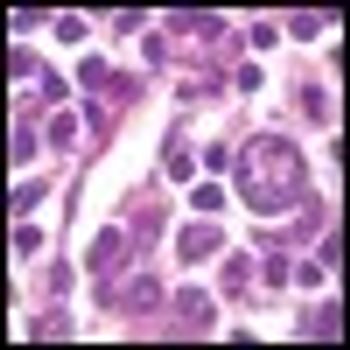
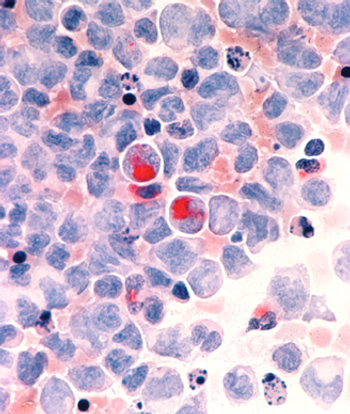
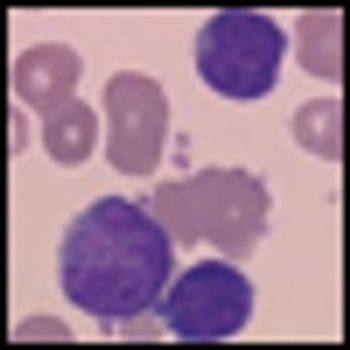
In their article in this issue of ONCOLOGY, Nastoupil, Rose, and Flowers give a very careful assessment of the options for treating diffuse large B-cell lymphoma (DLBCL), with a focus on the importance of dose density in improving outcomes in this disease.