Oncology NEWS International
- Oncology NEWS International Vol 13 No 2
- Volume 13
- Issue 2
Bexxar: Low Risk of Secondary MDS/AML
SAN DIEGO-There have been no reported cases of treatment-related myelodysplastic syndrome and acute myeloblastic leukemia (tMDS/tAML) in patients with low-grade non-Hodgkin’s lymphoma (NHL) treated initially with the Bexxar therapeutic regimen (tositumomab and iodine-131 tositumomab).
SAN DIEGOThere have been no reported cases of treatment-related myelodysplastic syndrome and acute myeloblastic leukemia (tMDS/tAML) in patients with low-grade non-Hodgkin’s lymphoma (NHL) treated initially with the Bexxar therapeutic regimen (tositumomab and iodine-131 tositumomab).
John M. Bennett, MD, Professor of Medicine, Laboratory Medicine and Pathology, Emeritus, at the University of Rochester Medical Center’s James P. Wilmot Cancer Center, presented the study at the 45th Annual Meeting of the American Society of Hematology (abstract 91).
Dr. Bennett explained that the study was an update of data presented at the ASH conference 2 years ago. The concern was that patients with low-grade NHL typically receive many cytotoxic regimens and local external-beam radiotherapy over the 8- to 12-year course of their disease, and virtually all of these agents are intrinsically carcinogenic. As a consequence, one of the potential complications of therapy is MDS and AML. Indeed, the estimated actuarial risk of tMDS/tAML associated with chemotherapy and radiotherapy at 8 years ranges from 4% to 17%.
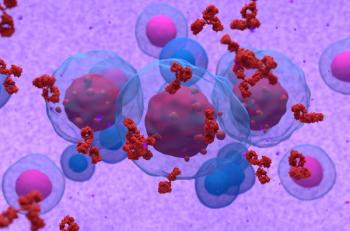
Since 1990, more than 1,500 patients with low-grade NHL have been treated with the Bexxar therapeutic regimen, which specifically targets CD20 on normal and malignant lymphocytes and delivers both gamma and beta radiation. Dr. Bennett noted that many durable long-term remissions have been reported in patients treated with the Bexxar therapeutic regimen (see article on page 13). "We investigated whether the systemic radiation from the Bexxar therapeutic regimen increases the incidence of tMDS/tAML over that observed in patients exposed to known leukemogenic agents," Dr. Bennett said.
The masked, independent review looked at 1,071 patients who were enrolled in seven studies of Bexxar therapy. Of these, 995 patients had relapsed/refractory low-grade NHL and had received a median of three prior cytotoxic regimens, including alkylating agents, platinums, topoisomerase II inhibitors, antimetabolites, and external-beam radiation therapy to greater than one marrow-bearing region. The other 76 patients had follicular NHL and received the Bexxar regimen as their initial therapy.
All patients had less than 25% bone marrow involvement. The mCi dose of the Bexxar therapeutic regimen was adjusted to deliver 65 or 75 cGy total body radiation dose depending on the patient’s pre-Bexxar platelet count (100,000 to 150,000/mm3 or more than 150,000/mm3, respectively).
Dr. Bennett reported that among 995 heavily pretreated patients, there were 35 investigator-reported cases of tMDS/tAML, with a median follow-up of 2 years. In contrast, among the 76 previously untreated patients, there have been no reported cases of tMDS/tAML, with a median follow-up of 4.6 years.
Bone Marrow Sample Review
A single-reference hematomorpholo-gist reviewed the available pre- and post-Bexxar bone marrow samples from the 35 tMDS/tAML patients in a blinded fashion. After this review, the incidence of tMDS/tAML in these Bexxar studies was reduced by 37%.
The reviewers found that two patients had no evidence of MDS with stable pre- and post-Bexxar blood counts and one had asplastic anemia before Bexxar therapy. Significantly, 9 patients were found to have tMDS in their pre-Bexxar marrow (see Figure), and 1 patient had AML (erythroleukemia).
The annualized incidence of tMDS/tAML for previously treated patients was 1.6% a year based on investigator assessments (35 cases), and 1.1% a year based on the independent hematomorpholo-gist’s assessment (22 confirmed cases).
Given the considerable variability in the incidence of tMDS/tAML in low-grade NHL patients in the literature (an average of 10% in 10 years) and the variety of statistical methods and diagnostic criteria used, Dr. Bennett said that treatment decisions must be based on risk-to-benefit ratios that are "reasonable and rational."
Articles in this issue
about 22 years ago
Adjuvant Docetaxel Bests FAC in Breast Caabout 22 years ago
Adding Rituximab to CHOP Chemo Improves DLBC Lymphoma Outcomesabout 22 years ago
BP1 Expression May Be Indicator of Early Breast Cancerabout 22 years ago
Doubling Imatinib Dose Ups CML Response RatesNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.