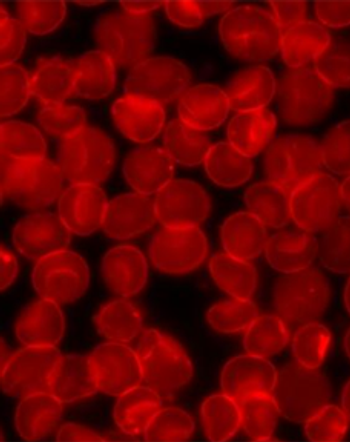
Reduced-Dose Ibrutinib Remains Effective in CLL
A study shows that lower doses of ibrutinib after a full-dose cycle may be enough for continued biological activity.
A phase I study evaluated a reduction in ibrutinib dose for patients with chronic lymphocytic leukemia (CLL) and showed that a lower dose after 1 full-dose cycle was enough to maintain biologic activity.
Ibrutinib is currently given at a dose of 420 mg per day. This study looked at reduction from 420 mg per day to 280 mg per day to 140 mg per day over three 28-day cycles.
Lisa S. Chen, PhD, of the department of experimental therapeutics at The University of Texas MD Anderson Cancer Center, and colleagues had previously shown a decrease in BTK protein levels in CLL cells after one cycle of ibrutinib, suggesting that ibrutinib dose could be lowered after completion of the first cycle without a loss of effect.
Dose reductions are desirable because of the possibility of indefinite administration of the drug in patients who respond, financial toxicity related to the cost of the drug and CLL management, and associated adverse events.
“Ibrutinib has already become a routine part of the CLL treatment paradigm, replacing chemoimmunotherapy in some situations, based on its efficacy and tolerable side effect profile,” said Paul M. Barr, MD, of University of Rochester Medical Center, who was not involved with the study. “Given this widespread use, further improving how we administer ibrutinib and potentially BTK inhibitors under development may have a significant impact on patient care.”
To further test this, Chen and colleagues
Chen and colleagues found that plasma and intracellular levels of ibrutinib were dose dependent. However, even the 140 mg per day dose was sufficient to occupy on average more than 95% of BTK protein. In addition, BTK downstream signaling inhibition was maintained at the lowest dose tested, and comparable reductions in total and phosphor-BTK protein levels were found across all three doses.
Also similar were reduction in plasma chemokine CCL3 and CCL4 levels, considered biomarkers of drug response. CCL3 levels averaged between 53% and 57% of pretreatment levels, while CCL4 averaged between 33% and 39%.
Commenting on the results of the study, Anthony Mato, MD, MSCE, director of the CLL program at the Memorial Sloan Kettering Cancer Center, advised caution and emphasized that these results are hypothesis-generating only and do not call for administration of ibrutinib at reduced doses in clinical practice.
“What this paper brings to the table is the understanding that blocking BTK at a higher dose initially is important to saturate BTK or eliminate many of the malignant cells, and as that number comes down, a lower dose may be appropriate,” said Mato, who was involved in
Any consideration of use of lower doses of ibrutinib in clinical practice, Mato said, must be preceded by large, multicenter, randomized clinical trials.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.