Will New Focus on Lenalidomide Risks Reveal More About Its Benefits?
There's reason to question whether lenalidomide is the cause of secondary cancers in patients who take it as an adjuvant. But new scrutiny may help to clarify how it acts against the primary.
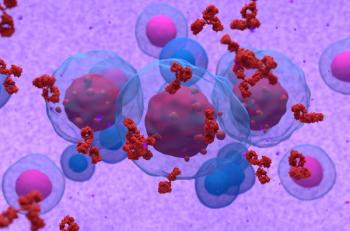
It's cold comfort to patients who have been taking lenalidomide (Revlimid) for myeloma or myelodysplastic syndrome (MDS), but the hard truth of cancer biology is that steps forward often begin with what appear to be setbacks. In this case, the FDA on April 8 issued a scary announcement that the drug which can put them into remission may also cause second primary cancers.
5q- syndrome bone marrow histology with typical abnormal megakaryocytes; source: Jon Salisbury, Wikimedia Commons
The question is: why? What is going on with this immune-system modulator (a chemical relative of thalidomide) whose mode of action is both broad and poorly understood? In deciding to study the drug's safety without advising restrictions for its use in blood-related cancers, the agency tips its hat to both the drug's effectiveness and to ongoing studies that may yet reveal how we can capitalize on its effects to find better alternatives.
Second cancer risk difficult to assess
Lenalidomide is approved for treatment of multiple myeloma, in combination with dexamethasone, for patients who have had one prior treatment. It's also approved for a subset of MDS patients. On April 8, the FDA announced that clinical trials "have found that patients treated with Revlimid (lenalidomide) may be at an increased risk of developing new types of cancer compared to patients who did not take the drug.” The studies involved all tested lenalidomide as an adjuvant either to stem cells or DNA-damaging drugs such as melphalan, not as a single agent. So it is not clear which intervention deserves the blame for the secondary cancers. (No studies have implicated thalidomide, but the FDA is also scrutinizing its safety record because the two drugs are chemically similar.)
Immune and oncologic effects
There is no question that, as an anti-cancer drug, lenalidomide is a cannon rather than a sniper. Setting aside its effects on the immune system (which may be just as important as its direct effects on cancer cells), in vitro and mouse studies reveal that it inhibits cell death, affects adhesion and angiogenesis, and normalizes the ability of stromal cells to support the growth of normal progenitor cells. In patients who respond to lenalidomide, it dramatically reduces the proportion of myeloid cells with the 5q deletion. Not surprisingly, this affects phenomena specific to what's missing from the deleted region of chromosome 5q, including two proteins involved in the cell cycle and, intriguingly, the tumor suppressor produced by the called gene SPARC.
Which of these actions is most important to remission? And if it is triggering secondary cancers, how? Answers are likely to emerge from further increases in attention to the drug.
MDS patients who respond to lenalidomide usually relapse within 2 or 3 years. They provide compelling human evidence to support the stem-cell hypothesis of cancer recurrence-that relapses are due to a population of treatment-resistant stem cells. A multicenter
When it transforms to leukemia, MDS usually evolves into acute myelogenous leukemia. But hematologists at the Lehigh Valley Hospital in Pennsylvania have recently reported on two cytogenetically similar cases in which
New revelations about the effects and risks of lenalidomide are certain to emerge next week at the
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.