Study Identifies Factors Influencing Variability in Postthaw Product Quality of Donor Stem Cells
Researchers indicated these study findings “could be a note of caution for transplant centers to not take for granted that the frozen product they have received will show perfect recovery once thawed.”
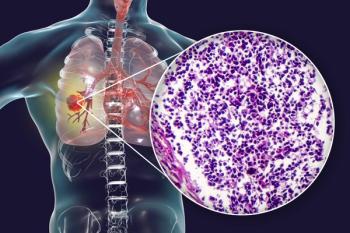
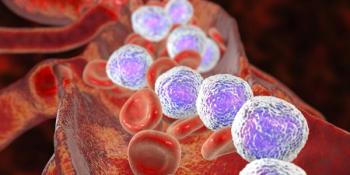
A study published in Blood Advances suggested that although postthaw CD34+ cell recovery and viability of cryopreserved allogeneic hemopoietic progenitor cell (HPC) is typically acceptable, there is a significant risk of poor postthaw product quality, associated with prolonged storage time, higher white cell count, and complex product manipulation precryopreservation.1
Given these findings, researchers suggested that transplant centers should request a higher CD34+ cell dose from donors whose products are to be cryopreserved and that optimization of precryopreservation factors, such as transit time and white cell count, during storage may improve postthaw yield.
“Prior to COVID-19, the donor and transplant systems were well coordinated and effective. Now, with irregular flights and closed borders, travel and transportation are not assured,” lead study author Duncan Purtill, MD, of Fiona Stanley Hospital in Western Australia, said in a press release.2
“Five to 7 days before stem cell transplant, the recipient usually starts chemotherapy to remove all their bone marrow cells,” Purtill continued. “Without a healthy transplant to replace the cells on the same day, they would be left with no functioning bone marrow, which would of course be very high risk and carry a poor prognosis. Life literally depends on the safe arrival and immediate infusion of stem cells.”
Using 305 allogeneic HPC products cryopreserved at 9 laboratories across Australia, researchers sought to understand the postthaw CD34+ cell recovery. Of note, all products were cryopreserved in controlled rate freezers, and CD34+ cell quantitation was performed with single-platform assays.
Median postthaw CD34+ cell recovery was 76% and ranged from 6% to 122%. Overall, 47 products (15%) had 50% or less CD34+ recovery after thawing and 4 products (1%) had 20% or less, though there was no apparent enumeration, transportation, or processing mishap to explain this poor postthaw recovery.
On univariate linear regression analysis, a low association was observed between CD34+ cell recovery and transit time, initial white cell count, product type, and precryopreservation manipulation, while no correlation was observed with initial product volume. However, on multivariate analysis, only transit time, initial white cell count, and manipulation status were associated with CD34+ cell recovery with statistical significance.
Further, postthaw CD34+ cell viability, or the percentage of viable events within the CD34+ cell gate, was only available for 139 samples from 6 centers. Both transit time and white cell count were again associated with postthaw CD34+ cell viability.
“It seems that there is variability in recovery and more work needs to be done to determine why,” Duncan Purtill, MD, of Fiona Stanley Hospital in Western Australia, said in the release. “When we freeze stem cells and then thaw them afterwards, we sometimes get unexpected results. In this study we identified some possible factors influencing that variability.”
Importantly though, researchers explained that the factors identified in this study accounted for only a small proportion of the overall variability in CD34+ cell recovery (r2 = 0.121). Therefore, as was recently recommended by the World Marrow Donor Association, the investigators indicated that transplant centers should be aware of the risk of unexpectedly poor postthaw CD34+ cell recovery and take steps to prevent it, including examination of thawed pilot vials before the commencement of conditioning therapy.
“Our findings could be a note of caution for transplant centers to not take for granted that the frozen product they have received will show perfect recovery once thawed,” said Purtill. “I hope centers will insist on receiving a pilot vial which has been frozen and transported in the same way. They can assess the pilot vial to determine its viability before they use the full product and start chemotherapy for the patient.”
References:
1. Purtill D, Antonenas V, Chiappini P, et al. Variable CD34+ recovery of cryopreserved allogeneic HPC products: transplant implications during the COVID-19 pandemic. Blood Advances. doi: 10.1182/bloodadvances.2020002431
2. Study: Cryopreservation Associated with Loss of Quality in Donor Stem Cell Products [news release]. Washington. Published September 4, 2020. Accessed September 16, 2020. https://www.hematology.org/newsroom/press-releases/2020/cryopreservation-associated-with-loss-of-quality-in-donor-stem-cell-products
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.