Women With Essential Thrombocythemia Live Longer Than Men
A new study including two separate cohorts found that male gender is a significant risk factor for mortality in patients with essential thrombocythemia. Gender may play a bigger role than thrombosis history in determining risk.
A new study found that male gender is a significant risk factor for mortality in patients with essential thrombocythemia (ET). Gender may play a bigger role than thrombosis history in determining risk.
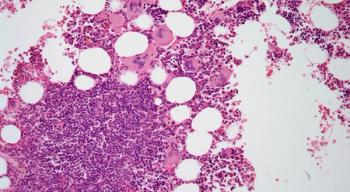
ET is considered a myeloproliferative neoplasm, and is similar in phenotype and molecular characterization to polycythemia vera (PV) and primary myelofibrosis (PMF). “Survival in these JAK2 mutation-enriched myeloproliferative neoplasms is significantly worse than the sex- and age-matched general population,” wrote study authors led by Ayalew Tefferi, MD, of the Mayo Clinic in Rochester, Minnesota.
Recent research has suggested that gender, along with a number of other factors, may be an important determinant of risk of mortality in patients with ET. The researchers revisited this question in two separate cohorts; the first included 904 patients from the Mayo Clinic, and the second included 490 patients from the University of Florence in Italy. The results of the analysis were
In the Mayo Clinic patients, the median age was 58 years and 65% of the cohort was female. Based on the international prognostic score for ET (IPSET), 23% were high-risk patients, 42% were intermediate risk, and 35% were low risk.
On a multivariate analysis, several factors were significant predictors of shortened survival. This included male gender, with a hazard ratio (HR) of 1.6 (95% CI, 1.3–2.0), along with age of 60 years or older (HR, 4.3; 95% CI, 3.4–5.4) and leukocyte count of at least 11 × 109/L (HR, 1.5; 95% CI, 1.3–1.9).
The median survival of women with ET in this cohort was 20 years, compared with 14 years for men (P = .0003).
The results were similar in the University of Florence cohort, where the male gender HR was 1.6 (95% CI, 1.1–2.5), the older age HR was 4.6 (95% CI, 2.2–9.5), and the elevated leukocyte HR was 1.8 (95% CI, 1.1–2.8).
A separate analysis in the context of the IPSET categories confirmed the results. And interestingly, the importance of male gender as a risk factor was most prominent in the IPSET high-risk patients, with an HR of 2.1 (95% CI, 1.50–3.0), while it was not significant in the intermediate- and low-risk patients.
Thrombosis history was significantly associated with survival on a univariate analysis, but this significance disappeared on the multivariate analysis.
“The observations from the current study suggest that older women with ET live longer than their male counterparts and that gender might supersede thrombosis history as a risk variable for overall survival,” the authors wrote. “From a practical standpoint, the findings … suggest consideration of gender, as a risk variable, in future prognostic models for ET.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.