- ONCOLOGY Vol 21 No 1
- Volume 21
- Issue 1
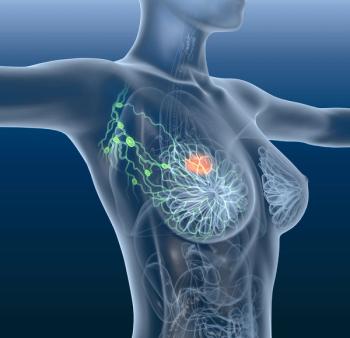
Tailoring Endocrine Therapy in Breast Cancer Patients
The majority of invasive breast cancer patients present with hormone receptor-positive disease, and modulation of estrogen receptor (ER) activation is an essential component of systemic adjuvant therapy for these women. While tamoxifen has traditionally been the primary adjuvant endocrine therapy for all ER-positive women, recent trials evaluating the use of aromatase inhibitors (AIs) have challenged this standard in postmenopausal women, and ongoing trials are examining the optimal use of endocrine therapy in younger women. Issues regarding the optimal approach to endocrine therapy in both pre- and postmenopausal women are examined in this review.
Nearly 215,000 cases of invasive breast cancer are diagnosed in the United States each year, approximately three-quarters of which are estrogen receptor (ER) or progesterone receptor-positive.[1] Our knowledge of the benefits of interfering with the ER-signaling pathway and treatment options for those with hormone receptor-positive disease have improved substantially with the development of aromatase inhibitors (AIs). For younger premenopausal women, the optimal use of tamoxifen with ovarian suppression/ovarian ablation (OS/OA) remains unresolved. Cianfrocca and Wolff provide a comprehensive and thoughtful review of these issues, highlighting current and ongoing studies of endocrine therapies in the adjuvant setting for both patient populations.[2]
Aromatase Inhibitors, Tamoxifen, or Both?
A large collective body of information has shown that (1) ER signaling is important in breast cancer growth and spread, (2) hormone receptor status is a strong predictor for endocrine therapy effectiveness, (3) endocrine therapy is only effective in those who are hormone receptor-positive (although a subset of these patients may exhibit de novo or acquired resistance), and (4) endocrine therapy can dramatically decrease breast cancer recurrence and death. While 5 years of adjuvant tamoxifen has been considered the treatment standard based on individual studies and the Early Breast Cancer Trialists' Collaborative Group (EBCTCG) overview analyses,[3] recent studies suggest a superior disease-free survival with AI therapy.
The first and largest of these studies, the Arimidex, Tamoxifen, Alone or in Combination (ATAC) trial, was a direct comparison of anastrozole (Arimidex) and tamoxifen and currently has over 5 years of follow-up. The Breast International Group (BIG) 1-98 trial shows similar results with letrozole (Femara), although this trial is less mature.[4,5] Alternatively, the sequential treatment strategies of 2, 3, or 5 years of tamoxifen followed by an AI have all shown a disease-free survival benefit compared with 5 years of tamoxifen.[6,7] One of these studies (the Arimidex-Nolvadex [ARNO] trial) has shown a survival benefit at 30.1 months.[8]
Thus, there is little controversy that postmenopausal women with hormone receptor-positive breast cancer should receive an aromatase inhibitor as part of their adjuvant therapy. What remains unclear is the optimal sequence of these therapies. Preclinical data suggest that tamoxifen may be more beneficial used early in the sequence of antiestrogen therapy, as xenografts selected for resistance to tamoxifen will respond to an aromatase inhibitor but AI-resistant tumors do not respond to tamoxifen.[9,10] However, direct comparisons of AI therapy upfront vs following tamoxifen have not yet matured and await results from BIG 1-98.
Proponents of upfront aromatase inhibitors argue that patients should not be denied the small but significant benefit of an AI early in the course of therapy for this theoretical advantage of starting with tamoxifen. In addition, because all crossover studies reported to date randomized patients after an initial treatment period with tamoxifen, those patients who may have had more aggressive disease and had early recurrences would have already been excluded. It is certainly reasonable to begin with an aromatase inhibitor for postmenopausal hormone-sensitive breast cancer, particularly when the patient is at higher risk for early recurrence. For each patient, careful consideration should be given to the differing short- and long-term toxicities of these two classes of agents. In the future, it is likely that tumor and host profiling studies will help guide treatment on a more individual basis.
A number of critical questions remain. What do we recommend to women who have completed 5 years of an AI or a combination of tamoxifen and an AI for 5 years? If additional therapy is chosen, what should it be? Are there significant differences among the third-generation AIs? It seems likely that 3 years of an AI, even when preceded by tamoxifen, may not be adequate therapy for those with higher-risk disease. Current studies do not address these questions, and rerandomization beyond 5 years of hormonal therapy is again necessary, as extrapolation from 10-year tamoxifen data may not be applicable. In addition, the ongoing MA.27 trial should provide direct comparative data for 5 years of adjuvant anastrozole vs exemestane (Aromasin) therapy.
Endocrine Therapy in Premenopausal Women
For younger women with hormone receptor-positive breast cancer, endocrine therapy is clearly effective, and understanding the optimal treatment regimen is critical. There are no prospective, randomized trials that address the role of ovarian ablation in the context of current treatment regimens. Older studies show convincingly that OA/OS is equivalent to CMF-based chemotherapy (cyclophosphamide, methotrexate, fluorouracil) and offers benefit similar to that of tamoxifen in premenopausal patients with hormone receptor-positive disease. However, common practice in North America is to offer these patients chemotherapy followed by tamoxifen, and the additional benefit of OA/OS in this situation is unclear.[11] Furthermore, the benefit of OA/OS compared with anthracycline- and taxane-based chemotherapy has not been explored.
Several ongoing studies will address these issues prospectively. The largest study, the Suppression of Ovarian Function Trial (SOFT), will randomize premenopausal women with hormone receptor-positive disease who may have received adjuvant chemotherapy with tamoxifen, tamoxifen plus OA for 5 years, or exemestane plus OA for 5 years.
Available data suggest that women under age 40 may gain the most benefit from OA/OS.[11,12] Ironically, these younger patients are subject to other risksthe consequences of OA/OS may prevent them from completing their families, and they experience the most long-term morbidity related to bone and the cardiovascular system. However, the risk-benefit ratio clearly depends on the likelihood of benefit. For ER-positive patients at high risk of recurrence who do not become postmenopausal after chemotherapy, it is not unreasonable to consider temporary ovarian suppression with a gonadotropin agonist. For lower-risk ER-positive patients whose comorbidities preclude the use of chemotherapy or who choose not to have it, OA/OS remains a reasonable addition to tamoxifen. Ideally, all patients not at these extremes should consider participation in a clinical trial if possible.
Future Directions
For both premenopausal and postmenopausal women, a better understanding of the molecular mechanisms of response and resistance will help oncologists tailor treatment. We have known for many years that the hormone receptor-positive phenotype does not translate directly into a hormone-responsive phenotype. Recent gene-expression profiling studies have begun to clarify this heterogeneity.[13] Coexpressed growth factor receptors may reduce dependence on the estrogen-receptor pathway and lead to antiestrogen resistance.[14] In addition, certain germline polymorphisms and mutations alter antiestrogen metabolism and toxicity.[15,16] Increasing knowledge of both tumor and host variables will help guide treatment of hormone receptor-positive breast cancer in the future.
Gina G. Chung, md
Lyndsay N. Harris, md
Disclosures:
The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Jemal A, Siegel R, Ward E, et al: Cancer statistics, 2006. CA Cancer J Clin 56:106-130, 2006.
2. Cianfrocca M, Wolff AC: Optimizing endocrine therapy for premenopausal and postmenopausal women with breast cancer. Oncology (Williston Park), 21:63-69, 2007.
3. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomized trials. Lancet 365:1687-1717, 2005.
4. Howell A, Cuzick J, Baum M, et al: Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completeion of 5 years' adjuvant treatment for breast cancer. Lancet 365:60-62, 2005.
5. Thurlimann B, Keshaviah A, Coates AS, et al: A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 353:2747-2757, 2005.
6. Coombes R, Hall E, Gibson L, et al: A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 350:1081-1092, 2004.
7. Goss PE, Ingle JN, Martino S, et al: Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: Updated findings from NCIC CTG MA.17. J Natl Cancer Inst 97:1262-1271, 2005.
8. Kaufmann M, Jonat W, Hilfrich H, et al: Survival benefit of switching to anastrazole after 2 years treatment with tamoxifen versus continued tamoxifen therapy: The ARNO 95 study (abstract 547). J Clin Oncol 24(18S):14s, 2006.
9. Long BJ, Jelovac D, Thiantanawat A, et al: The effect of second-line antiestrogen therapy on breast tumor growth after first-line treatment with the aromatase inhibitor letrozole: long-term studies using the intratumoral aromatase postmenopausal breast cancer model. Clin Cancer Res 8:2378-2388, 2002.
10. Long BJ, Jelovac D, Handratta V, et al: Therapeutic strategies using the aromatase inhibitor letrozole and tamoxifen in a breast cancer model. J Natl Cancer Inst 96:456-465, 2004.
11. Davidson NE, O'Neill AM, Vukov AM, et al: Chemoendocrine therapy for premenopausal women with axillary lymph node-positive, steroid hormone receptor-positive breast cancer: Results from INT 0101 (E5188). J Clin Oncol 23:5973-5982, 2005.
12. Gnant M, Greil R, Kubista E, et al: The impact of treatment-induced amenorrhea on survival of premenopausal patients with endocrine-responsive breast cancer: 10-year results of ABCSG-05 (CMF vs. goserelin+tamoxifen) (abstract 17). Proceedings of the 29th Annual San Antonio Breast Cancer Symposium, San Antonio, Texas, December 14-17, 2006.
13. Paik S, Shak S, Tang G, et al: A multigene assay to predict recurrence of tamoxifen-treated, node-degative breast cancer. N Engl J Med 351:2817-2826, 2004.
14. Ellis MJ, Coop A, Singh B, et al: Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: Evidence from a phase III randomized trial. J Clin Oncol 19:3808-3816, 2001.
15. Jin Y, Desta Z, Stearns V, et al: CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 97:30-39, 2005.
16. Abramson N, Costantino JP, Garber JE, et al: Effect of Factor V Leiden and prothrombin G20210->A mutations on thromboembolic risk in the national surgical adjuvant breast and bowel project breast cancer prevention trial. J Natl Cancer Inst 98:904-910, 2006.
Articles in this issue
about 19 years ago
'Repairing the World'about 19 years ago
Evolving Classification and Management of Myelodysplastic Syndromeabout 19 years ago
The Significance of Anemia in Elderly Patients with Cancerabout 19 years ago
Optimizing Endocrine Therapy for Breast Cancer: 'Miles to Go'about 19 years ago
Landmark Lapatinib Data Publishedabout 19 years ago
Practice Guidelines Released for HER2 Testing in Breast Cancerabout 19 years ago
Age Matters... Or Does It?about 19 years ago
New Vaccine Helps Fight Colorectal Cancer in British Studyabout 19 years ago
Targeted Focal Therapy in Prostate Cancer: Too Soon for a Paradigm Shiftabout 19 years ago
New Therapeutics for Soft-Tissue Sarcomas in AdultsNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.