Oncology NEWS International
- Oncology NEWS International Vol 11 No 5
- Volume 11
- Issue 5
Current Treatment Options for Aplastic Anemia and Myelodysplastic Syndrome
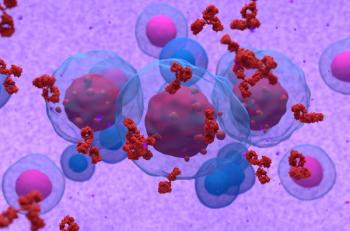
LOS ANGELES-Myelodysplastic syndrome and aplastic anemia are both diseases of bone marrow failure and are characterized by reticulocytopenic anemia, with variable neutropenia and thrombocytopenia. Other than that, the two diseases are substantially different from each other. Tools for diagnosing and managing these two complex diseases were updated by Ronald L. Paquette, MD, associate professor of medicine at the University of California Medical Center in Los Angeles
LOS ANGELESMyelodysplastic syndrome and aplastic anemia are both diseases of bone marrow failure and are characterized by reticulocytopenic anemia, with variable neutropenia and thrombocytopenia. Other than that, the two diseases are substantially different from each other. Tools for diagnosing and managing these two complex diseases were updated by Ronald L. Paquette, MD, associate professor of medicine at the University of California Medical Center in Los Angeles.
Aplastic Anemia
Patients with aplastic anemia (AA) are usually quite ill and symptomatic when they present, predominantly because of pancytopenia. They may have fatigue or dyspnea on exertion, severe infections, petechiae, purpura, and/or mucosal bleeding. These patients can have profound anemia. "It’s not uncommon for them to come in with a hemoglobin of 5 g/dL," Dr. Paquette reported.
Diagnosis is by bone marrow aspiration and biopsy. "Usually the bone marrow is nearly completely empty and no dysplastic features are seen. This is a disease that really is autoimmune in nature, with the patient’s own immune system attacking bone marrow precursors and essentially wiping them out," Dr. Paquette said.
Disease criteria are:
- absolute neutrophil count < 500/µL;
- absolute reticulocyte count < 20,000/µL; and
- platelet count < 20,000/µL.
Patients with one criterion have moderate AA; those with two criteria have severe disease; and patients with three criteria, including a neutrophil count < 200/µL, have very severe disease.
Very Effective Therapies
"Fortunately, although these patients are very sick when they come in, there are some very effective therapies for this disease," Dr. Paquette said (see Table 1).
Allogeneic bone marrow transplantation is indicated for severe or very severe cases. Retrospective studies have shown that patients younger than 20 have better survival with bone marrow transplantation than immunosuppressive therapy for initial treatment, although older patients can also be candidates. The decisions are made on a case-by-case basis.
Survival following allogeneic bone marrow transplantation ranges from 65% to 80%. One of the risks is failure of the transplanted cells to grow in the patient, which is usually associated with a high mortality. Acute grade 3/4 graft vs host disease occurs in 20% of patients and chronic graft vs host disease can be disabling and life-threatening in a small number of patients. Survivors are at risk of developing solid tumors.
Most older patients receive immunosuppressive treatment. The response rate ranges from 60% to 80% with "very excellent long-term survival,’’ Dr. Paquette noted. ‘‘Although there is a fair to moderate risk of relapse, most patients that relapse successfully respond to repeat treatment with antithymocyte globulin (ATG).’’
Salvage options are unrelated donor bone marrow transplantation and a second course of horse ATG/cyclosporine (Neoral, Sandimmune). Some patients respond to cyclosporine alone. Hematopoietic growth factors can be used as adjunct treatment in patients with severe neutropenia and recurrent infections.
A study of unrelated donor bone marrow transplantation had 2-year survival of 57%. Patients younger than 20 and transplanted less than 1 year from time of diagnosis fared better than other patients. "So those patients who are real candidates for unrelated transplantation should be identified early and brought to transplantation, rather than waiting and hoping that they may recover with ongoing rounds of immunosuppression," Dr. Paquette noted.
Myelodysplastic Syndrome
Myelodysplastic syndrome (MDS) is characterized by depressed peripheral blood counts and ineffective hematopoiesis. Patients usually have a hypercellular bone marrow.
Patients can present with symptoms similar to aplastic anemia, including fatigue and dyspnea on exertion, or MDS may be detected by a routine blood count. Laboratory findings include reticulocytopenic anemia, sometimes with neutropenia and thrombocytopenia. The anemia may be macrocytic, normocytic, or microcytic. "In those patients with macrocytic anemia, it is important to rule out other causes of megaloblastic anemias," Dr. Paquette said.
Infection usually occurs later in the disease course. Petechiae, purpura, and mucosal bleeding may be indications of thrombocytopenia and more advanced MDS.
Treatment Trials
Transplantation is rarely used for MDS because most patients with this disease are elderly. A transplantation study done in Seattle found that age and number of blasts are important prognostic factors. When MDS does occur among those under 40, the survival rate is about 50%, whereas older patients have a poorer prognosis.
Patients who have increased number of blasts have high risk disease that could make them a candidate for transplant, but also have a high relapse rate after transplant. "Half the patients with some increased number of blasts will relapse in spite of the transplant, whereas those patients who have normal or a relatively normal number of blasts will typically be cured of their disease," Dr. Paquette reported.
A Real Dilemma
"This presents a real dilemma because the patients who typically have low numbers of blasts in the bone marrow are those patients who will do very well without a transplant," Dr. Paquette said. "These are the patients with either low or intermediate risk disease. If you transplant these patients, there is a substantial risk of the patient dying from the transplant. Even if there’s a chance of a cure, you may be shortening their lives."
The Seattle study was unable to show a survival benefit from transplantation, compared to supportive care or other treatments, for patients with low or intermediate risk disease.
"A majority of patients with myelodysplastic syndrome receive erythropoietin at some point in the course of their disease, predominantly because almost everyone is anemic and the majority of patients develop symptomatology related to anemia," Dr. Paquette said.
Meta-Analysis
In a meta-analysis of 17 trials assessing the effects of erythropoietin (EPO) among a total of 205 MDS patients, the overall response rate was only 16%. The data, however, came from older trials using very different dosing than currently used, some even administered intravenously.
Although not representative of current therapy, the meta-analysis was helpful in identifying some patients that appeared to benefit from EPO therapy more than others. Response rates were greater among patients that:
- did not have ringed sideroblasts in their bone marrow than those with ringed sideroblasts (21% vs 8%);
- were anemic but did not yet require transfusions 44% vs 10%); and
- had baseline serum erythropoietin < 200 U/L (26% vs 10%).
A subsequent study found that combining erythropoietin with low-dose filgrastim (Neupogen) enhanced the myeloid response. The 55 study participants received EPO at 100 to 300 U/kg/d plus filgrastim titrated up to achieve a normal neutrophil count or to twice the baseline for those who started with a normal count. The erythroid response was 48% and the myeloid response 96%. Baseline EPO level significantly predicted the likelihood of response.
Several trials have studied the effectiveness of filgrastim in stimulating neutrophil counts. "Most patients will respond and have a good increase in their neutrophil count," Dr. Paquette said, "but its use should be restricted to those with recurrent infections."
Experimental Treatments
Antithymocyte globulin (ATG), used to treat aplastic anemia, is being investigated for use in MDS. In a study sponsored by the National Institutes of Health, low-risk patients with less than 20% bone marrow blasts had a relatively high response rate of 41%. The responses were stable in 81% of the patients at 2 years. "Patients with refractory anemia were more likely to benefit than the other subgroups," Dr. Paquette said.
Thalidomide (Thalomid) was investigated in a University of Chicago study among 83 patients treated with 100 to 400 mg/day. "The problem was tolerance in this patient population," Dr. Paquette stated. "Elderly people tend not to tolerate thalidomide very well for extended periods of time and more than one-third of the patients dropped out of the intended 12-week treatment." Side effects include fatigue, constipation, shortness of breath, fluid retention, dizziness, rash, and peripheral neuropathy. Erythroid response did occur among 19% of the study participants, with a 31% response rate for those completing treatment."
Among newer agents with potential activity against MDS are thrombopoietic agents, such as IL-11, and tyrosine kinase inhibitors such as imatinib mesylate (Gleevec, STI571) (see Table 2, above).
Articles in this issue
almost 24 years ago
Prognosis Good for Local Recurrence After Lumpectomyalmost 24 years ago
Long-Term Use of Actiq Safe and Effective for Breakthrough Painalmost 24 years ago
Youth Exposed to Tobacco Promotionsalmost 24 years ago
Green Tea May Help Prevent Certain Gastrointestinal Cancersalmost 24 years ago
EGFR Inhibitor Effective as Salvage Therapy for NSCLCalmost 24 years ago
Targeted Filgrastim Support Allows Planned Chemotherapy Dosesalmost 24 years ago
Low Risk of CHF With Paclitaxel/Trastuzumab Adjuvant Rxalmost 24 years ago
Anxiety, Depression in Women at High Risk for Breast Canceralmost 24 years ago
NCCN Updates its Treatment Guidelines for Breast Canceralmost 24 years ago
Danny Glover ‘Acting’ as Spokesman for Anemia LifeLineNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.