- Oncology Vol 27 No 12
- Volume 27
- Issue 12
Proton Radiotherapy for Prostate Cancer: How Did We Get Here, and Where Do We Go From Here?
Despite the promise of proton therapy, comparative evidence has yet to definitively demonstrate its clinical benefit over other forms of contemporary radiation for prostate cancer.
Proton radiotherapy is an important technology for cancer treatment. By reducing and even eliminating unwanted radiation dose to surrounding tissue, proton therapy has the potential to lessen the toxicity of radiotherapy. The promise of precisely delivered radiation doses has led to the adoption of proton radiotherapy in selected centers across the United States.[1] Currently there are 11 proton centers in operation, with 8 centers under construction and 1 in planning. There are 11 additional smaller superconducting synchrocyclotron proton radiotherapy machines currently in development.[2] However, despite the promise of proton therapy, comparative evidence has yet to definitively demonstrate its clinical benefit over other forms of contemporary radiation for prostate cancer.
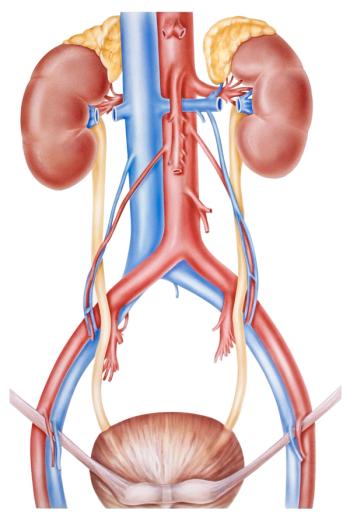
Following the first postulation by Wilson in 1946[3] that high-energy protons could penetrate into tissue to a depth that could potentially treat small volumes of tumor within the body, prostate cancer was one of the earliest organ sites to be targeted by proton radiotherapy.[4] In-silico studies comparing the theoretical distribution of radiation dose for prostate intensity-modulated radiotherapy (IMRT) and proton radiotherapy have suggested that the benefit from older 3-D conformal proton radiotherapy was limited to a reduction in low and moderate doses of radiotherapy to the bladder and rectum.[5-7] However, newer intensity-modulated proton radiotherapy (IMPT), currently in the earliest phases of adoption,[8] may allow for even more significant reduction of dose to surrounding normal tissue.[6]
Clinically, there have been multiple retrospective and prospective single-arm studies showing excellent outcomes for both proton therapy[9,10] and IMRT[11,12] in patients with prostate cancer. Comparative claims-based analyses[13-15] and retrospective quality-of-life studies[16] have shown mixed results for proton radiotherapy compared with IMRT. Certainly these studies have limitations-and randomized trial data are sorely needed. The definitive randomized trial of proton radiotherapy vs IMRT for prostate cancer, PARTIQoL,[17] led by Massachusetts General Hospital and the University of Pennsylvania, is now actively accruing.[18]
Because of the current lack of strong clinical evidence supporting the relative benefit of proton radiotherapy compared with IMRT in the treatment of prostate cancer, some private insurers have announced that they will no longer cover proton radiotherapy for prostate cancer.[19] Responding differently to the same circumstances, the American Society for Radiation Oncology (ASTRO), as part of the American Board of Internal Medicine’s Choosing Wisely campaign, has recommended that patients who receive proton radiotherapy for prostate cancer enroll in a clinical trial or prospective registry.[20] Therefore, in contrast to insurers, who increasingly are not covering proton therapy for prostate cancer, ASTRO continues to strongly support coverage with evidence development,[21] recognizing that proton beam therapy is not a new technology, and that insurance coverage of prostate cancer patients treated on trials or within prospective registries is important to the gathering of comparative effectiveness data. The question thus arises: How did we get here?
Steinberg and Konski have outlined the historical, regulatory, and economic factors that have contributed to the proliferation of proton radiotherapy in the United States.[22] Beyond the practical reasons they offer for why proton radiotherapy proliferated for prostate cancer, another factor to consider is that innovation in radiation technology occurs at a fast pace, without a clear framework for investigating whether the innovations translate to incremental, as well as measurable and clinically meaningful, improvements in patient outcomes. One approach to determining Medicare coverage and reimbursement for new technologies was recently proposed. Medicare would assign new medical technologies to one of three payment categories based on comparative effectiveness evidence. The authors write: “After an initial 3-year period, if services with insufficient evidence do not provide additional evidence demonstrating superior comparative clinical effectiveness, payment would drop to reference pricing levels.”[23] The authors highlighted the example of IMRT as a perfect setting for testing this approach. However, for clinical studies examining the effectiveness and toxicity of treatments, especially in prostate cancer, 3 years is simply too short. This proposal is only one of many such proposals under discussion. Clearly there is a need for intensive dialogue around how best to generate evidence for new technologies in radiation therapy.
The problem of rapid innovation outpacing comparative evidence and broad consensus on best practice is hardly unique to radiation oncology,[24,25] or even to medicine.[26] It may be a hallmark of truly transformative technology that the implications of that technology are impossible to predict until it is adopted. Realizing this, where can we go from here? Will the continued cycle of innovation, investment, and adoption of new radiation technology always outstrip our ability to evaluate the technique clinically in a timely manner? At the very least, it is time for radiation oncology to strive to perform more timely and more widespread clinical investigations of new radiation technologies. Specific funding for evaluation of the clinical comparative effectiveness of new radiation modalities is sorely needed. Currently, only 1.6% of National Institutes of Health (NIH) funding supports radiation oncology research,[27] and of this amount, only 7.6% (less than 0.1% of overall NIH funding) supports clinical investigations, presumably the category of research into which the testing of the comparative effectiveness of new radiation technologies would fall. The importance of federal funding for research specific to radiation technology is crucial in the absence of industry-sponsored randomized controlled trials (RCTs) for radiotherapy (RCTs investigating radiation alone account for only 4% of all industry-funded trials in a recent survey[28]). Because radiotherapy affects roughly two-thirds of all patients with cancer,[29] funding of comparative effectiveness trials and prospective outcomes registries for radiotherapy is critical for all cancer patients.
We are confident that the field of radiation oncology will continue to innovate. However, increasing funding for radiation-specific comparative effectiveness research and continued coverage of promising therapies that are being evaluated in a timely and rigorous prospective manner is critical if we are to balance innovation and promise with data and value.
Financial Disclosure:Proton radiotherapy is available at Massachusetts General Hospital (JAE) and at the Abramson Cancer Center at the University of Pennsylvania (JEB), but not at the Yale School of Medicine (JBY).
References:
1. Hoppe B, Henderson R, Mendenhall WM, et al. Proton therapy for prostate cancer. Oncology (Williston Park). 2011;25:644-50, 52.
2. Mevion S250 Installation. 2013 [cited 2013 October 1]. Available from:
3. Wilson RR. Radiological use of fast protons. Radiology. 1946;47:487-91.
4. Munzenrider JE, Shipley WU, Verhey LJ. Future prospects of radiation therapy with protons. Semin Oncol. 1981;8:110-24.
5. Vargas C, Fryer A, Mahajan C, et al. Dose-volume comparison of proton therapy and intensity-modulated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70:744-51.
6. Trofimov A, Nguyen PL, Coen JJ, et al. Radiotherapy treatment of early-stage prostate cancer with IMRT and protons: a treatment planning comparison. Int J Radiat Oncol Biol Phys. 2007;69:444-53.
7. Mock U, Bogner J, Georg D, et al. Comparative treatment planning on localized prostate carcinoma conformal photon- versus proton-based radiotherapy. Strahlenther Onkol. 2005;181:448-55.
8. Efstathiou JA, Gray PJ, Zietman AL. Proton beam therapy and localised prostate cancer: current status and controversies. Br J Cancer. 2013;108:1225-30.
9. Hoppe BS, Nichols RC, Henderson RH, et al. Erectile function, incontinence, and other quality of life outcomes following proton therapy for prostate cancer in men 60 years old and younger. Cancer. 2012;118:4619-26.
10. Coen JJ, Paly JJ, Niemierko A, et al. Long-term quality of life outcome after proton beam monotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82:e201-9.
11. Ghadjar P, Jackson A, Spratt DE, et al. Patterns and predictors of amelioration of genitourinary toxicity after high-dose intensity-modulated radiation therapy for localized prostate cancer: implications for defining postradiotherapy urinary toxicity. Eur Urol. 2013;64:931-8.
12. Fonteyne V, Villeirs G, Lumen N, De Meerleer G. Urinary toxicity after high dose intensity modulated radiotherapy as primary therapy for prostate cancer. Radiother Oncol. 2009;92:42-7.
13. Kim S, Shen S, Moore DF, et al. Late gastrointestinal toxicities following radiation therapy for prostate cancer. Eur Urol. 2011;60:908-16.
14. Sheets NC, Goldin GH, Meyer AM, et al. Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer. JAMA. 2012;307:1611-20.
15. Yu JB, Soulos PR, Herrin J, et al. Proton versus intensity-modulated radiotherapy for prostate cancer: patterns of care and early toxicity. J Natl Cancer Inst. 2013;105:25-32.
16. Gray PJ, Paly JJ, Yeap BY, et al. Patient-reported outcomes after 3-dimensional conformal, intensity-modulated, or proton beam radiotherapy for localized prostate cancer. Cancer. 2013;119:1729-35.
17. Proton therapy vs. IMRT for low or intermediate risk prostate cancer (PARTIQoL). 2013 [cited 2013 October 7]. Available from:
18. Bekelman JE, Hahn SM. The body of evidence for advanced technology in radiation oncology. J Natl Cancer Inst. 2013;105:6-7.
19. Winslow R, Martin T. Prostate-cancer therapy comes under attack. The Wall Street Journal. 2013 August 20. 2-13;Sect. B1.
20. ASTRO. Choosing wisely-five things physicians and patients should question. 2013 [cited 2013 October 3]. Available from:
21. ASTRO. ASTRO position statement: use of proton beam therapy for prostate cancer. February 2013. 2013 [cited 2013 October 7]. Available from:
22. Steinberg ML, Konski A. Proton beam therapy and the convoluted pathway to incorporating emerging technology into routine medical care in the United States. Cancer J. 2009;15:333-8.
23. Pearson SD, Bach PB. How Medicare could use comparative effectiveness research in deciding on new coverage and reimbursement. Health Affairs. 2010;29:1796-804.
24. Krill LS, Bristow RE. Robotic surgery: gynecologic oncology. Cancer J. 2013;19:167-76.
25. Kantarjian HM, Fojo T, Mathisen M, Zwelling LA. Cancer drugs in the United States: justum pretium-the just price. J Clin Oncol. 2013;31:3600-4.
26. Singer N. Technology outpaces privacy (yet again). The New York Times. 2010 December 12;Sect. 1.
27. Steinberg M, McBride WH, Vlashi E, Pajonk F. National Institutes of Health funding in radiation oncology: a snapshot. Int J Radiat Oncol Biol Phys. 2013;86:234-40.
28. Lloyd S, Buscariollo D, Gross CP, et al. The funding of phase III clinical trials examining radiation compared with that of other modalities. Int J Radiat Oncol Biol Phys. 2012;84:S44-5.
29. ASTRO. Fast facts about radiation therapy. 2013 [cited 2013 October 7]. Available from:
Articles in this issue
about 12 years ago
POEMS Syndrome: Still an Enigma?about 12 years ago
POEMS Syndrome: What's in a Name?about 12 years ago
Roundtable: the ACA and Cancer CareNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.

















































































