Rigosertib May Benefit Some Patients with Myelodysplastic Syndromes
Although there are currently no approved second-line therapies for high-risk MDS, researchers have discovered that rigosertib has the potential to benefit this population of patients.
A new phase 1/2, dose-escalating
The study, which was published in Leukemia Research, included 22 patients with higher-risk myelodysplastic syndromes. The researchers found that those who responded or had stable disease experienced 1 year longer survival compared with nonresponders. The investigators also determined the optimal dose of rigosertib was 1,375 mg/m2/day.
“This study suggests that patients with refractory acute leukemia should be referred for clinical trial,” said Steven Fruchtman, MD, who is chief medical officer and senior vice president of Onconova Therapeutics, Newtown, Pennsylvania. “The outcome is not necessarily dismal. We hope to translate these findings into strategies to prolong survival in addition to seeing responses.”
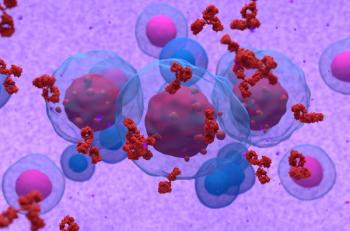
In this current study, nine patients had higher-risk MDS and 13 had acute myeloid leukemia (AML) and had relapsed or were refractory to standard therapy. The researchers noted that currently there are no approved second-line therapies for these patients. The subjects in the study received between 3-day and 7-day continuous intravenous infusions of rigosertib, which inhibits Ras-effector pathways that interact with the Ras-binding domains.
The researchers conducted a dose escalation regimen following a Fibonacci scheme. The agent was administered at doses of 650-1,700 mg/m2/day in 14-day cycles. The team found that rigosertib was well tolerated for up to 23 cycles. There were no treatment-related deaths and overall hematologic toxicity was acceptable, despite significant baseline cytopenias. The study showed that only 18% of the patients suffered serious adverse events (AEs). The most common AEs were fatigue, diarrhea, pyrexia, dyspnea, insomnia, and anemia.
In a subset of patients, rigosertib exhibited biologic activity and there was a reduction or stabilization of bone marrow blasts and improved peripheral blood counts. The study showed that 10 (53%) of 19 evaluable patients demonstrated bone marrow/peripheral blood responses or stable disease. Among these 10 patients, four with MDS and one with AML demonstrated responses, and three with MDS and two with AML had stable disease. When the team examined survival rates they found that the responders had a median survival of 15.7 months. However, the median survival was only 2.0 months for nonresponders.
Currently, Onconova Therapeutics is developing rigosertib as a treatment for patients with higher-risk MDS. However, the novel mechanism of action for rigosertib may have application to other solid and liquid tumors, according to the company. “Depending on the availability of funding, we plan to study the combination of azacitidine plus oral rigosertib versus azacidine plus placebo in elderly AML,” said Dr. Fruchtman.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.