Use of Fluorescence Imaging During Cytoreductive Surgery Could Improve Outcomes in Ovarian Cancer
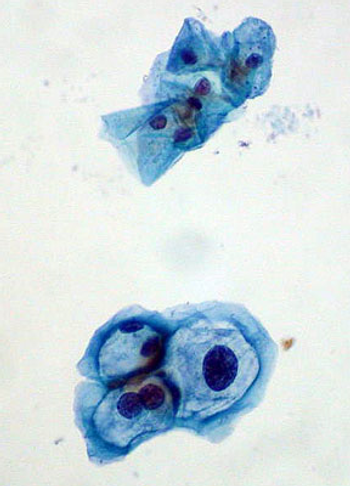
To improve staging, debulking, and prognosis in cytoreductive surgery, researchers in the Netherlands and Germany have developed a fluorescence imaging technique to visualize ovarian tumors.