A recent case report in the New England Journal of Medicine highlights the promising potentials of adoptive T-cell immunotherapy by redirecting them, through chimeric antigen receptors, as a novel and effective therapeutic modality for cancer.

Your AI-Trained Oncology Knowledge Connection!


A survey of more than 500 long-term survivors of non-Hodgkin’s lymphoma (NHL) has revealed that more than one-third experience persistent or worsening symptoms of post-traumatic stress disorder (PTSD), with nearly 4 of 10 cancer survivors stating they still experience symptoms of PTSD more than a decade after their cancer diagnosis.
A recent case report in the New England Journal of Medicine highlights the promising potentials of adoptive T-cell immunotherapy by redirecting them, through chimeric antigen receptors, as a novel and effective therapeutic modality for cancer.

The U.S. Food and Drug Administration (FDA) announced last week the approval of brentuximab vedotin, a CD30-directed antibody drug-conjugate, for the treatment of refractory Hodgkin lymphoma and systemic anaplastic large-cell lymphoma.
Equine ATG has been used for the treatment of severe aplastic anemia since the 1980s. Rabbit ATG is used in many parts of the world including South America, Japan, and European countries. The results of a randomized study of equine versus rabbit ATG showed that rabbit ATG was inferior to equine ATG.

Researchers at the University of Pennsylvania have reported on the results of a trial in which a patient with chronic lymphocytic leukemia (CLL) experienced a complete remission after immunotherapy with tumor-reactive modified T cells.
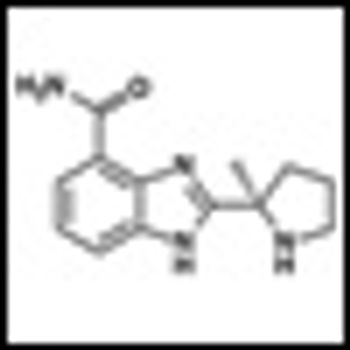
Results of a Phase I study of the novel Poly(ADP-ribose) polymerase (PARP) inhibitor veliparib (ABT-888) in solid tumors and lymphoma have just been published in Cancer Research (doi:10.1158/0008-5472.CAN-11-1227).
Researchers at the University of Chicago and colleagues have identified two variants on chromosome 6q21 that are associated with second malignant neoplasms (SMNs) in survivors of pediatric Hodgkin’s lymphoma. The SMNs are linked to radiation therapy used to treat the pediatric cancer.

There has been dramatic progress in the management of acute promyelocytic leukemia during the past three decades. Important insights into the pathogenesis of the disease have come to light and effective treatment has been developed.

Our ability to stratify patients with CLL into high-risk and low-risk categories has advanced dramatically over the past two decades. However, which test or tests are most reliable remains to be seen.

A rarely noted aspect of the era of novel agents and explosive new knowledge in the clonal plasma cell diseases is how short the half-life of relevant information has become, and how this churning has challenged clinical thinking.

In less than a decade, the resources available to treat light chain (AL) amyloidosis have increased impressively.

This review of the various available options for the treatment of systemic amyloidosis is designed to help the clinician determine which patients are candidates for stem cell transplantation and which should be treated with conventional chemotherapy.

Observation is the standard of care. However, clinical trials are ongoing to determine whether early therapy with newer agents can prolong the time to progression-and most importantly, prolong survival.

In this video interview, Joseph Connors gives an overview of the results presented here at ASCO of the phase II trial of brentuximab vedotin in patients with relapsed or refractory Hodgkin lymphoma, and discusses the most intriguing work currently being done with novel agents used to treat relapsed or refractory Hodgkin lymphoma.

Myelodysplastic syndromes, also referred to collectively as MDS, have significant biological and clinical heterogeneity, a highly variable natural history, and a complex pathobiology that is not clearly understood.

The myelodysplastic syndromes (MDS) are a heterogeneous spectrum of clonal hematopoietic diseases characterized by bone marrow hypercellularity, dysplasia of cellular elements, and consequent inadequate hematopoiesis, with resultant peripheral blood cytopenias.

The review by Dr. Akhtari outlines the diagnosis, prognosis, and treatment options for patients with myelodysplastic syndromes (MDS), and touches on the current challenges in treating patients suffering from MDS.

This review will cover the key elements of modern acute lymphoblastic leukemia treatment regimens, focusing primarily on front-line treatment and concluding with a brief discussion of the management of relapsed disease.

We have witnessed remarkable gains in the biological understanding and treatment of acute lymphoblastic leukemia (ALL) over the past decade.

About 35 years ago, I encountered several children and adolescents with acute lymphoblastic leukemia or widespread non-Hodgkin lymphoma who presented with or who developed, upon initiation of therapy, severe renal and metabolic derangements.

Computerized registry couldbe easily adopted in the U.S.,according to Italian developers. Developing a web-based registry amongcommunity oncologists may be usefulfor collecting significant informationabout febrile events in patients withhematologic malignancies.

The accurate and in-depth documentation of learning gaps is a fundamental aspect of developing continuing education activities. To obtain a better understanding of community-based medical oncology practice patterns, 43 oncologists within the United States were recruited to complete a traditional clinical case–based questionnaire and to contribute specific anonymous demographic and treatment information derived from their actual patients. This information was used to create a cross-sectional case database on two types of cancer in which major clinical advances have been reported in recent years - multiple myeloma and follicular lymphoma. These diseases also are similar in that most patients experience clinically meaningful benefits from systemic treatment but are unlikely to be cured by therapy. As further described in this and the subsequent two articles, this case-based series documents that (a) clinical research advances are being quickly implemented in daily patient care and that (b) although therapeutic strategies vary based on patient age, the short-term outcomes in terms of response to and tolerance of treatment are similar in younger and older patients.

A number of recent treatment advances in the management of follicular lymphoma (FL), including the introduction of the anti-CD20 monoclonal antibody rituximab, have effectively shifted the primary therapeutic goal away from palliation and avoidance of toxicity toward the more proactive objective of extending survival. This paper reviews recent practice patterns in the broad context of the published findings from major phase III randomized trials; it documents potential gaps between trial results and actual practice, and the implications of these for continuing education of oncologists. Forty-three US-based community oncologists participated in a cross-sectional case survey during which 40 documented their management of 186 patients with newly diagnosed FL and 133 patients with relapsed FL, all of whom were treated after January 1, 2008. The findings from this initiative indicate that the majority of these patients did not have any major symptoms at presentation. Additionally, tolerance of and response to treatment, regardless of the regimen employed, were similar across the different age groups studied (<65, 65-74, ≥75 years). Therapies selected by the physicians surveyed in both the up-front and the relapsed settings broadly corresponded to the evidence-based published literature and were supported by treatment guidelines. In addition, a change in the proportional use of bendamustine/rituximab (BR) in the up-front treatment of FL from 2008 to 2010 was observed, suggesting that community oncologists are rapidly incorporating pivotal clinical trial results when deciding on individual patient management strategies.

The management of multiple myeloma (MM) has undergone rapid change with the recent emergence of several effective novel agents that have added complexity to individualized treatment decision-making. This paper reviews the initial management of 276 patients with MM diagnosed and treated by 43 US-based community oncologists since January 1, 2008. The case survey data obtained are evaluated within the broad context of published findings from major phase III randomized trials and as such reveal potential education gaps and implications for oncology CME. Overall, the results reveal that most patients were symptomatic at diagnosis and were risk-stratified by fluorescene in situ hybridization (FISH) and/or cytogenetics. When analyzed by age, the overall symptomatology and biomarker-defined risk profiles appeared similar in the three age groups studied (

The effectiveness of RT in the palliative setting is sometimes overlooked; however, RT can provide excellent palliation for patients whose disease becomes refractory to other modalities.

Canadian researchers also find that patients are not having recommended cancer screening studies done on a regular basis.