined-modality therapy in patients with squamous cell cancers correlated with tumor response and patient survival.[18]
Is Surgery Necessary After Combined-Modality Therapy?
Most phase II trials reveal that patients who respond to preoperative combined-modality therapy have a corresponding improvement in outcome.[52,64] Two randomized trials examined whether surgery is necessary after combined-modality therapy.
In the Fédération Francophone de Cancérologie Digestive (FFCD) 9102 trial, 445 patients with clinically resectable, stage (T3-4, N0-1, M0) squamous cell cancer or adenocarcinoma of the esophagus received combined-modality therapy. However, randomization was limited to patients who responded to initial combined-modality therapy-ie, two cycles of 5-FU, cisplatin, and concurrent radiation (either 46 Gy at 2 Gy/d or a split course of 15 Gy on weeks 1 and 3).[65] The 259 patients who had at least a partial response were then randomized to surgery or additional combined-modality therapy, which included three cycles of 5-FU, cisplatin, and concurrent radiation (either 20 Gy at 2 Gy/d or a split course of 15 Gy).
The investigators found no significant difference in 2-year survival (34% vs 40%, P = .56) or median survival (18 vs 19 months) among patients who underwent surgery vs additional combined-modality therapy. Moreover, using the Spitzer index, they found no difference in global quality of life. However, a significantly greater decrease in quality of life (7.52 vs 8.45; P < .01) was observed in the postoperative period among patients who underwent surgery.[66] The data from FFCD 9102 suggested that patients who respond initially to combined-modality therapy should complete combined-modality therapy rather than stop this treatment and undergo surgery.
The German Oesophageal Cancer Study Group compared preoperative combined-modality therapy followed by surgery vs combined-modality therapy given alone.[67] In this trial, 172 eligible patients up to 70 years of age who had locally advanced (T3-4, N0-1, M0) squamous cell cancers of the esophagus were randomized to preoperative therapy (three cycles of 5-FU, leucovorin, etoposide, and cisplatin, followed by concurrent etoposide and cisplatin, plus 40 Gy) followed by surgery vs combined-modality therapy alone (the same chemotherapy, but with the radiation dose increased to 60 to 65 Gy with or without brachytherapy). Despite a decrease in local failure for those who were randomized to preoperative therapy followed by surgery (36% vs 58%, P = .003), there was no significant difference in 3-year survival (31% vs 24%) between the two groups.
Palliation of Dysphagia
Dysphagia is a common problem in esophageal cancer patients-it is the symptom that presents the most frequently, and it may remain problematic up to the time of the patient's death. Coia et al reported that within 2 weeks after the start of combined-modality therapy, 45% of esophageal cancer patients had an improvement in swallowing; by the completion of the sixth week, 83% experienced improvement.[68] Overall, 88% of the patients had improvement in the symptom, with a median time to maximum improvement of 4 weeks. Histology and stage had no impact on the rate of palliation.
Intraluminal brachytherapy is also an effective (albeit more limited) strategy, achieving palliation of dysphagia in 40% to 90% of patients.[69-70] A randomized trial from the Dutch Stent or Intraluminal Radiotherapy for Inoperable Esophageal Cancer (SIREC) study group measured the ability to swallow using various quality-of-life scales in patients treated with stents and others given one 12-Gy fraction of brachytherapy. The team discovered more rapid improvement among those who underwent stent placement, although long-term relief was superior among those given brachytherapy.[21] Median survivals were similar (145 vs 155 days in the stent group and the brachytherapy group, respectively).
Acute and Long-Term Toxicity of Radiation Therapy
Limited toxicity data are available for patients who received conventional doses of radiation therapy. Patients experience lethargy and esophagitis beginning 2 to 3 weeks after starting such treatment; these symptoms usually resolve 1 to 2 weeks following the completion of therapy.
The most carefully documented acute toxicity data in patients receiving combined-modality therapy were reported in the RTOG 85-01 and 94-05 trials discussed previously.[5,9,30] In addition, Gergel and associates examined the effect of radiation on pulmonary function,[71] in patients who received 39.6 Gy of radiation with anterior/posterior fields followed by obliques (total dose: 50.4 Gy) plus concurrent oxaliplatin and 5-FU. Pulmonary function tests performed both preirradiation and a median of 16 days postirradiation revealed significant declines in both diffusing capacity of the lung for CO2 and total lung capacity.
Lee and associates reported that 18% of 61 patients treated with preoperative combined-modality therapy had pulmonary complications.[72] The incidence of such complications was significantly increased among patients in whom 40% or more of lung volume received at least 10 Gy of radiation, compared with those in whom less than 40% of lung volume received at least 10 Gy (35% vs 8%, P = .014). Likewise, the incidence was significantly increased among patients in whom 30% or more of lung volume received at least 15 Gy, compared with those in whom less than 30% of lung volume received at least 15 Gy (33% vs 10%, P =.036).
Radiation Treatment in the Setting of a Tracheoesophageal Fistula
The presence of a malignant tracheoesophageal fistula is an unfavorable prognostic feature. Although experience is very limited, data from the Mayo Clinic suggest that radiation does not necessarily increase the severity of a malignant tracheoesophageal fistula, and it may be administered safely. In this report, 10 patients with a malignant tracheoesophageal fistula received 30 to 66 Gy of external-beam irradiation. The median survival was 5 months, and none of the patients experienced an enlarging or more debilitating fistula following radiation therapy.[73]
Conclusions
The standard nonoperative treatment for patients with locoregional esophageal cancer is combined-modality therapy using 50.4 Gy of radiation therapy plus concurrent 5-FU-based chemotherapy. Dose escalation with either external-beam radiation or brachytherapy does not improve the results when compared with radiation therapy or combined-modality therapy alone. Active areas of clinical investigation include the development of combined-modality therapy regimens using newer systemic agents, the use of FDG-PET to assist in the development of innovative radiation treatment planning techniques, and the identification of prognostic molecular markers. Although controversial, the addition of surgery following primary combined-modality therapy does not appear to improve survival.
Disclosures:
Dr. Minsky is a consultant and speaker for Sanofi-Aventis and Roche; and is a consultant and speaker for, and receives research funding from Genentech and Bristol-Myers Squibb.
References:
1. Pohl H, Welch HG: The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst 97:142-146, 2005.
2. De-Ren S: Ten-year follow-up of esophageal cancer treated by radical radiation therapy: Analysis of 869 patients. Int J Radiat Oncol Biol Phys 16:329-334, 1989.
3. Newaishy GA, Read GA, Duncan W, et al: Results of radical radiotherapy of squamous cell carcinoma of the esophagus. Clin Radiol 33:347-352, 1982.
4. Okawa T, Kita M, Tanaka M, et al: Results of radiotherapy for inoperable locally advanced esophageal cancer. Int J Radiat Oncol Biol Phys 17:49-54, 1989.
5. Herskovic A, Martz LK, Al-Sarraf M, et al: Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med 326:1593-1598, 1992.
6. Al-Sarraf M, Martz K, Herskovic A, et al: Superiority of chemo-radiotherapy (CT-RT) vs radiotherapy (RT) in patients with esophageal cancer. Final report of an Intergroup randomized and confirmed study (abstract 464). Proc Am Soc Clin Oncol 15:206, 1996.
7. Sykes AJ, Burt PA, Slevin NJ, et al: Radical radiotherapy for carcinoma of the oesophagus: An effective alternative to surgery. Radiother Oncol 48:15-21, 1998.
8. Sai H, Mitsumori M, Arai K, et al: Long-term results of definitive radiotherapy for stage I esophageal cancer. Int J Radiat Oncol Biol Phys 62:1339-1344, 2005.
9. Al-Sarraf M, Martz K, Herskovic A, et al: Progress report of combined chemoradiotherapy versus radiotherapy alone in patients with esophageal cancer: An intergroup study. J Clin Oncol 15:277-284, 1997.
10. Cooper JS, Guo MD, Herskovic A, et al: Chemoradiotherapy of locally advanced esophageal cancer. Long-term follow-up of a prospective randomized trial (RTOG 85-01). JAMA 281:1623-1627, 1999.
11. Streeter OE, Martz KL, Gaspar LE, et al: Does race influence survival for esophageal cancer patients treated on the radiation and chemotherapy arm of RTOG # 85-01? Int J Radiat Oncol Biol Phys 44:1047-1052, 1999.
12. Suntharalingam M, Moughhan J, Coia LR, et al: Outcome results of the 1996-1999 patterns of care survey of the national practice for patients receiving radiation therapy for carcinoma of the esophagus. J Clin Oncol 23:2325-2331, 2005.
13. Kenjo M, Oguchi M, Gomi K, et al: Radiation therapy for esophageal cancer: Results of the patterns of care study in Japan 1995-1997. Esophagus 2:77-83, 2005.
14. Bains MS, Stojadinovic A, Minsky B, et al: A phase II trial of preoperative combined-modality therapy for localized esophageal carcinoma: Initial results. J Thorac Cardiovasc Surg 124:270-277, 2002.
15. Goldberg M, Lampert C, Colarusso P, et al: Survival following intensive preoperative combined modality therapy with paclitaxel, cisplatin, 5-fluorouracil, and radiation in resectable esophageal carcinoma: A phase I report (abstract 612). Proc Am Soc Clin Oncol 21:154a, 2002.
16. Ilson DH, Bains M, Kelsen DP, et al: Phase I trial of escalating-dose irinotecan given weekly with cisplatin and concurrent radiotherapy in locally advanced esophageal cancer. J Clin Oncol 21:2926-2932, 2003.
17. Ott K, Fink U, Becker K, et al: Prediction of response to preoperative chemotherapy in gastric carcinoma by metabolic imaging: Results of a prospective trial. J Clin Oncol 21:4604-4610, 2003.
18. Wieder HA, Brucher BL, Zimmermann F, et al: Time course of tumor metabolic activity during chemoradiotherapy of esophageal squamous cell carcinoma and response to treatment. J Clin Oncol 22:900-908, 2004.
19. Kelsen DP, Ginsberg R, Pajak T, et al: Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Engl J Med 339:1979-1984, 1998.
20. Armstrong JG: High dose rate remote afterloading brachytherapy for lung and esophageal cancer. Semin Radiat Oncol 4:270-277, 1993.
21. Homs MY, Essink-Bot ML, Borsboom GJJM, et al: Quality of life after palliative treatment for oesophageal carcinoma-a prospective comparison between stent placement and single dose chemotherapy. Eur J Cancer 40:1862-1871, 2004.
22. Okawa T, Dokiya T, Nishio M, et al: Multi-institutional randomized trial of external radiotherapy with and without intraluminal brachytherapy for esophageal cancer in Japan. Int J Radiat Oncol Biol Phys 45:623-628, 1999.
23. Calais G, Dorval E, Louisot P, et al: Radiotherapy with high dose rate brachytherapy boost and concomitant chemotherapy for stages IIB and III esophageal carcinoma: Results of a pilot study. Int J Radiat Oncol Biol Phys 38:769-775, 1997.
24. Yorozu A, Dokiya T, Oki Y, et al: Curative radiotherapy with high-dose-rate brachytherapy boost for localized esophageal carcinoma: Dose-effect relationship of brachytherapy with the balloon type applicator system. Radiother Oncol 51:133-139, 1999.
25. Gaspar LE, Qian C, Kocha WI, et al: A phase I/II study of external beam radiation, brachytherapy and concurrent chemotherapy in localized cancer of the esophagus (RTOG 92-07): Preliminary toxicity report. Int J Radiat Oncol Biol Phys 37:593-599, 1997.
26. Gaspar LE, Nag S, Herskovic A, et al: American Brachytherapy Society (ABS) consensus guidelines for brachytherapy of esophageal cancer. Int J Radiat Oncol Biol Phys 38:127-132, 1997.
27. Zhang Z, Liao Z, Jin J, et al: Dose response relationship in locoregional control for patients with stage II-III esophageal cancer treated with concurrent chemotherapy and radiotherapy. Int J Radiat Oncol Biol Phys 61:656-664, 2005.
28. Calais G, Jadaud E, Chapet S, et al: High dose radiotherapy (RT) and concomitant chemotherapy for nonresectable esophageal cancer. Results of a phase II study (abstract). Proc Am Soc Clin Oncol 13:197, 1994.
29. Minsky BD, Neuberg D, Kelsen DP, et al: Final report of intergroup trial 0122 (ECOG PE-289, RTOG 90-12): Phase II trial of neoadjuvant chemotherapy plus concurrent chemotherapy and high-dose radiation for squamous cell carcinoma of the esophagus. Int J Radiat Oncol Biol Phys 43:517-523, 1999.
30. Minsky BD, Pajak T, Ginsberg RJ, et al: INT 0123 (RTOG 94-05) phase III trial of combined-modality therapy for esophageal cancer: High dose (64.8 Gy) vs. standard dose (50.4 Gy) radiation therapy. J Clin Oncol 20:1167-1174, 2002.
31. Wang Y, Shi XH, He SQ, et al: Comparison between continuous accelerated hyperfractionated and late-course accelerated hyperfractionated radiotherapy for esophageal carcinoma. Int J Radiat Oncol Biol Phys 54:131-136, 2002.
32. Zhao KL, Shi XH, Jiang GL, et al: Late course accelerated hyperfractionated radiotherapy for localized esophageal carcinoma. Int J Radiat Oncol Biol Phys 60:123-129, 2004.
33. Choi N, Park SD, Lynch T, et al: Twice-daily radiotherapy as concurrent boost technique during chemotherapy cycles in neoadjuvant chemoradiotherapy for resectable esophageal carcinoma: Mature results of a phase II study. Int J Radiat Oncol Biol Phys 60:111-122, 2004.
34. Jacob JH, Seitz JF, Langlois C, et al: Definitive concurrent chemo-radiation therapy (CRT) in squamous cell carcinoma of the esophagus (SCCE): Preliminary results of a French randomized trial comparing standard vs. split course irradiation (FNCLCC-FFCD 9305) (abstract 1035). Proc Am Soc Clin Oncol 18:270a, 1999.
35. Sugahara S, Tokuuye K, Okumura T, et al: Clinical results of proton beam therapy for cancer of the esophagus. Int J Radiat Oncol Biol Phys 61:76-84, 2005.
36. Nutting CM, Bedford JL, Cosgrove VP, et al: A comparison of conformal and intensity-modulated techniques for esophageal radiotherapy. Radiother Oncol 61:157-163, 2001.
37. Phillips TL, Minsky BD, Dicker AP: Cancer of the esophagus, in Leibel SA, Phillips TL (eds): Textbook of Radiation Oncology, 1st ed, pp 601-623. Philadelphia, W.B. Saunders, 1998.
38. Tai P, van Dyk J, Yu E, et al: Variability of target volume delineation in cervical esophageal cancer. Int J Radiat Oncol Biol Phys 42:277-288, 1998.
39. Konski A, Doss M, Milestone B, et al: The integration of 18-fluoro-deoxy-glucose positron emission tomography and endoscopic ultrasound in the treatment-planning process for esophageal carcinoma. Int J Radiat Oncol Biol Phys 61:1123-1128, 2005.
40. Larson SM, Schoder H, Yeung H: Positron emission tomography/computerized tomography functional imaging of esophageal and colorectal cancer. Cancer J 10:243-250, 2004.
41. van Westreenen HL, Heeren PAM, Jager PL, et al: Pitfalls of positive findings in staging esophageal cancer with F-18-fluorodeoxyglucose positron emission tomography. Ann Surg Oncol 10:1105, 2003.
42. Flamen P, van Cutsem E, Lerut T, et al: Positron emission tomography for assessment of the response to induction radiochemotherapy in locally advanced esophageal cancer. Ann Oncol 13:361-368, 2002.
43. Downey RJ, Akhurst T, Ilson D, et al: Whole body 18FDG-PET and the response of esophageal cancer to induction therapy: Results of a prospective trial. J Clin Oncol 21:428-432, 2003.
44. Tai P, Van Dyk J, Battista J, et al: Improving the consistency in cervical esophageal target volume definition by special training. Int J Radiat Oncol Biol Phys 53:766-774, 2002.
45. Nutting CM, Bedford JL, Cosgrove VP, et al: A comparison of conformal and intensity-modulated techniques for oesophageal radiotherapy. Radiother Oncol 61:157-163, 2001.
46. Font A, Garcia-Alfonso P, Arellano A, et al: Preoperative combined multimodal therapy with docetaxel plus 5-fluorouracil and concurrent hyperfractionated radiotherapy for locally advanced esophageal cancer (abstract 2326). Proc Am Soc Clin Oncol 21:128b, 2002.
47. Ilson DH, Minsky B, Kelsen D: Irinotecan cisplatin and radiation in esophageal cancer. Oncology (Williston Park) 16(suppl 5):11-15, 2002.
48. D’Adamo DR, Bains M, Minsky B, et al: A phase I trial of paclitaxel, cisplatin, irinotecan, and concurrent radiation therapy in locally advanced esophageal cancer (abstract 1401). Proc Am Soc Clin Oncol 22:349, 2003.
49. Safran H, DiPetrillo T, Nadeem A, et al: Neoadjuvant herceptin, paclitaxel, cisplatin, and radiation for adenocarcinoma of esophagus: A phase I study (abstract 560). Proc Am Soc Clin Oncol 21:141a, 2002.
50. Khushalani KI, Leichman CG, Proulx G, et al: Oxaliplatin in combination with protracted-infusion fluorouracil and radiation: Report of a clinical trial for patients with esophageal cancer. J Clin Oncol 20:2844-2850, 2002.
51. Chiarion-Sileni V, Corti L, Innocente R, et al: Oxaliplatin (OX) and leucovorin (L) combined with protracted- infusion fluorouracil (F) and radiation (XRT) in locally advanced esophageal cancer (LAEC): A multicentric phase II study (abstract 4071). J Clin Oncol 23(16S):325s, 2005.
52. Berger AC, Farma J, Scott WJ, et al: Complete response to neoadjuvant chemoradiotherapy in esophageal carcinoma is associated with significantly improved survival. J Clin Oncol 23:4330-4337, 2005.
53. Sarbia M, Stahl M, Fink U, et al: Expression of apoptosis-regulating proteins and outcome of esophageal cancer patients treated by combined therapy modalities. Clin Cancer Res 4:2991-2997, 1998.
54. Pomp J, Davelaar J, Blom J, et al: Radiotherapy for oesophagus carcinoma: The impact of p53 on treatment outcome. Radiother Oncol 46:179-184, 1998.
55. Merchant TE, Minsky BD, Lauwers GY, et al: Esophageal cancer phospholipids correlated with histopathologic findings: A 31P NMR study. NMR Biomed 12:184-188, 1999.
56. Kishi K, Doki Y, Miyata H, et al: Prediction of the response to chemoradiation and prognosis in oesophageal squamous cancer (abstract). Br J Surg 89:597-603, 2002.
57. Hironaka S, Hasebe T, Kamijo T, et al: Biopsy specimen microvessel density is a useful prognostic marker in patients with T2-4M0 esophageal cancer treated with chemoradiotherapy. Clin Cancer Res 8:124-130, 2002.
58. Nomiya T, Nemoto K, Miyachi H, et al: Relationships between radiosensitivity and microvascular density in esophageal carcinoma: Significance of hypoxic fraction. Int J Radiat Oncol Biol Phys 58:589-596, 2005.
59. Morita M, Kuwano H, Araki K, et al: Prognostic significance of lymphocytic infiltration following preoperative chemoradiotherapy and hyperthermia for esophageal cancer. Int J Radiat Oncol Biol Phys 49:1259-1266, 2001.
60. Akamatsu M, Matsumoto T, Oka K, et al: c-erbB-2 oncoprotein expression related to chemoradioresistance in esophageal squamous cell carcinoma. Int J Radiat Oncol Biol Phys 57:1323-1327, 2003.
61. Kalha I, Kaw M, Fukami N, et al: The accuracy of endoscopic ultrasound for restaging esophageal carcinoma after chemoradiation therapy. Cancer 101:940-947, 2004.
62. Lim JT, Truong PT, Berthelet E, et al: Endoscopic response predicts for survival and organ preservation after primary chemoradiation for esophageal cancer. Int J Radiat Oncol Biol Phys 57:1328-1335, 2003.
63. Brink I, Hentschel M, Bley TA, et al: Effects of neoadjuvant radio-chemotherapy on 18F-FDG-PET in esophageal carcinoma. Eur J Surg Oncol 30:544-550, 2004.
64. Brucher BL, Stein HJ, Zimmermann F, et al: Responders benefit from neoadjuvant radiochemotherapy in esophageal squamous cell carcinoma: Results of a prospective phase-II trial. Eur J Surg Oncol 30:963-971, 2004.
65. Bedenne L, Michel P, Bouche O, et al: Randomized phase III trial in locally advanced esophageal cancer: Radiochemotherapy followed by surgery versus radiochemotherapy alone (FFCD 9102) (abstract 519). Proc Am Soc Clin Oncol 21:130a, 2002.
66. Bonnetain F, Bedenne L, Michel P,
et al: Definitive results of a comparative longitudinal quality of life study using the Spitzer index in the randomized multicentric phase III trial FFCD 9102 (surgery vs. radiochemotherapy in patients with locally advanced esophageal cancer) (abstract 1002). Proc Am Soc Clin Oncol 22:250, 2003.
67. Stahl M, Stuschke M, Lehmann N, et al: Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 23:2310-2317, 2005.
68. Coia LR, Soffen EM, Schultheiss TE, et al: Swallowing function in patients with esophageal cancer treated with concurrent radiation and chemotherapy. Cancer 71:281-286, 1993.
69. Sur RK, Singh DP, Sharma SC: Radiation therapy of esophageal cancer: Role of high dose rate brachytherapy. Int J Radiat Oncol Biol Phys 22:1043-1046, 1992.
70. Sur RK, Donde B, Levin VC, et al: Fractionated high dose rate intraluminal brachytherapy in palliation of advanced esophageal cancer. Int J Radiat Oncol Biol Phys 40:447-453, 1998.
71. Gergel TJ, Leichman LL, Nava HR, et al: Effect of concurrent radiation therapy and chemotherapy on pulmonary function in patients with esophageal cancer: Dose-volume histogram analysis. Cancer J 8:451-460, 2002.
72. Lee HK, Vaporciyan A, Cox JD, et al: Postoperative pulmonary complications after preoperative chemoradiation for esophageal carcinoma: Correlation with pulmonary dose-volume histogram parameters. Int J Radiat Oncol Biol Phys 57:1317-1322, 2003.
73. Gschossmann JM, Bonner JA, Foote RL, et al: Malignant tracheoesophageal fistula in patients with esophageal cancer. Cancer 72:1513-1521, 1993.
Articles in this issue
almost 20 years ago
Whatever It Takesalmost 20 years ago
Docetaxel Approved for Advanced Stomach Canceralmost 20 years ago
Adjuvant Therapy for Colorectal Cancer: Yesterday, Today, and Tomorrowalmost 20 years ago
Rituximab Effective in Treating Chronic Graft-vs-Host Diseasealmost 20 years ago
Fertility-Preserving Options for Cervical Canceralmost 20 years ago
Commentary (Putnam): Primary Combined-Modality Therapy for Esophageal Canceralmost 20 years ago
Commentary (Kuban): Permanent Prostate BrachytherapyNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.